Abstract
Background
Preoperative localization studies with Tc99m-sestamibi have become an integral step in the preoperative assessment of patients with primary hyperparathyroidism (PHPT). This enables scan-directed minimally invasive parathyroidectomy (MIP) to be the preferred treatment for PHPT in many units. This study aimed to identify factors that lead to negative imaging studies in patients with PHPT.
Methods
Over a 3-year period consecutive unselected patients with PHPT underwent Tc99m-sestamibi scanning and high-resolution ultrasound (US) scanning by the same radiologist. When localization studies were concordant, patients underwent MIP. Those patients with negative imaging studies underwent bilateral neck exploration. Histology slides were independently reviewed and the proportion of chief cells and oxyphil cells within each adenoma was estimated.
Results
One hundred and fifty-eight patients underwent localization studies (38 men and120 women, aged 61.8 ± 15.2 years). Sestamibi scans were negative in 52 (32%) and positive in 106 (68%) patients. There was a higher incidence of hyperplasia in the group of patients with negative sestamibi scans (4 out of 52 vs. 4 out of 103, P < 0.05, χ2 test). In patients with negative sestamibi scans the majority of adenomas were formed predominantly from chief cells (26 out of 36) while the majority of patients with adenomas composed predominantly of oxyphil cells had positive scans (21 out of 23) (P < 0.05, χ2 test). The weight of parathyroid adenomas was higher when sestamibi scans were positive (median: 1,180 vs. 517 mg, P < 0.05, Student’s t-test).
Conclusion
Successful preoperative localization of parathyroid adenomas using Tc99m-sestamibi scanning is influenced by the cytological predominance of individual tumors. Negative scans might therefore be unavoidable in a subgroup of patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Primary hyperparathyroidism (PHPT) is a common endocrine disease, with a prevalence estimated to be 21 per 1,000 population in women aged 55–75 years, which is equivalent to a 3 in 1,000 prevalence in the general population.1,2The vast majority of these patients (i.e., up to 85%) present with a single enlarged overactive parathyroid adenoma. Ever since the first successful parathyroidectomy performed by Mandl in 1925, bilateral cervical exploration has been considered the gold standard operation for PHPT. Until recently, most surgeons have subscribed to the aphorism attributed to the late Dr. Doppman that “the only localization study you need is to locate a good endocrine surgeon”3. Recently, Tc99m-sestamibi scanning has been used to improve the ability to locate parathyroid adenomas and this has led to the introduction of a scan-directed minimally invasive parathyroidectomy (MIP) technique. A recent meta-analysis involving 784 patients from 24 individual studies reported an overall sensitivity and specificity of 91% and 99% respectively for sestamibi localization of parathyroid adenomas in patients with PHPT.4
Technetium-99m methoxyisobutylisonitrile (sestamibi) was initially introduced for cardiac scintigraphy and was accidentally found to be concentrated in parathyroid adenomas.5 Sestamibi is a monovalent lipophilic cation that diffuses passively through cell membranes and accumulates almost exclusively in mitochondria following negative membrane potentials.6 The exact mechanism of its elective uptake in abnormal parathyroid glands remains debatable. High mitochondrial activity is considered to be the major component of sestamibi uptake by human parathyroid tissue in patients with PHPT.7,8 The lack of expression of P-glycoprotein (P-gp) and multidrug resistance-related protein (MRP) favors the specific uptake of sestamibi into the parathyroid glands, sestamibi imaging being negative in adenomas that express at least one of these proteins.9,10
Multiple series have reported that sestamibi scanning has a very high specificity, with very rare false-positive results. Nevertheless, sestamibi accumulates in a number of nonparathyroid tissues. Because PHPT and neoplasia coexist in some patients it is important to note that sestamibi uptake can occur in several primary carcinomas, such as breast,11 lung,12 head, and neck carcinomas, and their lymph node and osseous metastases.13 Within the neck, uptake and prolonged retention of Tc99m-sestamibi have been described in differentiated thyroid malignancies,14 primary thyroid lymphomas,15 reactive lymph nodes,16 remnant thymus,17 and enlarged submandibular salivary gland.18 Furthermore, in a patient with multiple endocrine neoplasia type I, sestamibi scanning identified a thymic carcinoid and a pituitary adenoma in addition to the enlarged parathyroid glands.19 For clinical decisions, false-positive scans can lead to unsuccessful unilateral exploration. Additionally, false-negative scans can occur with cervical adenomas and ectopic lesions and it has been estimated that at least 1 in 8 solitary parathyroid adenomas is not detected with sestamibi scanning.20
Technical improvements for sestamibi scanning have evolved in recent years. It has been shown that dual-tracer subtraction is superior to the earlier technique of double-phase washout.21 More recently, single photon emission computed tomography (SPECT) was found to further increase the sensitivity of sestamibi imaging from 87% (as in planar scintigraphy) up to 95%22. Some authors have reported that thyroid suppression with thyroxine (T4) or liothyronine (T3) may improve the yield of sestamibi imaging in patients who have an initially nonlocalizing study.23
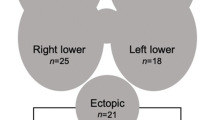
Combining sestamibi scintigraphy and high-resolution ultrasonography may increase sensitivity to 95%, the size of the adenoma influencing the efficacy of the sestamibi scans, whereas the size and position of the adenoma will influence detection with US (Fig. 1).24 A small series of 21 patients has previously been reported using a dual imaging technique.25 In our center this technique has been extensively applied in recent years because of the ability to repeat the ultrasound scan on the morning of the operation, enabling preoperative marking and facilitating precise position of the neck incision for MIP.
Imaging by sestamibi scanning and neck ultrasound in patients with primary hyperparathyroidism. A. Patient 1: ultrasound image demonstrating a left parathyroid adenoma, lying deep to the thyroid (black arrow) and confirmed on B. coronal and C. axial sestamibi scans. D. Patient 2: sagittal image from sestamibi scan demonstrating posterior mediastinal parathyroid adenomablack arrow), which was not seen on ultrasound scan (false-negative result), but was confirmed on E. coronal T1-weighted MRI scan to be a para-esophageal parathyroid adenoma (black arrow).
The aim of this study was to analyze the diagnostic accuracy of dual imaging in some 150 consecutive patients with PHPT investigated in our unit in the first 3 years after introduction of the technique, with a particular interest in the factors associated with negative imaging studies.
PATIENTS AND METHODS
Patients
From April 2001, all patients with a biochemical diagnosis of PHPT underwent preoperative localization with Tc99m-sestamibi scans and ultrasonography (US) of the neck. When the two localization studies were concordant, patients were listed for minimally invasive parathyroidectomy (MIP). Patients with negative imaging studies underwent bilateral cervical exploration. According to our established protocol for parathyroid surgery, an intravenous infusion of 5 mg/kg methylene blue in 500 ml of 5% dextrose was commenced 1 hour prior to surgery to aid intraoperative localization of the parathyroid glands.
All patients were seen in the outpatients department 4–6 weeks after surgery and assessed for symptoms and complications along with a review of the histological findings. A further follow-up appointment was organized after 1–3 years.
Imaging techniques
Sestamibi scans were performed using the single agent wash-out technique. Patients were administered with 600 MBq of Tc99m-sestamibi. Single frontal planar images were obtained at 10 and 90 minutes after isotope administration. Tc99m-sestamibi scintigraphy (SPET) images were obtained after 90 minutes. Patients were scanned using a Sopha DST-XL gamma camera (General Electric) with a low-energy, high-resolution parallel collimator and images were obtained with a 256 × 256 matrix.
Ultrasound scans were performed by a single experienced operator using a small footprint high-resolution 15-MHz linear array probe (Sequoia; Acuson, Mountain View, CA, USA).
Histology Data
All specimens were measured and weighed using laboratory scales. Slides were reviewed by two consultant histopathologists with a special interest in endocrine pathology. In particular, the proportion of chief cells and oxyphil cells within each adenoma was estimated by reviewing at least ten fields on medium-power optical microscopy.
Statistical Analysis
Data are presented as mean ± standard deviation (range). Unpaired Student’s t-test and χ2 test were used.
RESULTS
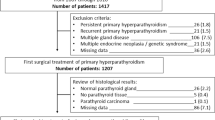
Between June 2001 and December 2004, a total of 158 patients with a biochemical diagnosis of PHPT underwent dual imaging with sestamibi scanning and high resolution ultrasound scanning. Unilateral uptake suggestive of a parathyroid adenoma was demonstrated in 103 patients. In 3 patients sestamibi scans showed bilateral uptake and during parathyroidectomy double adenomas were found in 2 patients, while the third patient had an adenoma and a normal gland. Sestamibi scans were negative in 52 patients. There was no difference between the demographic characteristics of patients with positive or negative sestamibi scans (Table 1). There was a trend toward more severe hypercalcemia and higher parathyroid hormone (PTH) levels in patients with positive sestamibi scans (Table 1).
During neck exploration, a single parathyroid adenoma was found in 97 out of 103 patients with positive sestamibi scans and in 45 out of 52 patients with negative scans (Table 2). There was a higher incidence of hyperplasia (4 out of 52 vs. 4 out of 103, P < 0.05, χ2 test) and more negative neck explorations (3 out of 52 vs. 1 out of 103) in the group of patients with negative sestamibi scans.
The weight and volume of adenomas in patients with positive sestamibi scans were significantly larger (Table 2). However, 3 out of 6 microadenomas (i.e. adenomas < 100 mg) were identified by sestamibi scans and some large adenomas were missed, suggesting that the weight and volume of the adenomas are not the only predictors of positive imaging results.
Histological analysis of 122 parathyroid adenomas revealed a significant difference in the cellular predominance in each group (Fig. 2; Table 2). A positive sestamibi scan was obtained in the vast majority of patients with adenomas formed predominantly by oxyphil cells (21 out of 23, 91%) and the majority of patients with adenomas formed by a mixed cell population (23 out of 31, 74%). When adenomas were formed predominantly of chief cells, sestamibi scans were negative in 26 out of 68 patients (38%).
Of the 103 patients with positive sestamibi scans, 92 patients had a positive ultrasound scan and such patients were offered minimally invasive parathyroidectomy (Table 3). Seven of the 11 patients with negative US had adenomas in a retrosternal position, presumed to be superior parathyroid adenomas that had migrated in front of the prevertebral plane toward the posterior mediastinum. These were large adenomas (mean weight: 1,085 mg, range 290–2,800 mg) and therefore it was the anatomical position rather than the size of these adenomas that limited the ability of US to locate them accurately. Interestingly, in the group of patients with negative sestamibi scans the position of the parathyroid adenoma was correctly identified by US in 10 patients with adenomas measuring between 75 and 700 mg (mean: 400 mg).
DISCUSSION
This paper reports on the efficacy of preoperative localization studies in 158 unselected consecutive patients with primary hyperparathyroidism (PHPT). Similar to other series previously published, it was found that SPET and high-resolution ultrasound scanning of the neck can accurately identify the position of a single parathyroid adenoma in approximately two-thirds of unselected patients (92 out of 158, 59%). Such patients can then undergo scan-directed minimally invasive parathyroidectomy. Using a similar preoperative imaging protocol others reported an overall sensitivity of 78%, which allowed a unilateral approach in 43% of the patients.26
Analysis of the factors associated with unsuccessful localization studies, confirms the trend to be able to detect larger glands and that the sensitivity of parathyroid scanning grossly correlates with weight. Based on such data, some authors suggest that there is little benefit in preoperative imaging, as small tumors will not be detected preoperatively and large tumors are easy to find at surgery. Nevertheless, more recent reports describe positive sestamibi scans for adenomas weighing less than 200 mg and this is confirmed in our series of adenomas of less than 200 mg (range: 55–200 mg) detected in 5 patients.
Perhaps more importantly we have confirmed that an abundance of oxyphil cells increases the likelihood of a positive Tc99m-sestamibi scan. Histologically, one can identify several types of cells within parathyroid adenomas.27 Chief cells are the predominant and normally the active endocrine cells, with slightly eosinophilic cytoplasm containing few mitochondria. The oxyphil cells have an intensely eosinophilic cytoplasm rich with numerous and tightly packed mitochondria. Clear cells with foamy, water-clear cell cytoplasm are fundamentally inactive cells with an unknown function. These cell types are considered to represent different stages in the life cycle of parathyroid cells and may therefore change over time. A variable mixture of these cells is seen in most parathyroid adenomas. In this study, two independent observers estimated the predominant type of cell in 122 adenomas. We found that positive sestamibi scans were more likely when adenomas had an abundance of oxyphil cells rather than in adenomas with a predominance of chief cells (i.e., a scarcity of oxyphil cells; 44 out of 54 vs. 42 out of 68, P = 0.002 χ2-test; Table 2).
Soon after the introduction of sestamibi scanning, some authors reported that positive scans are more likely if there is an abundance of oxyphil cells within the parathyroid adenomas28 and that sestamibi imaging was always negative if no oxyphil cells were present within a parathyroid adenoma,29 but these findings were not universally accepted.30–32 This question was readdressed in two recent large studies. In a group of 103 consecutive patients, it was found that positive scans were more likely to be associated with a higher percentage of oxyphil cells.33 Others randomly selected 40 adenomas from 98 patients with PHPT and found that parathyroid adenomas with greater than 25% oxyphil content were more likely to have a positive sestamibi scan result.34 In this context, our study is the largest series showing that individual histological characteristics of parathyroid adenomas can influence the likelihood of positive preoperative localization studies.
Failure of detection by sestamibi may not be critical as 12 patients with a negative sestamibi scan had their adenoma identified by US, suggesting that a skilled ultrasonographer can successfully locate small parathyroid adenomas even in the absence of guidance from a sestamibi scan. Despite such encouraging experience, it remains our practice to offer minimally invasive parathyroidectomy only to patients with concordant imaging studies.
The majority of patients with a positive sestamibi scan but a negative ultrasound scan had adenomas located in the posterior mediastinum. These patients underwent bilateral neck exploration and in 7 out of 10 patients the adenomas were found in the caudal cervical compartment or the posterior mediastinum. Based on the origin of their vascular pedicle, it was considered that such adenomas were derived from the superior parathyroid glands and had moved along the paravertebral plane.
Minimally invasive parathyroidectomy was only performed when both preoperative localization tests were concordant. Additionally, we used intraoperative methylene blue to facilitate rapid identification of the parathyroid adenomas at surgery. Although no formal record was made of the intensity of blue staining of individual adenomas, we found this adjunct to be helpful in the vast majority of cases by confirming that the “structure” dissected at the site marked by preoperative ultrasound does indeed correspond to a parathyroid adenoma. A similar protocol has been reported to be helpful during radio-guided MIP.35 Having used three methods to identify a parathyroid adenoma, we considered that intraoperative PTH monitoring is not needed to confirm the excision of overactive parathyroid tissue. Using this protocol we have achieved satisfactory success rates and a long-term cure for patients with PHPT offered MIP without intraoperative PTH monitoring (personal data, manuscript in preparation). Similar results were reported in a study from France, in which MIP performed without intraoperative confirmation studies in 45 patients had a success rate of 91.7%.36 Furthermore, a very recent series from the Mayo Clinic reported that patients with PHPT and an unequivocally positive preoperative sestamibi scan can safely and successfully be managed with focused unilateral cervical exploration without either intraoperative PTH monitoring or the use of the gamma probe.37
In conclusion, our study reports that successful preoperative localization of parathyroid adenomas using SPET is influenced by the cytological predominance of individual tumors. Although SPET is influenced by the weight and volume of the adenoma, it may still be successful in identifying microadenomas.
The clinical implications for the management of patients with PHPT is that the likelihood of being offered scan-directed unilateral neck exploration (minimally invasive parathyroidectomy) depends on whether or not the patient harbors a parathyroid adenoma with an abundance of oxyphil cells. A false-negative sestamibi scan remains either unavoidable or highly likely in the subgroup of patients with an adenoma formed predominantly of chief cells.
References
Adami S, Marcocci C, Gatti D. Epidemiology of primary hyperparathyroidism in Europe. J Bone Miner Res 2002;17(Suppl 2):N18–N23
Melton LJ III. Epidemiology of primary hyperparathyroidism. J Bone Miner Res 1991;6(Suppl 2):S25–S30
Doppman J. Reoperative parathyroid surgery: localization procedures, parathyroid surgery. Prog Surg 1986;18:117
Denham DW, Norman J. Cost-effectiveness of preoperative sestamibi scan for primary hyperparathyroidism is dependent solely upon the surgeon’s choice of operative procedure. J Am Coll Surg 1998;186:293–305
Coackley AJ, Kettle AG, Wells CP, et al. 99Tc-sestamibi: a new agent for parathyroid imaging. Nucl Med Commun 1989;10:791–794
Arbab AS, Koizumi K, Toyama K, et al. Uptake of technetium-99m-tetrofosmin, technetium-99, -MIBI and thalium-201 in tumour cell lines. J Nucl Med 1996;37:1551–1556
Hetrakul N, Civelek AC, Sragg CA, et al. In vitro accumulation of technetium-99m-sestamibi in human parathyroid mitochondria. Surgery 2001;130:1011–1018
O’Doherty MJ, Kettle AG, Wells P, et al. Parathyroid imaging with technetium-99m-sestamibi: preoperative localization and tissue uptake studies. J Nucl Med 1992;33:313–318
Kao A, Shiau YC, Tsai SC, et al. Technetium-99m methoxyisobutylisonitrile imaging for parathyroid adenoma: relationship to P-glycoprotein or multidrug resistance-related protein expression. Eur J Nucl Med Mol Imaging 2002;29:1012–1015
Sun SS, Shiau YC, Lin CC, et al. Correlation between P-glycoprotein (P-gp) expression in parathyroid and Tc-99m-MIBI parathyroid image finding. Nucl Med Biol 2001;28:929–933
Taillefer R, Robidoux A, Lambert R, et al. Technetium-99m-sestamibi prone scintimammography to detect primary breast cancer and axillary lymph node involvement. J Nucl Med 1995;36:1758–1765
Yen TC, Tzen KY, Lee CM, et al. Squamous cell carcinoma of the lung mimicking an ectopic mediastinal parathyroid adenoma demonstrated by Tc-99m sestamibi in a hypercalcaemic patient. Clin Nucl Med 1999; 24:895–896
Glaser C, Pruckmayer M, Staudenherz A, et al. Utility of technetium-99m-sestamibi to assess osseous tumour spread. J Nucl Med 1996;37:1526–1528
Kos WGM, Brown MR, Balfour JF. A false-positive localization of parathyroid adenoma with technetium Tc99m-sestamibi secondary to a thyroid follicular carcinoma. Arch Surg 1996;131:216–217
Scott AM, Kostakoglu L, O’Brien JP, et al. Comparison of technetium-99m-MIBI and thalium-201-chloride uptake in primary thyroid lymphoma. J Nucl Med 1992;33:1396–1398
Leslie WD, Riese KT, Mohamed C. Sestamibi retention in reactive lymph node hyperplasia: a cause of false-positive parathyroid localisation. Clin Nucl Med 2000;25:216–217
Mudun A, Kocak M, Unal S, Cantez S, et al. Tc99m MIBI accumulation in remnant thymus: a cause of false-positive interpretation in parathyroid imaging. Clin Nucl Med 1995;20:379–380
Campeau RJ, Reuther WL, Wayne J. False-positive Tc99m sestamibi examination for parathyroid adenoma in a case of asymmetrical salivary gland enlargement. Clin Nucl Med 1999;24:723–724
Perez-Monte JE, Brown ML, Clarke MR, et al. Parathyroid hyperplasia, thymic carcinoid and pituitary adenoma detected with technetium 99m-MIBI in MEN type I. J Nucl Med 1997;38:1767–1769
Pattou F, Huglo D, Proye C. Radionuclide scanning in parathyroid diseases. Br J Surg 1998;85:1605–1616
Leslie WD, Dupont JO, Bybel B, et al. Parathyroid (99m)Tc-sestamibi scintigraphy: dual tracer subtraction is superior to double-phase washout. Eur J Nucl Med Mol Imaging 2002;29:1566–1570
Moka D, Voth E, Dietlein M, et al. Technetium 99m-MIBI-SPECT: a highly sensitive diagnostic tool for localization of parathyroid adenomas. Surgery 2000;128:29–35
Royal RE, Delpassand ES, Shapiro SE, et al. Improving the yield of preoperative localisation: technetium Tc 99m-sestamibi imaging after thyroid suppression. Surgery 2002;132:968–975
Lumachi F, Zucchetta P, Marzola MC, et al. Advantages of combined technetium-99m-sestamibi scintigraphy and high-resolution ultrasonography in parathyroid localization: comparative study in 91 patients with primary hyperparathyroidism. Eur J Endocrinol 2000;143:755–760
Casara D, Rubello D, Piotto A, et al. (99m)Tc-MIBI radio-guided minimally invasive parathyroid surgery planned on the basis of preoperative combined (99m)Tc-pertechnetate/(99m)TC-MIBI and ultrasound imaging protocol. Eur J Nucl Med 2000;27:1300–1304
Purcell GP, Dirbas FM, Jeffrey RB, et al. Parathyroid localization with high-resolution ultrasound and technetium Tc99m-sestamibi. Arch Surg 1999;134:824–830
DeLellis RA. Surgical pathology of the parathyroid glands. In Randolph G, editor, Surgery of the Thyroid and Parathyroid Glands, St. Louis, MI, Elsevier, 2003;571–577
Melloul M, Paz A, Koren R, Cytron S, et al. (99m)-TC-MIBI scintigraphy of parathyroid adenomas and its relation to tumour size and oxyphil cell abundance. Eur J Nucl Med 2001;28:209–213
Carpentier A, Jeannotte S, Verreault J, et al. Preoperative localization of parathyroid lesions in hyperparathyroidism: relationship between technetium 99m-MIBI uptake and oxyphil cell content. J Nucl Med 1998;39(8):1441–1444
Staudenherz A, Abela C, Niederle B, et al. Comparison and histopathological correlation of three parathyroid imaging methods in a population with a high prevalence of concomitant thyroid disease. Eur J Nucl Med 1997;24:143–149
Bhatnagar A, Vezza PR, Bryan JA, et al. Technetium 99m-sestamibi parathyroid scintigraphy: effect of P-glycoprotein, histology and tumour size on detectability. J Nucl Med 1998;39:1617–1620
Ugur O, Bozkurt MF, Hamaloglu E, et al. Clinicopathologic and radiopharmacokinetic factors affecting gamma-probe-guided parathyroidectomy. Arch Surg 2004;139:1175–1179
Westreich RW, Brandwein M, Mechanick JI, et al. Preoperative parathyroid localization: correlating false-negative technetium-99m-sestamibi scans with parathyroid disease. Laryngoscope 2003;113:567–572
Mehta NY, Ruda JM, Kapadia S, et al. Relationship of technetium-99m sestamibi scans to histopathological features of hyperfunctioning parathyroid tissue. Arch Otol Head Neck Surg 2005;131:493–498
Flynn MB, Bumpous JM, Schill K, et al. Minimally invasive radioguided parathyroidectomy. J Am Coll Surg 2000;191:24–31
Saint Marc O, Cogliandolo A, Pidoto RR, et al. Prospective evaluation of ultrasonography plus MIBI scintigraphy in selecting patients with primary hyperparathyroidism for unilateral neck exploration under local anaesthesia. Am J Surg 2004;187:388–393
Jacobson SR, van Heerden JA, Farley DR, et al. Focused cervical exploration for primary hyperparathyroidism without intraoperative parathyroid hormone monitoring or use of the gamma probe. World J Surg 2004;28:1127–1131
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mihai, R., Gleeson, F., Buley, I.D. et al. Negative Imaging Studies for Primary Hyperparathyroidism Are Unavoidable: Correlation of Sestamibi and High-Resolution Ultrasound Scanning with Histological Analysis in 150 Patients. World J. Surg. 30, 697–704 (2006). https://doi.org/10.1007/s00268-005-0338-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0338-9