Abstract
Mortality rate following pancreaticoduodenectomy has markedly decreased in high-volume centers. We achieved zero mortality among 100 pancreaticoduodenectomies in a middle-volume center. The purpose of this study was to review our experience and analyze factors contributing to the zero mortality. Patient backgrounds, intraoperative variables, postoperative complications, and surgical, radiologic, and other medical interventions for the complications were retrospectively analyzed for 100 consecutive pancreaticoduodenectomies for malignant or benign disease. The mean age of the patients was 63 years. Altogether, 59 patients had preoperative co-morbidity, and 35 had a past history of abdominal surgery. The median operating time and blood loss were 525 minutes and 1215 ml, respectively. Postoperative complications occurred in 42 patients. The most frequent complication was pancreatic stump leak (n = 12), but no life-threatening pancreatic anastomotic leak occurred. This may result from the duct invagination anastomosis applied to 67 pancreases with a small duct. Serious complications were seen in six patients; two patients required surgical intervention, but four were successfully treated with the help of interventional radiologists or internists. Radiologic intervention was applied to 13 patients: drainage of an intraabdominal abscess/collection and vascular intervention. In addition to advances in surgical techniques to reduce local complications, particularly pancreatic anastomotic leak, intimate collaboration with experienced interventional radiologists and internists allows zero mortality even in middle-volume centers.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Postoperative complications following Whipple’s operation have not decreased during the last two decades, and a rate of approximately 40% has been reported even in recently published series.1,2 Meanwhile, the hospital mortality rate has markedly decreased below 4% in large-volume centers.1,2 Since 1990, three series of 118, 145, and 152 consecutive pancreaticoduodenectomies, respectively, without mortality have been reported.3–5 What contributed to the reduced mortality rate despite the unchanged morbidity rate? The frequency of serious postoperative complications, which possibly lead to patient deaths (e.g., pancreatic anastomotic leak, intraperitoneal abscess, hemorrhage) may have decreased. Advances in surgical techniques, surgical materials, and medications including antimicrobials and octreotide may be related factors.6,7 Furthermore, improved perioperative management to treat the complications may also be associated with decreased mortality. Recent advances in interventional radiology, in particular, are possibly responsible for the decline in mortality.2
Pancreatic anastomotic leak, which should be distinguished from stump leak of pure pancreatic juice, is an important common complication after pancreaticoduodenectomy and likely a major cause of in-hospital mortality.8,9 To reduce or eliminate this life-threatening complication, we have employed the pancreatic duct invagination anastomosis for the pancreas with a small duct and the duct-to-mucosa anastomosis for those with a large duct in 100 consecutive pancreaticoduodenectomies since November 1998. We then achieved zero mortality and only a 2% reoperation rate in this series. However, the morbidity rate was still considerable. The purpose of this study was to review our middle-volume center experience with pancreaticoduodenectomy and analyze factors contributing to the zero mortality.
METHODS
Patients
Between November 1998 and December 2003, a series of 100 consecutive pancreaticoduodenectomies were performed at our institution. Total pancreatectomy is not included in this study. Patient characteristics are summarized in Table 1. The mean age was 63 ± 11 years (range 33–82 years). Preoperative co-morbidity was detected in 59 patients: Diabetes or impaired glucose tolerance was present in 42, hypertension in 21, other cardiovascular diseases in 17, and acute pancreatitis in 3. In addition, 35 patients had a past history of one or more abdominal surgeries. Pathologic diagnoses included pancreatic cancer in 30 patients, cystic tumor of the pancreas in 17, ampullary cancer in 16, extrahepatic bile duct cancer in 13, chronic pancreatitis in 11, duodenal cancer in 7, and other diseases in 10. As shown in Table 2, a total of 65 standard Whipple operations and 35 pylorus-preserving procedures were performed. Altogether, 15 patients with pancreatic cancer, 1 with duodenal cancer, and 1 with gastric cancer underwent simultaneous portal vein resection. Combined resection of other organs included the right-side colon in 9 patients, partial liver in 2, and left kidney in 2 for cancer involvement or unrelated diseases.
Surgical Procedures
Pancreaticoduodenectomy was performed with various extents of lymphadenectomy according to the diagnosis and cancer stage. The pancreas was transected with an ultrasonic dissector (CUSA System; Cooper Medical Devices, Mountainview, CA, USA) in all instances as described previously.10,11 During the transection, even branch pancreatic ducts were identified, ligated, and divided. For the pancreatic duct invagination anastomosis, the main duct was exposed (>1 cm) and a 4F or 5F pancreatic stent (Suikan-tube; Sumitomo Bakelite, Tokyo, Japan) was inserted into the duct and fixed with two absorbable sutures (4-0 Poliglecaprone).
The first step of our reconstruction procedure was hepaticojejunostomy with interrupted 4-0 polydioxanone stitches. A stent catheter was placed through the anastomosis and exteriorized via the liver or the jejunum. Subsequently, pancreatic reconstruction was achieved with three different pancreaticojejunostomy techniques according to the pancreatic texture and duct size.12
The pancreatic duct invagination anastomosis was performed in 67 patients with a small duct (≤5 mm in diameter). Among these patients, stitches between the stump parenchyma and jejunal seromuscular layer were added only for hard texture (n = 11), not for soft texture (n = 56), to avoid parenchymal ischemia and internal laceration. The conventional duct-to-mucosa anastomosis was applied to 33 patients with a large duct (> 5 mm) (Table 2). Details of the pancreatic duct invagination anastomosis were published elsewhere.12,13 In brief, a 10-gauge intravenous catheter was passed through the jejunum, and the pancreatic stent was introduced through this catheter. The main duct was anchored to the adjacent serosa using the absorbable sutures with which the pancreatic stent had been fixed, and 3 ml of fibrin glue was sprayed on the pancreas stump. Gastrojejunostomy was then performed with the standard two-layer anastomosis. Two closed drains were placed in the vicinity of the biliary and pancreatic anastomoses.
Postoperative Management
All patients were monitored postoperatively in the intensive care unit (ICU) for 12 to 40 hours and subsequently transferred to the pancreatobiliary regular care floor. Prophylactic intravenous antibiotics were started intraoperatively followed by the same regimen every 12 hours for 4 to 5 days. The antibiotics used were cefotiam, cefazolin sodium, or flomoxef (an oxacephem antibiotic of broad antibacterial activity). Once an infective complication was diagnosed, a sensitive antibiotic was selected and administered. Intravenous hyperalimentation and protease inhibitors were routinely used postoperatively in all patients. A histamine H2-receptor blocker was given during postoperative hospitalization, but octreotide and erythromycin lactobionate were not used in this series. A stent catheter placed through the bile duct anastomosis was clamped 2 weeks after surgery and removed at 3 weeks. A pancreatic stent was removed around 4 weeks postoperatively. Intraperitoneal closed drains were removed at the discretion of the attending surgeon, usually between postoperative days 5 and 8, depending on the drainage output and the fluid amylase level.
Assessments
Intraoperative data, including the operating time, estimated total blood loss, and blood transfusion, were collected from the surgical records. Clinical information regarding the postoperative course (i.e., complications, readmission to the ICU, additional operation, in-hospital mortality) were retrospectively collected from hospital charts. Postoperative complications for which ICU readmission was required were defined as serious complications.
The amylase level in drainage fluid from a drain placed in the area of the pancreatic anastomosis was determined on day 7. A pancreatic fistula was diagnosed when the drainage fluid amylase concentration was more than three times the serum concentration regardless of the output volume. In pancreatic fistula patients, 20 ml of contrast medium (Urografin) was introduced through a transanastomotic bile stent into the jejunal loop for follow-through radiographic studies to rule out pancreatic anastomotic leak (disruption). Unless extraluminal Urografin leak around pancreaticojejunostomy was seen, the fistula was considered a pancreatic stump leak.
RESULTS
Intraoperaive and postoperative results are summarized in Table 3. The median operating time and blood loss were 525 minutes (range 375–1075 minutes) and 1215 ml (range 300–7360 ml), respectively. Blood transfusion was required intraoperatively in 65 patients. The median number of transfused blood units was 4 (range 0–50).
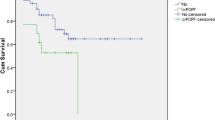
A total of 48 complications were recorded in 42 patients in this series. Twelve patients with a soft pancreas developed pancreatic stump leak, which was the most frequent complication. However, no pancreatic anastomotic leak occurred. Seven of these stump leaks were drained through the perianastomosis drain and removed with no sequelae. Intraabdominal collection was diagnosed in 10 patients, 8 of whom underwent percutaneous drainage; 5 were related to pancreatic stump leak based on the discharge fluid amylase levels. All eventually closed during the hospitalization. Two liver abscesses were treated percutaneously by interventional radiologists. Eleven patients developed delayed gastric emptying: three (4.6%) after a standard Whipple operation and eight (22.9%) after pylorus-preserving procedures. Systemic complications were diagnosed in four patients.
Serious complications requiring ICU readmission were seen in six patients. An additional operation was undertaken in two of the six patients, both within 24 hours postoperatively. One patient received emergency hemostasis for bleeding from the incompletely ligated inferior pancreatoduodenal artery. Another patient undergoing common hepatic artery resection for tumor invasion developed an early-onset thrombosis around the arterial anastomosis site. Because radiologic intervention failed to remove this thrombus, a second hepatic arterial reconstruction was required. No patient required relaparotomy for pancreatic fistula in this series. The other four serious complications included two systemic ones: Mobitz II atrioventricular block with transient cardiac arrest and pulmonary embolism, both of which were successfully treated with adequate medications. The other two complications were arterial bleeding, one from the stump of the gastroduodenal artery and the other from a common hepatic artery aneurysm. Both were associated with an infected pancreatic stump leak and were successfully controlled with occlusion by fiber metal coils in the common hepatic artery.
Radiologic intervention was applied to a total of 13 patients: drainage of an intraabdominal collection (n = 8) or liver abscess (n = 2) and vascular intervention (n = 3). There was no in-hospital mortality in this series.
DISCUSSION
Several studies have examined the effect of institutional volume on patient outcomes after pancreaticoduodenectomy and demonstrated that high-volume centers had significantly less mortality than low-volume centers.14–18 Birkmeyer et al., explained this effect by the “practice makes perfect” hypothesis and the “selective referral” hypothesis.18 However, the definitions of high volume varied among all these studies, from more than 5 to more than 50 cases per year.17,18 A large surveillance study in The Netherlands demonstrated the clear inverse relation between hospital volume and mortality, showing a death rate of 16% in low-volume (< 5) hospitals and 1% in high-volume (≥ 25) hospitals.15 Based on their criteria, our hospital belongs to the category of middle-volume centers. Among three previous series of more than 100 consecutive pancreaticoduodenectomies performed without mortality since 1990,3–5 two series of 107 and 145 patients, respectively, were published from high-volume centers3,4 and one from a middle-volume center, which achieved zero mortality among 152 patients with pancreaticogastrostomy.5 We reported herein the first zero mortality series of pancreaticoduodenectomy with pancreaticojejunostomy from a middle-volume center.
Although there was no mortality in this series, the postoperative morbidity rate was 42%. This considerable rate was comparable to those reported in the recent literature, and morbidity rates published in these two decades remained almost unchanged. Most patients undergoing pancreaticoduodenectomy are from a geriatric population in whom preoperative co-morbidity is likely. In addition, they frequently have past histories of one or more abdominal surgeries. This series noted 59 co-morbidities and 35 histories of abdominal surgery. Aranha et al., also reported substantial co-morbidity rates in their series,5 and others demonstrated a relation between either advanced age or co-morbidity and the complication rate.19,20 Moreover, because a large proportion of the indications are malignancy, retroperitoneal lymphadenectomy with or without neural dissection is required. These patient backgrounds combined with this high risk surgery are likely associated with the substantial and unchanged morbidity rates.
Among the local complications, pancreatic fistula is a common, important complication. Most published series have enrolled both pancreatic-enteric anastomosis disruption (pancreatic anastomotic leak) and extravasation of pancreatic secretions from the branch duct open on the stump (pancreatic stump leak) in the pancreatic fistula. The pancreatic stump leak is clinically unimportant and usually managed successfully. In contrast, the anastomotic leak is a risky complication that can lead to life-threatening complications including intraabdominal abscess, subsequent sepsis, and massive hemorrhage because this pancreatic fistula is strongly activated by the concomitant leak of enteric contents.7 In fact, considerable anastomotic leak-related deaths have been reported in the literature.8,9 Therefore, although the overall morbidity rate after pancreaticoduodenectomy is difficult to reduce significantly, prevention of the anastomotic leak is of vital importance to reduce or eliminate postoperative mortality.
In an attempt to prevent pancreatic anastomotic leak, we have employed three anastomotic techniques according to the pancreatic texture and the duct size.12 The duct-invagination anastomosis selected for pancreases with a small duct, a high risk group of pancreatic anastomotic leak, requires only a small puncture on the jejunum with an intravenous catheter instead of opening the jejunum. As a result, although 12 patients with a soft pancreas and a small duct developed pancreatic stump leak, no pancreatic anastomotic leak occurred, which is thought to be the reason for zero mortality in our series. However, there were still serious local and systemic complications in this series.
Interventional radiology plays an important role in reducing mortality after major abdominal surgery. Pancreaticoduodenectomy, in particular, frequently requires radiologic intervention because this aggressive surgery is still associated with intraabdominal collection/abscess, hemorrhage, and vascular complications, all of which can result in death.9 In our series, radiologic intervention was applied to 13 patients. Although a patient who developed thrombosis in the hepatic artery eventually required an additional operation, another 12 patients were successfully treated without the need for surgical intervention. In addition to the local complications, two patients with serious systemic complications (life-threatening arrhythmia and pulmonary embolism) were successfully treated and managed by internists. Gouma et al.,15 underlined the importance of the availability of hospital facilities and special care in their series of 300 consecutive pancreaticoduodenectomies. Our results additionally indicated that a multidisciplinary approach and active management of complications throughout the postoperative period allow zero mortality, at least in middle-volume centers.
CONCLUSIONS
These results suggest that our zero mortality was due not only to the contribution of surgery but also to other medical and radiologic interventions. In addition to the advances in surgical techniques to reduce pancreatic anastomotic leak and other local complications, intimate collaboration with experienced interventional radiologists and other specialists seems to be essential to reduce mortality even further. Given sufficient circumstances in an institution, zero or nearly zero mortality is possible even in middle-volume centers.
References
Conlon KC, Labow D, Leung D, et al. Prospective randomized clinical trial of the value of intraperitoneal drainage after pancreatic resection. Ann Surg 2001;234:487–494
Sohn TA, Yeo CJ, Cameron JL, et al. Pancreaticoduodenectomy: role of interventional radiologists in managing patients and complications. J Gastrointest Surg 2003;7:209–219
Trede M, Schwall G, Saeger H-D. Survival after pancreaticoduodenectomy: 118 consecutive resections without an operative mortality. Ann Surg 1990;211:447–458
Cameron JL, Pitt HA, Yeo CJ, et al. One hundred and forty-five consecutive pancreaticoduodenectomies without mortality. Ann Surg 1993;217:430–438
Aranha GV, Hodul PJ, Creech S, et al. Zero mortality after 152 consecutive pancreaticoduodenectomies with pancreaticogastrostomy. J Am Coll Surg 2003;197:223–232
Sampliner JE. Postoperative care of the pancreatic surgical patient: the role of the intensivist. Surg Clin North Am 2001;81:637–645
Gouillat C, Gigot J-F. Pancreatic surgical complications: the case for prophylaxis. Gut 2001;48(Suppl. IV):iv32–iv39
Sikora SS, Posner MC. Management of the pancreatic stump following pancreaticoduodenectomy. Br J Surg 1995;82:1590–1597
Halloran CM, Ghaneh P, Bosonnet L, et al. Complications of pancreatic cancer resection. Dig Surg 2002;19:138–146
Kuroda Y, Tanioka Y, Suzuki Y, et al. Distal pancreatectomy using the ultrasonic dissector. J Am Coll Surg 1995;180:737–738
Suzuki Y, Fujino Y, Tanioka Y, et al. Randomized clinical trial of ultrasonic dissector or conventional division in distal pancreatectomy for non-fibrotic pancreas. Br J Surg 1999;86:608–611
Suzuki Y, Fujino Y, Tanioka Y, et al. Selection of pancreaticojejunostomy techniques according to pancreatic texture and duct size. Arch Surg 2002;137:1044–1047
Suzuki Y, Fujino Y, Ku Y, et al. New pancreatic duct-invagination anastomosis using ultrasonic dissection for non-fibrotic pancreas with a nondilated duct. World J Surg 2002;26:162–165
White RR, Shah AS, Tyler DS. Pancreatic cancer since Halsted. Ann Surg 2003;238:S132–S147
Gouma DJ, van Geenen RC, van Gulik TM, et al. Rates of complications and death after pancreaticoduodenectomy: risk factors and the impact of hospital volume. Ann Surg 2000;232:786–795
Ho V, Heslin MJ. Effect of hospital volume and experience on in-hospital mortality for pancreaticoduodenectomy. Ann Surg 2003;237:509–514
Lieberman MD, Kilbum H, Lindsey M, et al. Relation of perioperative deaths to hospital volume among patients undergoing pancreatic resection for malignancy. Ann Surg 1995;225:638–645
Birkmeyer JD, Finlayson SRG, Toeteson ANA, et al. Effect of hospital volume on in-hospital mortality with pancreaticoduodenectomy. Surgery 1999;125:250–256
Bathe OF, Caldera H, Hamilton KL, et al. Diminished benefit from resection of cancer of the head of the pancreas in patients of advanced age. J Surg Oncol 2001;77:115–122
Finlayson EV, Birkmeyer JD, Stukel TA, et al. Adjusting surgical mortality rates for patient comorbidities: more harm than good? Surgery 2002;132:787–794
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suzuki, Y., Fujino, Y., Ajiki, T. et al. No Mortality among 100 Consecutive Pancreaticoduodenectomies in a Middle-volume Center. World J. Surg. 29, 1409–1414 (2005). https://doi.org/10.1007/s00268-005-0152-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-005-0152-4