Abstract
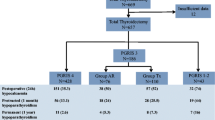
Parathyroid autotransplantation is a technique for ensuring the continued function of parathyroid tissue at the time of total thyroidectomy (TT). The aim of this study was to ascertain whether the number of parathyroids transplanted affects the incidence of temporary and permanent hypoparathyroidism. A retrospective cohort study included all patients undergoing a TT in a single unit between July 1998 and June 2003. The number of parathyroids transplanted, the final pathology, and the incidence of temporary and permanent hypoparathyroidism were documented. Fisher’s exact test was used for statistical analysis. A total of 1196 patients underwent a TT during the 5 years studied. Of these, 306 (25.6%) had no parathyroids transplanted, 650 (54.3%), 206 (17.2%), 34 (2.8%) had 1,2, or 3 glands autotransplanted, respectively. The incidence of temporary hypoparathyroidism was 9.8% for no gland transplants, 11.9%, 15.1%, and 31.4% for 1,2,and 3 gland transplants, respectively (p < 0.05). The incidence of permanent hypoparathyroidism was 0.98%, 0.77%, 0.97%, and 0%, respectively (p = NS). The incidence of temporary hypoparathyroidism was higher when surgery was performed for Graves’ disease. Temporary hypocalcemia is closely related to the number of autotransplanted parathyroids during TT. The long-term outcome is not affected by the number of parathyroids autotransplanted. A “ready selective” approach to parathyroid autotransplantation is an effective strategy for minimizing the rate of permanent hypoparathyroidism.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Permanent hypoparathyroidism following thyroid surgery is a potentially debilitating condition. Fears of permanent hypoparathyroidism have in the past led many surgeons to adopt subtotal thyroidectomy as their standard procedure for benign thyroid disease. However, it is increasingly recognized that total rather than subtotal thyroidectomy is the optimal procedure for benign multinodular goiters [1], as well as for all but the lowest risk thyroid cancers [2]. This has renewed the interest in the need for parathyroid preservation during thyroidectomy.
The preservation of as much functional parathyroid tissue in situ as possible is the key to minimizing permanent hypoparathyroidism. However, some glands may be anatomically intact but not physiologically viable, either because of thrombosis of the delicate parathyroid artery or because of parathyroid capsule edema despite meticulous dissection [3]. Furthermore, occasionally parathyroid glands may be inadvertently removed with the thyroid specimen during surgery because they were not identified intra operatively. The process of parathyroid autotransplantation during a partial thyroidectomy was first described by Lahey [4]. However, only after the demonstration of the viability of transplanted parathyroid tissue in humans [5] did autotransplantation became part of the endocrine surgical armamentarium. Most surgeons would accept that when preservation of parathyroid tissue in situ is not an option the best alternative is parathyroid autotransplantation (PAT) [6]. However, the adoption of PAT by endocrine surgeons has varied considerably from a selective approach with transplantation of nonviable glands [7] to routine autotransplantation of one gland [8] to autotransplantation of all identifiable parathyroids or at least two of the identified glands [9].
The aim of this study was to identify whether the number of parathyroids autotransplanted has an effect on the incidence of permanent hypoparathyroidism or the incidence of temporary hypocalcemia.
Methods
A retrospective cohort study comprising all patients that had a total thyroidectomy (TT) between July 1998 and June 2003 was performed. Data were obtained from the Endocrine Surgery database, which is prospectively compiled and regularly audited for accuracy. For each TT, the number of parathyroids transplanted, the histopathology, and the incidence of temporary hypocalcemia and permanent hypoparathyroidism were documented.
For the purposes of this study temporary hypocalcemia was defined as any patient with corrected serum calcium of less than 2 mmo1/1, with or without symptoms, that returned to the normal range at 3 months follow-up without requiring calcium supplementation. Permanent hypoparathyroidism was defined as any patient with a serum calcium level below the normal range or requiring calcium and/or vitamin D supplementation to remain eucalcaemic at 6 months from surgery.
Data were analyzed using the Stata Statistical Software package (version 7, Stata Corp, College Station, TX). Comparison of the rate of hypocalcemia and hypoparathyroidism was performed using Fisher’s exact test. The Alpha for significance was set at P < 0. 05
Results
A total of 1196 patients underwent TT in the University of Sydney Endocrine Surgery Unit in the 5 years between July 1998 and June 2003 with the indications for surgery and/or histopathology as documented in Table 1. Of these 306 (25.6%) had no parathyroid glands transplanted, 650 (54.3%) had 1 gland autotransplanted, 206 (17.2%) had 2 glands autotransplanted, and 34 (2.9%) had 3 glands autotransplanted.
Overall, 149 (12.5%) patients experienced temporary hypocalcemia after TT, with a statistically significant increase in incidence as the number of glands transplanted increased (Table 2).
The incidence of temporary hypocalcemia was higher in patients with Graves’ disease regardless of the number of parathyroid glands transplanted, although this difference became less marked as the number of parathyroid transplants increased. The incidence of permanent hypoparathyroidism in thyrotoxic patients was not significantly different from the overall incidence (Table 3).
Overall, there were 10 cases of permanent hypoparathyroidism after TT over 5 years and 1197 operations (0.84%). There were 3 cases in patients that had no PAT (0.98%), 5 cases in patients that had had one parathyroid transplanted (0.77%), 2 cases in patients that had two glands transplanted (0.97%), and no cases in patients that had three glands transplanted. These differences were not statistically significant.
Discussion:
Thyroid disease is prevalent [10], and over 8,200 primary thyroid operations are typically performed each year in the UK [11] and just over 4100 were performed over twelve months in Australia from 2002 to 2003. However, thyroidectomy continues to produce significant morbidity. In 1989 4% of all surgical claims settled by the Medical Defence Union in the UK [12], and 1% of all litigation relating to adverse effects after medical or surgical treatment in Germany between 1975 and 1998 were related to thyroid surgery [13]. After recurrent laryngeal nerve palsy, permanent hypoparathyroidism accounts for the largest category of thyroidectomy-related claims [12]. Because adverse events tend to be under reported in the literature, the true incidence of permanent hypoparathyroidism is difficult to ascertain, but incidences as low as 0% and as high as 43% have been reported [14]. Permanent hypoparathyroidism is a complication that commits the patient to lifelong calcium and vitamin D supplementation. It has been long known that chronic hypoparathyroidism is associated with an increased risk of cataract formation [15] and calcification of the basal ganglia [16], but reversible peripheral neuropathy [17] and cardiac pathology [18] may also occur. To reduce the risk of permanent hypoparathyroidism, many surgeons adopted a compromise operation in the form of subtotal thyroidectomy as their standard procedure for benign multinodular goiter and Graves’ disease. It is now accepted, however, that total rather than subtotal thyroidectomy is the optimal procedure for both benign multinodular goiter [1] and all the but the most low risk thyroid cancers [2]. This has lead to a resurgence in interest in the need for parathyroid preservation.
The preservation of as much functional parathyroid tissue in situ as possible during TT is the key to minimizing permanent hypoparathyroidism. This may be accomplished by a combination of preservation of the delicate parathyroid vasculature and ligation of the branches of the inferior thyroid artery as close as possible to the thyroid capsule. Despite the adoption of this approach, some glands maybe anatomically intact but not physiologically viable [9]. Indeed, time-consuming meticulous dissection to preserve functioning parathyroid glands in all cases is destined to fail in some either from thrombosis of the parathyroid artery or parathyroid capsule edema [3]. It can be difficult to ascertain the viability of an apparently anatomically intact parathyroid, and various methods of assessment have been adopted including the careful incision of the parathyroid capsule to assess for bleeding (the knife test) [19], Doppler measurements of the parathyroid vessels [20], and intraoperative parathyroid hormone (PTH) assays [21]. Furthermore, the unintentional removal of parathyroid tissue during thyroidectomy is well documented [22].
There is no question that the use of PAT can be associated with a low incidence of permanent hypoparathyroidism [14], but the cause –effect relationship is difficult to prove, because any approach adopted is probably a reflection of the skill and judgment of the surgeon adopting the technique rather than of the technique per se. Within our unit there has been a progressive evolution in the approach to PAT. Early on, PAT was rarely performed, but by the late 1980s the protocol called for a selective approach; i.e., only nonviable glands were transplanted. In the mid 1990s a policy of routine autotransplantation of one gland was introduced in an effort to reduce our incidence of hypoparathyroidism further [23]. Our cumulative experience has demonstrated that the removal of a well vascularized and otherwise normal parathyroid gland is unnecessary because it does not have a positive effect on the incidence of permanent hypoparathyroidism. For this reason a policy of “ready selective” PAT has been followed. This consists in the adoption of a low threshold for PAT when it is deemed that time-consuming dissection of the pedicle offers little chance of successfully preserving a functional parathyroid gland.
The efficacy of PAT may be inferred from our data that demonstrate the maintenance of normal serum calcium after the initial period of hypocalcemia. Proof that the grafted parathyroid tissue contributes to the restoration of eucalcemia along with the anatomically and physiologically intact parathyroid left in situ is more challenging because parathyroids are normally transplanted in the sternocleidomastoid muscle, and differentiating between graft function and the function of intact parathyroid glands is not accurate [24]. There are however, data from a series of 32 MEN 2A and 2B children who underwent prophylactic parathyroidectomy during a total thyroidectomy. These data reveal that 3 months after a period of postoperative hypocalcemia, normal calcium metabolism was restored in nearly all children [25]
Our data also confirm that PAT is associated with a higher incidence of temporary hypoparathyroidisrm, as has been previously documented [26]. We have also demonstrated that there is a correlation between the numbers of parathyroids transplanted and the incidence of temporary hypocalcemia. Our results with thyrotoxic patients concur with existing data demonstrating a higher incidence of temporary hypocalcemia in hyperthyroid patients, probably related to skeletal avidity for calcium associated with this pathology[27]. Indeed, there appears to be a correlation between temporary postoperative hypocalcemia and free thyroxine levels [28].
Significantly, the rate of permanent hypoparathyroidism is not a product of the number of glands transplanted at the time of surgery. Indeed, there were no cases of permanent hypoparathyroidism even when three glands were transplanted. This suggests that although there is no need to pursue the policy of routine PAT of at least one gland at every operation, it is a valid technique when a gland is judged to have been compromised or is likely to be compromised by the attempt to dissect the gland free. Adopted judiciously a “ready selective” PAT approach contributes to maintaining an overall incidence of permanent hypoparathyroidism below 1%, regardless of the number of glands transplanted.
References
TS Reeve L Delbridge A Cohen et al. (1987) ArticleTitleTotal thyroidectomy the preferred option of multinodular goitre Ann. Surg. 206 782–785 Occurrence Handle3689014
OH Clark (1997) Papillary thyroid carcinoma: rationale for total thyroidectomy OH Clark QY Duh (Eds) Textbook of Endocrine Surgery W. B. Saunders Philadelphia, 90–94
L. Delbridge (2002) ArticleTitleParathyroid autotransplantation: an essential technique for safe thyroid surgery Aust. N. Z. J. Surg. 72 852–853 Occurrence Handle10.1046/j.1445-2197.2002.02637.x
F. Lahey (1926) ArticleTitleThe transplantation of parathyroids in partial thyroidectomy Surg. Gynecol. Obstet. 62 508
SA Wells SuffixJr JC Gunnells JD Shelourne et al. (1975) ArticleTitleTransplantation of the parathyroid glands in man: clinical indications and results Surgery 78 34–44 Occurrence Handle1138398
Shaha AR, Byers RM, Terz JJ. Thyroid Cancer Surgical Practice Guidelines. Practice guidelines for major cancer sites, Society for surgical oncology, 1997.
AR Shaha C Burnett BM. Jaffe (1991) ArticleTitleParathyroid autotransplantation during thyroid surgery J. Surg. Oncol. 46 21–24 Occurrence Handle1986142
RE Wilson E Paloyan AM Lawrence MH Brooks JR. Picleman (1976) ArticleTitleDiscussion in Total thyroidectomy and parathyroid autotransplantation for radiation associated thyroid cancer . Surgery 80 70–76 Occurrence Handle1273769
H Funahashi et al. (1993) ArticleTitleOur technique of parathyroid autotransplantation in operation for papillary thyroid cancer Surgery 114 92–96 Occurrence Handle8356534
WM Tunbridge et al. (1977) ArticleTitleThe spectrum of thyroid disease in the community. The Whickham Survey Clin Endocrinol (Oxf) 7 481–493
JD Ramsden AP Johnson HC Cocks et al. (2002) ArticleTitleWho performs thyroid surgery: a review of current otolaryngologicalpractice practice Clin Otolaryngol. 27 304–309 Occurrence Handle10.1046/j.1365-2273.2002.00560.x
AR Ready AD. Barnes (1994) ArticleTitleComplications of thyroidectomy Br. J. Surg. 81 1555–1556 Occurrence Handle7827875
KM Schulte HD. Roher (1999) ArticleTitleMedico-legal aspects of thyroid surgery Chirurg 70 1131–1138 Occurrence Handle10.1007/s001040050875 Occurrence Handle10550343
CY. Lo (2002) ArticleTitleParathyroid autotransplantation during thyroidectomy Aust N. Z. J. Surg. 72 902–907 Occurrence Handle10.1046/j.1445-2197.2002.02580.x
AW Ireland JW Hornbrook FC Neale et al. (1968) ArticleTitleThe crystalline lens in chronic surgical hypoparathyroidism Arch. Intern. Med. 122 408–411 Occurrence Handle10.1001/archinte.122.5.408 Occurrence Handle5687928
MB Forman MP Sandler A Danziger et al. (1980) ArticleTitleBasal ganglia calcification in postoperative hypoparathyroidism Clin. Endocrinol. (Oxf) 12 385–390
R Goswami M Bhatia R Goyal et al. (2002) ArticleTitleReversible peripheral neuropathy in idiopathic hypoparathyroidism ActaNeurol. Scancd. 105 128–131
SN Levine CN. Rheams (1985) ArticleTitleHypocalcaemic heart failure Am. J. Med. 78 1033–1035 Occurrence Handle10.1016/0002-9343(85)90228-1 Occurrence Handle4014262
L. Delbridge (2003) ArticleTitleTotal thyroidectomy: the evolution of surgical technique Aust. N. Z. J. Surg. 73 761–768 Occurrence Handle10.1046/j.1445-2197.2003.02756.x
S Ander K Johansson S. Smeds (1997) ArticleTitleIn situ preservation of the parathyroid glands during oprations on the thyroid Eur. J. Surg. 163 33–37 Occurrence Handle9116109
FM Warren PE Anderson MK Wax et al. (2002) ArticleTitleIntraoperative parathyroid hormone levels in thyroid and parathyroid surgery Laryngoscope 112 1866–1870 Occurrence Handle10.1097/00005537-200210000-00031 Occurrence Handle12368632
NJ Lee JD Blakey S Bhuta et al. (1999) ArticleTitleUnintentional parathyroidectomy during thyroidectomy Laryngoscope 109 1238–1240 Occurrence Handle10.1097/00005537-199908000-00010 Occurrence Handle10443826
J Zedenius C Wadstrom L. Delbridge (1999) ArticleTitleRoutine autotransplantation of at least one parathyroid gland during total thyroidectomy may reduce permanent hypoparathyroidism to zero Aust. N. Z. J. Surg. 69 794–797 Occurrence Handle10.1046/j.1440-1622.1999.01697.x Occurrence Handle10553968
JA Olson MK DeBenedetti DS Baumann et al. (1996) ArticleTitleParathyroid autotransplantation during thyroidectomy: results of long term follow up.Ann Surg. 223 472–480
MA Skinner JA Norton JF Moley et al. (1997) ArticleTitleHeterotopic autotransplantation of parathyroid tissue in children undergoing total thyroidectomy J. Pediatr. Surg. 32 510–513 Occurrence Handle10.1016/S0022-3468(97)90618-7 Occurrence Handle9094030
R Bergamaschi G Becouarn J Reconceray et al. (1998) ArticleTitleMorbidity of thyroid surgery Am. Surg. 176 71–75 Occurrence Handle10.1016/S0002-9610(98)00099-3
N Demeester-Mirkine L Hooghe J Geertruyden ParticleVan et al. (1992) ArticleTitleHypocalcaemia after thyroidectomy Arch. Surg. 127 854–858 Occurrence Handle1524486
CR McHenry T Speroff D Wentworth et al. (1994) ArticleTitleRisk factors for -postthyroidectomy hypocalcemia Surgery 116 641–647 Occurrence Handle7940161
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Palazzo, F.F., Sywak, M.S., Sidhu, S.B. et al. Parathyroid Autotransplantation during Total Thyroidectomy—Does the Number of Glands Transplanted Affect Outcome?. World J. Surg. 29, 629–631 (2005). https://doi.org/10.1007/s00268-005-7729-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-7729-9