Abstract
Background
The impact of viral background on long-term effectiveness of different treatment modalities for recurrent hepatocellular carcinoma (HCC) was not fully analyzed.
Method
Consecutive 726 patients who developed intrahepatic recurrence after primary hepatectomy for HCC between 2008 and 2015 were retrospectively studied. Post-recurrence survival (PRS) and rerecurrence-free survival (R-RFS) and risk factors were analyzed.
Results
After a median follow-up period of 56 months, the 5-year PRS rates of the patients who underwent rehepatectomy, radiofrequency ablation (RFA), and transarterial chemoembolization (TACE) were 79.4%, 83.0%, and 54.6%, respectively. The treatment benefit for PRS was consistently observed in patients with hepatitis B virus (HBV) and non-B, non-C subgroups, but not hepatitis C virus (HCV). For patients with late recurrence of HCC, R-RFS was superior in HBV subgroup and HCV subgroup which received antiviral treatment (compared to naïve HCV subgroup). Survival difference triaged by viral status was lost in the counterpart with early recurrence. Overall, RFA improved PRS and R-RFS in patients receiving antiviral treatment.
Conclusion
To achieve long-term survival after HCC recurrence, rehepatectomy and RFA were comparably effective, particularly among those with HBV. Antiviral treatment complemented survivals of patients with HCV after RFA, particularly in late first recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the sixth most commonly diagnosed cancer and third leading cause of cancer death worldwide.1 The majority of HCC cases are related to chronic liver disease, approximately 80% of which are associated with hepatitis B or C virus (HBV or HCV) worldwide.2 Other non-viral factors, such as nonalcoholic fatty liver disease (NAFLD), are becoming increasingly relevant in the epidemiology of HCC.3
Hepatectomy remains the mainstay of treatment for resectable HCC in Asian countries, where deceased donor liver transplantation is limited.4 Recurrence of HCC is common: 60% to 80% of patients develop recurrence within 5 years,5 80% of whom develop intrahepatic recurrence.6 Intrahepatic recurrence can be categorized as early recurrence (< 1 year or 2 years), resulting from micrometastasis, and late recurrence (> 1–2 years), which results from de novo carcinogenesis.7 To date, no effective adjuvant therapies that provide survival benefit for HCC patients have been developed, and molecular testing for prognosis after hepatectomy remains suboptimal.8 Recurrence management strategies are based on each patient’s recurrence pattern and liver function, and the treatment algorithm applied is the same as for primary HCC.9 Recently, the Barcelona Clinic Liver Cancer (BCLC) guidelines were updated to integrate the concept of treatment stage migration, which accounts for the possibility of tumor downstaging after initial management.10 Effective local treatments for recurrent HCC, including rehepatectomy, radiofrequency ablation (RFA), and transarterial chemoembolization (TACE), can improve patients’ chances of long-term survival and downstaging.
The implications of the complexity of the effects of viral hepatitis on the liver and the unique immune landscapes and tumor microenvironments of patients’ livers for the potential effectiveness of immunotherapies have inspired extensive research.11 With emerging combinations of immunotherapy and targeted therapy and the identification of accurate prognostic markers, HCC management strategies have advanced considerably.
Previously, we analyzed the short-term survival outcomes among patients who receive different treatments for recurrent HCC after primary hepatectomy;12 the survival rates of the patients who underwent rehepatectomy and RFA were higher than those who underwent TACE and similar to those who underwent primary resection without recurrence. Although the survival outcomes in patients with recurrent HCC have improved over the years, the potential relationships between survival outcomes and liver background among patients with recurrent HCC have not been thoroughly researched.
We aimed to investigate the comparative effectiveness of treatment modalities for recurrent HCC and their interrelationship with viral status, together considering oncological characteristics, in the long term after recurrence. Specifically, we analyzed the long-term survival and recurrence outcomes in patients treated for recurrent intrahepatic HCC after primary hepatectomy and their potential relationship with liver background.
Methods
Patients
We retrospectively reviewed the data of consecutive Taiwanese patients who underwent primary hepatectomy for HCC at the National Taiwan University Hospital between January 2008 and December 2015. Patients who developed recurrence before the end of the follow-up period in July 2021 were included in this study. We reviewed and compared the treatments the patients received for recurrent HCC as well as the patients’ viral hepatitis profiles. This study was approved by the Ethics Committee of the National Taiwan University Hospital (202111080RINB) in accordance with all relevant guidelines.
Antiviral Treatment Policy for HBV and HCV
Since the nationwide reimbursement program of antiviral therapy for patients with HBV were launched in 2003, interferon and nucleotide analogue–based therapies were given for patients with cirrhosis, chronic hepatitis B (high serum HBV DNA ≥ 20,000 IU/mL and ≥ 2000 IU/mL for hepatitis B e antigen (HBeAg)-negative patients), and a persistently elevated serum alanine aminotransferase (ALT) level (≥ 2 times upper normal limit) for non-cirrhotic patients,12,13 or after curative treatment for HCC. Patients with anti-HCV seropositivity were evaluated for interferon therapy (with ribavirin) if observed to have elevated serum ALT levels and no hepatic decompensation since 2003 and for direct-acting agents (DAAs) if presence of HCV viremia regardless of liver fibrosis status and genotype since 2017 can be observed.14,15
Primary Hepatectomy, Follow-Up, and Recurrence Management
All the patients had undergone hepatectomy for primary HCC; the treatment strategy and procedures were as previously described.16,17 Each treatment decision was audited by a multidisciplinary liver tumor board in cases of newly diagnosed or recurrent HCC.18
The patients were followed regularly after primary hepatectomy. The patients’ laboratory data (liver function panels and alpha fetoprotein (AFP) levels) and abdominal ultrasound images were collected and reviewed every 3 months. Additional imaging studies (dynamic contrast computed tomography or magnetic resonance imaging) were arranged in cases of suspected recurrence. Tumor recurrence was defined as the appearance of a new lesion detected through imaging with a typical radiological pattern of HCC. Early recurrence was defined as recurrence within 12 months after treatment for primary or recurrent HCC.19
When intrahepatic recurrence developed, management strategy and decision making were the same as those used in the treatment of primary HCC, as previously described.9,20,21 First, patients were evaluated for operative rehepatectomy. The evaluation protocol and selection criteria have been described in a previous report.20 Patients whose recurrent HCC lesions were not more than 5 cm in diameter and accessible for percutaneous RFA and in whom rehepatectomy would be risky were treated with RFA.9 Patients who did not fulfill the aforementioned criteria underwent TACE if the serum total bilirubin level was < 2 mg/dL.9
Variables
We collected each patient’s data, including their age at primary hepatectomy, sex, family history of HCC, viral hepatitis profile (HBV, positive for hepatitis B surface antigen (HBsAg); HCV, positive for anti-HCV antibodies; HBV and HCV, or non-B, non-C), and laboratory data and tumor characteristics, including serum albumin and total bilirubin levels, albumin–bilirubin (ALBI) score,22 indocyanine green retention rate at 15 min after administration (ICG-R15), serum AFP levels, type of hepatectomy (major or minimally invasive), and tumor characteristics (number, largest tumor diameter, lobular distribution, tumor differentiation, pathological microvascular invasion, free margin, presence of liver cirrhosis, and fit to University of San Francisco (UCSF) criteria), at primary HCC diagnosis and at recurrence.
Survival Outcomes
The primary outcomes were post-recurrence survival (PRS) and rerecurrence-free survival (R-RFS) after diagnosis of first HCC recurrence. PRS was calculated from the time of first HCC recurrence to death or end of follow-up (July 2021), and R-RFS was calculated from the time of first HCC recurrence to the time of second recurrence. The patients were categorized according to the treatment they received for recurrent HCC, their viral profiles, and whether they developed rerecurrence after first recurrence.
Statistical Analyses
Categorical data are presented herein as counts and percentages; continuous data are expressed as means with standard deviations. Statistical comparisons for significance were performed using the chi-square test or Fisher’s exact test, as appropriate. PRS and R-RFS were measured using the Kaplan–Meier method and compared using a log-rank test. Cox’s proportional hazards model was used for multivariate analysis to identify significant prognostic factors. The univariate and multivariate hazard ratios (HRs) for risk factors for PRS and R-RFS were determined and are herein reported with 95% CIs. Sensitivity analysis was employed to patients with HCC recurrence within USCF criteria. All variables with P values of < 0.10 were included in the final multivariate model. A P value of < 0.05 was considered significant. All the statistical analyses were performed using SPSS v.26 (IBM, Armonk, NY, USA).
Results
Demographic Characteristics
A total of 1619 consecutive patients underwent primary hepatectomy for HCC. Among them, 952 developed HCC recurrence, and 667 did not. Among the patients with recurrence, 152 (16%) developed extrahepatic recurrence (88 of which developed concurrent intrahepatic recurrence), and 800 (84.0%) developed intrahepatic recurrence (Fig. 1A). Patients who received systemic therapy (n = 17) and supportive care (n = 57) for intrahepatic recurrence were excluded. Seven hundred and twenty-six patients (76.3%) underwent rehepatectomy (n = 107), RFA (n = 387), or TACE (n = 232) for recurrent HCC and were further analyzed (Fig. 1B).
Patient selection (A, B) and survivals after first recurrence (C, D). A Flowchart and B Sankey diagram of development of first hepatocellular carcinoma (HCC) recurrence and subsequent rerecurrence after primary hepatectomy. Survival curves comparing post-recurrence survival (PRS) (C) and rerecurrence-free survival (R-RFS) (D) of patients who underwent rehepatectomy, radiofrequency ablation (RFA), and transarterial chemoembolization (TACE) for first HCC recurrence
The clinicopathological characteristics of the 726 patients are summarized in Tables 1 and 2. The mean age at primary HCC diagnosis was 61.5 ± 11.8 years. Most (75.1%) of the patients were men. Regarding hepatitis viral infection status, 433 (59.6%) of patients had HBV, 153 (21.1%) had HCV, 30 (4.1%) had HBV and HCV, and 110 (15.2%) were non-B, non-C. Nearly half (48.8%) of the patients had liver cirrhosis, and 256 (35.3%) had AFP > 100 ng/mL. The mean ALBI score and ICG R-15 were − 3.04 and 11.3%, respectively. The mean primary HCC tumor size was 4.8 ± 3.8 cm. Most of the tumors were within the UCSF criteria (70.9%) and had high pathological grades (> 2; 67.8%).
Among the patients, 258 (35.5%) developed early recurrence, 317 (43.7%) had multiple tumors, and 163 (22.5%) had R-AFP > 100 ng/mL. Most (77.7%) recurrent HCC tumors were within the UCSF criteria. The mean recurrent tumor size, R-ALBI score, and R-ICG R-15 were 2.6 ± 1.8 cm, − 2.84, and 10.8%, respectively. After receiving treatment for HCC recurrence, 506 (69.7%) patients developed intrahepatic rerecurrence.
Treatments for Intrahepatic HCC Recurrence
Table 1 presents a comparison of the 3 treatment groups (with 107, 387, and 232 patients in the rehepatectomy, RFA, and TACE groups, respectively). The patients who underwent rehepatectomy were generally younger. The patients who underwent RFA generally had higher ICG R-15 values at both primary HCC diagnosis and first recurrence and had smaller recurrent tumors. Most of the patients who underwent rehepatectomy (93.5%) and RFA (94.3%) had recurrent tumors within the UCSF criteria.
Compared with the rehepatectomy and RFA groups, the TACE group had a larger primary tumor and larger proportions of patients with multiple tumors, tumors beyond the UCSF criteria, and microvascular invasion, and a larger proportion had undergone major hepatectomy for primary HCC. Compared with the rehepatectomy and RFA groups, at first recurrence, the TACE group had higher total serum bilirubin, lower serum albumin, and a higher ALBI score and number of recurrent tumors as well as greater proportions of patients with AFP > 100 ng/mL, multiple and bilateral tumors, and tumors beyond the UCSF criteria. Most of the patients in the TACE group (211/232, 91%) developed intrahepatic rerecurrence (all P < 0.05).
Survival Outcomes (PRS and R-RFS) After Intrahepatic HCC Recurrence
Over a median follow-up period of 56.0 months, the 5-year and 10-year PRS rates were 73.8% and 56.5%, respectively. The 1-year, 3-year, 5-year, and 7-year PRS rates were 98.1%, 86.6%, 79.4%, and 74.6%, respectively, in the rehepatectomy group; 98.6%, 90.7%, 83.0%, and 76.1%, respectively, in the RFA group; and 86.2%, 65.2%, 54.6%, and 49.7%, respectively, in the TACE group. The PRS rates of the rehepatectomy and RFA groups did not differ significantly (P = 0.779), and both were higher than those in the TACE group (P < 0.001, Fig. 1C).
After treatment for first intrahepatic recurrence, 556 (76.5%) of the patients developed rerecurrence, 506 (91.0%) and 50 (9.0%) of whom developed intrahepatic and extrahepatic rerecurrence, respectively. The median R-RFS duration was 12.0 months. The 1-year, 3-year, and 5-year R-RFS rates were 69.3%, 41.9%, and 29.9%, respectively, in the rehepatectomy group; 64.3%, 34.7%, and 22.1%, respectively, in the RFA group; and 17.8%, 7.1%, and 3.5%, respectively, in the TACE group. The R-RFS rates in the rehepatectomy and RFA groups did not differ significantly (P = 0.107) and were higher than those in the TACE group (P < 0.001, Fig. 1D).
Although the RFA group had higher average age and more patients with liver cirrhosis, microvascular invasion, and multiple recurrent tumors compared with the rehepatectomy group, the PRS and R-RFS rates of the groups were similar. The intrahepatic rerecurrence rates of the rehepatectomy and RFA groups were also comparable (57.9% vs 65.9%, P = 0.306).
Viral Status Stratification and Interrelation with Treatment Modalities for Intrahepatic HCC Recurrence
Because patients were regularly followed after recurrence, flare-up events of hepatitis were rare. Three patients had HBV flare-up after HCC recurrence. Two had received interferon treatment before the diagnosis of primary HCC. They had HCC recurrence 20 months and 28 months after primary resection and HBV flare-up 16 months and 39 months after recurrence, respectively. Both died of subsequent liver failure. The third patient had HBV flare-up 24 months after recurrence due to discontinuation of entecavir for 3 months. The episode was subsided after resuming entecavir treatment. No events of death or active hepatitis related to HCV were documented.
Triaged by viral status, demographics of patients with recurrent HCC after different treatments are shown in Table 2. Notably, patients with HBV were younger, more with family history of HCC and had higher AFP level; patients with HCV had lower serum albumin and higher ALBI score when recurrence developed; non-B, non-C patients had larger initial tumor, and more of them received primary major resection; when recurrence developed, the tumor was larger and more presented with multiple tumors (all P < 0.05). The 5-year PRS rates were comparable in patients with either HBV or HCV (P = 0.822), while the R-RFS rates of the patients with HBV were higher than those with HCV (P = 0.032, Fig. 2A).
Survivals (PRS and R-RFS) in HBV or HCV patients with HCC recurrence after primary resection (A). Survival curves comparing PRS (B) and R-RFS (C) of patients who underwent rehepatectomy, RFA, and TACE for first HCC recurrence, stratified by viral status (i.e., HBV, HCV, HBV&HCV, and non-B, non-C). HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; PRS, post-recurrence survival; RFA, radiofrequency ablation; R-RFS, rerecurrence-free survival; TACE, transarterial chemoembolization
The 5-year PRS rates of patients with HBV who underwent rehepatectomy and RFA were comparable (79.9% vs 86.1%, P = 0.448) and were both higher than those patients with HBV who underwent TACE (54.3%, P < 0.001, respectively), whereas among the patients with HCV and those with HBV and HCV, the parallel significance was lost among the 3 treatment groups. Among the non-B, non-C patients, only RFA provided higher 5-year PRS rate than TACE (71.6% vs 47.1%, P = 0.038, Fig. 2B). The R-RFS rates of the patients who underwent rehepatectomy and RFA were higher than those who underwent TACE regardless of the patients’ viral profiles (all P < 0.05, Fig. 2C).
Comparative Outcomes in Recurrent HCC Subgroups: HCV with Antiviral Treatment, Naïve HCV, and HBV (as Benchmark Reference)
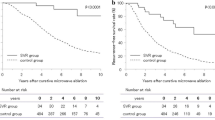
We tried to determine whether antiviral treatment for HCV affected survival outcome for recurrence HCC. We identified 81 patients who received antiviral treatment for HCV (Supplementary Table S3). These patients who received antiviral treatment had better PRS and R-RFS than those without (P < 0.001 and 0.004, respectively) and was comparable to survival outcomes in patients with HBV (P = 0.095 and 0.931, respectively, Fig. 3A, B). For HCV patients who received different treatments for recurrent HCC, although patients who received antiviral treatment had better PRS and R-RFS in all treatment modalities, no statistical significance was reached except in PRS of patients who received RFA (P = 0.014) and R-RFS (borderline significance) (P = 0.52) (Fig. 3C–E).
Comparative outcomes in patients with HCV with or without antiviral treatment. (A) PRS (A) and R-RFS (B) of patients with HBV and patients with HCV with or without antiviral treatment after post-resection HCC recurrence. PRS and RFS of patients with HCV with or without antiviral treatment who underwent rehepatectomy (C), RFA (D), or TACE (E) for recurrent HCC after post-resection HCC recurrence
Risk Factor Analysis
We analyzed the patients’ demographic and clinical data at primary HCC diagnosis and first recurrence to identify prognostic factors for PRS and R-RFS (Table 3). A multivariate analysis including risk factors that were significant in the univariate analysis (full panels of risk factors in Supplementary Table S1) revealed that early recurrence (PRS: HR = 1.926, 95% CI = 1.287–2.882; R-RFS: HR = 1.262, 95% CI = 1.011–1.576), high ALBI grades at recurrence (PRS: HR = 2.572, 95% CI = 1.737–3.810; R-RFS: HR = 1.724, 95% CI = 1.374–2.163), and recurrent tumors beyond the UCSF criteria (PRS: HR = 1.964, 95% CI = 1.189–3.257; R-RFS: HR = 2.558, 95% CI = 1.859–3.509) were risk factors for both poor PRS and R-RFS. Male sex (PRS: HR = 2.033, 95% CI = 1.262–3.276) was a significant risk factor for poor PRS, and multiple recurrent tumors (R-RFS: HR = 1.557, 95% CI = 1.227–1.975), the largest recurrent tumor > 3 cm in diameter (R-RFS: HR = 1.329, 95% CI = 1.040–1.696), and AFP > 100 ng/mL at recurrence (R-RFS: HR = 1.434, 95% CI = 1.116–1.843) were risk factors for poor R-RFS. Regarding treatment for recurrent HCC, RFA was a protective factor for both PRS and R-RFS, and rehepatectomy was a protective factor for R-RFS. Other factors, such as age, family history of HCC, HBV and HCV status, ALBI grade, liver cirrhosis, major hepatectomy, and primary HCC tumor characteristics, were not significant predictors of PRS or R-RFS.
Viral Background in Late Recurrence After Primary Hepatectomy: R-RFS (HBV > HCV)
We investigated whether the differential effect of HBV and HCV on the PRS and R-RFS was associated with late recurrence after primary hepatectomy (demographics shown in Supplementary Table S2). The 1-year, 3-year, and 5-year R-RFS rates were 66.7%, 37.5%, and 26.0%, respectively, in the HBV group (n = 275) and were 61.3%, 24.5%, and 6.9%, respectively, in the HCV group (n = 102). The R-RFS rates of the patients who developed late recurrence were higher among those with HBV and lower among those with HCV (Fig. 4A). This difference was not noted among those who developed early recurrence.
Late recurrence after primary resection for HCC and post-recurrence survivals (PRS and R-RFS). (A) HBV and HCV. (B) HCV with or without antiviral treatment. Abbreviations: HBV, hepatitis B virus; HCC, hepatocellular carcinoma; HCV, hepatitis C virus; PRS, post-recurrence survival; R-RFS, rerecurrence-free survival
The 1-year, 3-year, and 5-year PRS rates were 100%, 91.8%, and 84.5%, respectively, in the HBV group and were 98.9%, 91.1%, and 83.7%, respectively, in the HCV group. No significant difference in PRS was identified regarding HBV or HCV status.
Furthermore, survival outcomes for HCV patients who developed early and late recurrence were compared. For patients who developed late recurrence, patients receiving antiviral treatment had better PRS and R-RFS outcomes than those without antiviral treatment (P = 0.020 and 0.041, respectively; Fig. 4B). In patients with early recurrence, no significant difference in PRS and R-RFS was identified regardless of receiving antiviral treatment or not.
Sensitivity Analysis for HCC Within UCSF Criteria
To evaluate the treatment effectiveness with balanced tumor burden, we performed sensitivity analysis, comparing the three treatment groups of patients with recurrent HCC status within UCSF criteria. The survival benefits (PRS and R-RFS) of rehepatectomy and RFA over TACE were consistent (Supplementary Fig. S1).
Discussion
Our study revealed four main findings. First, rehepatectomy and RFA are equal as treatments for recurrent HCC with long-term effectiveness. Second, early recurrence, recurrent tumor status, and ALBI grade were identified as key prognostic factors for HCC rerecurrence. Third, for the patients with HBV and non-B, non-C, rehepatectomy and RFA provided greater PRS and R-RFS than TACE. In HCV patients who received RFA for HCC recurrence, antiviral treatment was associated with improved PRS. Lastly, for patients with late recurrence, R-RFS was better in subgroups of HBV and HCV patients who received antiviral treatment than naïve HCV patients. Survival difference triaged by viral status was lost in the counterpart of early recurrence.
Management of recurrent HCC after primary resection is complex, involving multidisciplinary teams and various treatment options,23 including rehepatectomy, RFA, TACE, and liver transplantation. The 5-year post-recurrence survival rates of patients who undergo such treatments range from 13.8 to 70%,23,24,25 with a median R-RFS duration of 12 months.26 Our study included patients with intrahepatic recurrence amenable to aggressive treatment, and the 5-year survival rates of the patients were higher than those in previous studies.23,27 In addition, the patients in the RFA and rehepatectomy groups had equal PRS and R-RFS rates regardless of their viral statuses. This observation remained consistent in patients with small tumor (≤ 3 cm) (data not shown). These findings proved that RFA serves as a reliable treatment for recurrent HCC, providing equivalent survival outcomes for small recurrent HCC tumors.9,28,29,30
Several prognostic factors for post-recurrence survival have been identified in previous studies, including early recurrence, an AFP level > 400 ng/mL, and primary HCC beyond the BCLC criteria.5,26,31 In the present study, treatments received for recurrent tumors, early recurrence, ALBI grades of recurrent tumors, AFP level, and primary tumor status were identified as prognostic factors for PRS and R-RFS. ALBI has been validated as a useful prognostic factor for survival among patients with HCC32,33 and has been used alone or integrated into prognostic models for the prediction of early recurrence after hepatectomy.33,34 In the present study, ALBI grade at the time of recurrence was identified to be a prognostic factor for PRS and R-RFS after treatment for recurrent HCC, suggesting its usefulness for predicting the treatment responses of patients with recurrent HCC as well.
Our study analyzed the efficacy of different therapeutic treatments with different viral backgrounds for recurrent HCC after curative hepatectomy. Patients with HBV and HCV could behave much differently as far as recurrence and likelihood of concomitant cirrhosis. Prior studies had demonstrated that among patients who developed primary HCC with different viral backgrounds, patients with HCV had poorer survival outcomes, compared with those with HBV or non-B, non-C, which was associated with a higher rate of late recurrence due possibly to multicentric hepatocarcinogenesis.35,36 Therefore, the rationale to compare outcomes of HCC with different viral backgrounds seems valid. Consistently, outcome of HCC recurrence was better in our HBV patients, which could further be a benchmark reference subgroup in comparative outcome of treating HCC recurrence.
Singal et al. 37 had demonstrated DAA reduced mortality in patients with prior treated HCC (with unclear primary or recurrence status). Anti-HCV treatment has become an indispensable element in managing HCV-HCC with the benefit of reducing HCC recurrence and improved liver profile.38 We acknowledge that the study is largely from an era before curative HCV therapy with a high rate of success using DAA. Nevertheless, the risk of HCC recurrence could be decreased but not eliminated, and post-recurrence outcome may still be affected by different treatment modalities. Moreover, post-recurrence outcome after treatment is not exactly “clock reset” back to that of primary HCC and warrants further studies.27 Our study showed that rehepatectomy and RFA were less beneficial than TACE in PRS for patients with HCV. For patients with late HCC recurrence, R-RFS was better in subgroups of HBV and HCV patients who received antiviral treatment than naïve HCV patients. For patients with early recurrence, antiviral treatment had less impact on survival outcome. Late recurrence was associated with de novo HCC tumorigenesis in the remnant liver, wherein liver reserve may be of greater importance in long-term outcomes.39 Patients with HBV generally received antiviral medication after primary resection,18,40 which reduces the risk of HCC recurrence, as HBsAg seroclearance reduced the risk of recurrence following hepatectomy.41 Antiviral treatment for HCV provided better PRS and R-RFS among those who developed late recurrence, which may be related to therapeutic benefit of improved liver reserve after viral eradication.42 Our results contribute to literature that with antiviral treatment for HCV, these patients could achieve comparable oncological outcomes to those patients with HBV.
Non-B, non-C patients, who comprised of 15.2% of our cohort, have been increasing in the past few years43 and exhibit distinctive HCC patterns that require attention.44,45 A recent study revealed that patients with NAFLD-related HCC were older, more likely to have metabolic comorbidities, and less likely to have liver cirrhosis than those HCC deriving from viral causes and were therefore less likely to receive early surveillance and diagnosis.46
Remnant liver function and HCC etiology are key factors influencing the outcomes in patients treated with immunotherapy or targeted therapy. As more systemic therapy options have become available, the survival rates of patients with advanced HCC have improved.47 The approval of new targeted agents and immune checkpoint inhibitors has facilitated the management of advanced-stage HCC and increased patients’ chances of tumor downstaging. A meta-analysis revealed that the effectiveness of immunotherapy was not affected by viral status, the KEYNOTE-240 and CheckMate-459 studies revealed no significant association between HCC etiology and tumor response to immunotherapy.48 Nevertheless, patients with viral etiologies may benefit from checkpoint inhibitor therapy, whereas those with nonviral etiologies such as NAFLD may not respond to immunotherapy.49 Hepatocarcinogenesis has viral and nonviral etiologies involving complex interactions between liver injury, cirrhosis, and immune cells. Further clarification of the underlying mechanisms of hepatocarcinogenesis may help identify patients that may benefit from aggressive local treatments.
Our study has some limitations. This was a retrospective study, and the treatments that patients received for primary and recurrent HCC tumors might have biased the results.
Conclusion
The effectiveness of rehepatectomy and RFA as treatments for recurrent HCC was mostly equivalent and superior to TACE. For HBV patients, rehepatectomy and RFA were protected against rerecurrence. HCV patients who received antiviral treatment benefited from RFA. Antiviral treatments improved survival outcomes in both HBV and HCV subgroups among patients with late recurrence, but not early recurrence. Prognostication in treating HCC recurrence after primary resection was associated with viral status.
Data Availability
The data that support the findings of this study are available from the corresponding author, C.-M. H., upon reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249.
Omata M, Cheng AL, Kokudo N, Kudo M, Lee JM, Jia J, et al. Asia-Pacific clinical practice guidelines on the management of hepatocellular carcinoma: a 2017 update. Hepatol Int. 2017;11(4):317-370.
Kulik L, El-Serag HB. Epidemiology and management of hepatocellular carcinoma. Gastroenterology. 2019;156(2):477-491.
Park JW, Chen M, Colombo M, Roberts LR, Schwartz M, Chen PJ, et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int. 2015;35(9):2155-2166.
Tsilimigras DI, Bagante F, Moris D, Hyer JM, Sahara K, Paredes AZ, et al. Recurrence patterns and outcomes after resection of hepatocellular carcinoma within and beyond the Barcelona Clinic Liver Cancer criteria. Ann Surg Oncol. 2020;27(7):2321-2331.
Taketomi A, Toshima T, Kitagawa D, Motomura T, Takeishi K, Mano Y, et al. Predictors of extrahepatic recurrence after curative hepatectomy for hepatocellular carcinoma. Ann Surg Oncol. 2010;17(10):2740-2746.
Portolani N, Coniglio A, Ghidoni S, Giovanelli M, Benetti A, Tiberio GA, et al. Early and late recurrence after liver resection for hepatocellular carcinoma: prognostic and therapeutic implications. Ann Surg. 2006;243(2):229-235.
Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American association for the study of liver diseases. Hepatology. 2018;68(2):723-750.
Ho CM, Lee PH, Shau WY, Ho MC, Wu YM, Hu RH. Survival in patients with recurrent hepatocellular carcinoma after primary hepatectomy: comparative effectiveness of treatment modalities. Surgery. 2012;151(5):700-709.
Reig M, Forner A, Rimola J, Ferrer-Fabrega J, Burrel M, Garcia-Criado A, et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol. 2022;76(3):681-693.
Giraud J, Chalopin D, Blanc JF, Saleh M. Hepatocellular carcinoma immune landscape and the potential of immunotherapies. Front Immunol. 2021;12:655697.
Chang CH, Lin JW, Wu LC, Liu CH, Lai MS. National antiviral treatment program and the incidence of hepatocellular carcinoma and associated mortality in Taiwan: a preliminary report. Med Care. 2013;51(10):908-913.
Liu CJ, Chen PJ. Elimination of hepatitis B in highly endemic settings: lessons learned in Taiwan and challenges ahead. Viruses. 2020;12(8):815.
Chien RN, Lu SN, Pwu RF, Wu GH, Yang WW, Liu CL. Taiwan accelerates its efforts to eliminate hepatitis C. Glob Health Med. 2021;3(5):293-300.
Chiang CJ, Yang YW, Chen JD, You SL, Yang HI, Lee MH, et al. Significant reduction in end-stage liver diseases burden through the national viral hepatitis therapy program in Taiwan. Hepatology. 2015;61(4):1154-1162.
Ho CM, Lee PH, Chen CL, Ho MC, Wu YM, Hu RH. Long-term outcomes after resection versus transplantation for hepatocellular carcinoma within UCSF criteria. Ann Surg Oncol. 2012;19(3):826-833.
Cheng HY, Ho CM, Hsiao CY, Ho MC, Wu YM, Lee PH, et al. Interval dynamics of transplantability for hepatocellular carcinoma after primary curative resection: risk factors for nontransplantable recurrence. HPB (Oxford). 2023;25(2):218-228.
Ho CM, Lee CH, Lee MC, Zhang JF, Chen CH, Wang JY, et al. Survival after treatable hepatocellular carcinoma recurrence in liver recipients: a nationwide cohort analysis. Front Oncol. 2020;10:616094.
Hong YM, Cho M, Yoon KT, Chu CW, Yang KH, Park YM, et al. Risk factors of early recurrence after curative hepatectomy in hepatocellular carcinoma. Tumour Biol. 2017;39(10):1010428317720863.
Ho MC, Huang GT, Tsang YM, Lee PH, Chen DS, Sheu JC, et al. Liver resection improves the survival of patients with multiple hepatocellular carcinomas. Ann Surg Oncol. 2009;16(4):848-855.
Su TH, Wu CH, Liu TH, Ho CM, Liu CJ. Clinical practice guidelines and real-life practice for hepatocellular carcinoma in Taiwan. Clin Mol Hepatol. 2023;29(2):230-241.
Johnson PJ, Berhane S, Kagebayashi C, Satomura S, Teng M, Reeves HL, et al. Assessment of liver function in patients with hepatocellular carcinoma: a new evidence-based approach-the ALBI grade. J Clin Oncol. 2015;33(6):550-508.
Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S. Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann Surg. 2015;261(5):947-955.
Chan AC, Chan SC, Chok KS, Cheung TT, Chiu DW, Poon RT, et al. Treatment strategy for recurrent hepatocellular carcinoma: salvage transplantation, repeated resection, or radiofrequency ablation? Liver Transpl. 2013;19(4):411-419.
Tsilimigras DI, Moris D, Hyer JM, Bagante F, Ratti F, Marques HP, et al. Serum alpha-fetoprotein levels at time of recurrence predict post-recurrence outcomes following resection of hepatocellular carcinoma. Ann Surg Oncol. 2021;28(12):7673-7683.
Wei T, Zhang XF, Bagante F, Ratti F, Marques HP, Silva S, et al. Early versus late recurrence of hepatocellular carcinoma after surgical resection based on post-recurrence survival: an international multi-institutional analysis. J Gastrointest Surg. 2021;25(1):125-133.
Ivanics T, Murillo Perez CF, Claasen M, Patel MS, Morgenshtern G, Erdman L, et al. Dynamic risk profiling of HCC recurrence after curative intent liver resection. Hepatology. 2022;76(5):1291-1301.
Gavriilidis P, Askari A, Azoulay D. Survival following redo hepatectomy vs radiofrequency ablation for recurrent hepatocellular carcinoma: a systematic review and meta-analysis. HPB (Oxford). 2017;19(1):3-9.
Xia Y, Li J, Liu G, Wang K, Qian G, Lu Z, et al. Long-term effects of repeat hepatectomy vs percutaneous radiofrequency ablation among patients with recurrent hepatocellular carcinoma: a randomized clinical trial. JAMA Oncol. 2020;6(2):255-263.
Erridge S, Pucher PH, Markar SR, Malietzis G, Athanasiou T, Darzi A, et al. Meta-analysis of determinants of survival following treatment of recurrent hepatocellular carcinoma. Br J Surg. 2017;104(11):1433-1442.
Xing H, Sun LY, Yan WT, Quan B, Liang L, Li C, et al. Repeat hepatectomy for patients with early and late recurrence of hepatocellular carcinoma: A multicenter propensity score matching analysis. Surgery. 2021;169(4):911-920.
Hiraoka A, Kumada T, Michitaka K, Toyoda H, Tada T, Ueki H, et al. Usefulness of albumin-bilirubin grade for evaluation of prognosis of 2584 Japanese patients with hepatocellular carcinoma. J Gastroenterol Hepatol. 2016;31(5):1031-1036.
Lee YH, Koh YS, Hur YH, Cho CK, Kim HJ, Park EK. Effectiveness of the albumin-bilirubin score as a prognostic factor for early recurrence after curative hepatic resection for hepatocellular carcinoma. Ann Hepatobiliary Pancreat Surg. 2018;22(4):335-343.
Chan AWH, Zhong J, Berhane S, Toyoda H, Cucchetti A, Shi K, et al. Development of pre and post-operative models to predict early recurrence of hepatocellular carcinoma after surgical resection. J Hepatol. 2018;69(6):1284-1293.
Utsunomiya T, Shimada M, Kudo M, Ichida T, Matsui O, Izumi N, et al. A comparison of the surgical outcomes among patients with HBV-positive, HCV-positive, and non-B non-C hepatocellular carcinoma: a nationwide study of 11,950 patients. Ann Surg. 2015;261(3):513-520.
Sasaki Y, Yamada T, Tanaka H, Ohigashi H, Eguchi H, Yano M, et al. Risk of recurrence in a long-term follow-up after surgery in 417 patients with hepatitis B- or hepatitis C-related hepatocellular carcinoma. Ann Surg. 2006;244(5):771-780.
Singal AG, Rich NE, Mehta N, Branch AD, Pillai A, Hoteit M, et al. Direct-acting antiviral therapy for hepatitis C virus infection is associated with increased survival in patients with a history of hepatocellular carcinoma. Gastroenterology. 2019;157(5):1253-1263.
Mocan T, Nenu I, Craciun R, Sparchez Z. Treatment of hepatitis C virus infection in patients with hepatocellular carcinoma: Truth or dare? J Gastroenterol Hepatol. 2021;36(6):1518-1528.
Imamura H, Matsuyama Y, Tanaka E, Ohkubo T, Hasegawa K, Miyagawa S, et al. Risk factors contributing to early and late phase intrahepatic recurrence of hepatocellular carcinoma after hepatectomy. Journal of Hepatology. 2003;38(2):200-207.
Huang G, Li P-p, Lau WY, Pan Z-y, Zhao L-h, Wang Z-g, et al. Antiviral therapy reduces hepatocellular carcinoma recurrence in patients with low HBV-DNA levels. Annals of Surgery. 2018;268(6):943-954.
Yoo S, Kim JY, Lim YS, Han S, Choi J. Impact of HBsAg seroclearance on late recurrence of hepatitis B virus-related hepatocellular carcinoma after surgical resection. J Hepatol. 2022;77(4):939-946
Cheung MCM, Walker AJ, Hudson BE, Verma S, McLauchlan J, Mutimer DJ, et al. Outcomes after successful direct-acting antiviral therapy for patients with chronic hepatitis C and decompensated cirrhosis. J Hepatol. 2016;65(4):741-747.
Tsai YC, Sou FM, Liu YW, Wu YJ, Yong CC, Chen DW, et al. Preoperative ALBI grade predicts the outcomes in non-B non-C HCC patients undergoing primary curative resection. BMC Gastroenterol. 2021;21(1):386.
McIntyre CA, Chou JF, Gonen M, Shia J, Gambarin-Gelwan M, Balachandran VP, et al. Hepatocellular carcinoma in patients with no identifiable risk factors. HPB (Oxford). 2021;23(1):118-126.
Yang T, Hu LY, Li ZL, Liu K, Wu H, Xing H, et al. Liver resection for hepatocellular carcinoma in non-alcoholic fatty liver disease: a multicenter propensity matching analysis with HBV-HCC. J Gastrointest Surg. 2020;24(2):320-329.
Tan DJH, Ng CH, Lin SY, Pan XH, Tay P, Lim WH, et al. Clinical characteristics, surveillance, treatment allocation, and outcomes of non-alcoholic fatty liver disease-related hepatocellular carcinoma: a systematic review and meta-analysis. The Lancet Oncology. 2022;23(4):521-530.
Ayoub WS, Jones PD, Yang JD, Martin P. Emerging drugs for the treatment of hepatocellular carcinoma. Expert Opin Emerg Drugs. 2022;27(2):141-149.
Ho WJ, Danilova L, Lim SJ, Verma R, Xavier S, Leatherman JM, et al. Viral status, immune microenvironment and immunological response to checkpoint inhibitors in hepatocellular carcinoma. J Immunother Cancer. 2020;8(1):e000394.
Pfister D, Nunez NG, Pinyol R, Govaere O, Pinter M, Szydlowska M, et al. NASH limits anti-tumour surveillance in immunotherapy-treated HCC. Nature. 2021;592(7854):450-456.
Author information
Authors and Affiliations
Contributions
Dr. Cheng had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Project development: H.-Y. C., C.-M. H., and R.-H. H.
Protocol development: C.-M. H., P.-H. L., and R.-H. H.
Data management: P.-H. L.
Data analysis: C.-Y. H., M.-C. H., and R.-H. H.
Manuscript writing/editing: Y.-M. W.
All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The National Taiwan University Hospital granted ethical approval to perform this study within its facilities (202111080RINB).
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cheng, HY., Hu, RH., Hsiao, CY. et al. Viral Status and Treatment Efficacy in Recurrent Hepatocellular Carcinoma After Primary Resection. J Gastrointest Surg 27, 1594–1610 (2023). https://doi.org/10.1007/s11605-023-05691-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-023-05691-z