Abstract
Obturator hernias are extremely rare abdominal hernias but are often associated with high morbidity and mortality. They are more common in thin elderly women and, in the majority of circumstances, present as small bowel obstructions. A high level of clinical suspicion is key and cross-sectional imaging can be very helpful in establishing the diagnosis and evaluating for bowel compromise. Operative approach should be guided by bowel viability and surgeon experience and expertise.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Algorithmic Approach
-
A.
Obturator hernias occur when the abdominal contents protrude through the obturator canal. They are quite rare, accounting for less than 1% of abdominal wall hernias, and are more common in thin elderly women, likely due to loss of supporting connective tissue and wider female pelvis [1]. In more than 90% of cases, the presenting symptom is a small bowel obstruction and the diagnosis is made intraoperatively [2]. Other symptoms include groin pain radiating medially to the knee (obturator neuralgia), palpable proximal thigh mass, or ecchymosis of the thigh in the setting of bowel necrosis.
-
B.
Obturator hernias are often not detectable on physical exam as the hernia is concealed beneath the adductor muscles. However, sometimes a palpable mass in the groin can be identified when the patient is supine with the hip flexed and laterally rotated. Two exam maneuvers that have been described are Howship-Romberg sign (medial thigh pain on extension, adduction , or medial rotation of the hip) and Hannington-Kiff sign (loss of adductor reflex) and are suggestive of an obturator hernia when positive [2].
-
C.
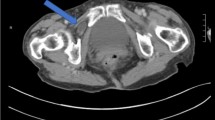
Due to the diagnostic difficulty, if physical exam findings are suggestive of obturator hernia or if clinical suspicion is high, computed tomography (CT) is considered the gold standard for diagnosis. CT scan may also provide information on bowel compromise or perforation.
-
D.
As previously described , the majority of obturator hernias are diagnosed intra-operatively when patients are taken to the operating room for a small bowel obstruction or concurrent inguinal or femoral hernia.
-
E.
Obturator hernias are associated with high mortality of 13–40%, likely due to late diagnosis, and, thus, whenever an obturator hernia is discovered, operative repair is strongly recommended [3].
-
F.
If the diagnosis is made preoperatively and strangulation is not suspected, a posterior approach is advised.
-
G.
For an open approach, a Stoppa repair or giant prosthetic reinforcement of visceral sac (GPRVS) may be performed though a lower midline or Pfannenstiel incision. A large synthetic mesh is placed in the preperitoneal space to cover the obturator orifice as well as the rest of the myopectineal orifice, including both the femoral and inguinal areas. If there is concern for bowel compromise on visual inspection, the peritoneal cavity may be entered for bowel resection.
-
H.
If surgical expertise is available, a minimally invasive (laparoscopic or robotic) approach is preferred. Either the totally extraperitoneal (TEP) or transabdominal preperitoneal (TAPP) technique may be used. In TEP , a specialized balloon is passed along the posterior rectus sheath and is used to dissect the preperitoneal space. The hernia contents are reduced, and a prosthetic mesh is used to cover the obturator orifice as well as the rest of the myopectineal orifice. The TAPP technique is performed in the same manner except that the peritoneal cavity is first entered and then the peritoneum is incised to enter the preperitoneal space. This approach is advantageous as it allows for visual inspection of the bowel to assess for viability. It is important to note that in both techniques, the mesh prosthesis should be larger than that used in traditional inguinal hernia repairs as it must cover both the inguinal and obturator spaces. If the appropriate-size mesh is not available, the mesh may be seated more inferiorly than usual to ensure proper coverage of the obturator orifice. As in the open approach, if there is suspicion for bowel compromise, the peritoneal cavity should be entered (if using the TEP technique) to assess bowel viability and perform bowel resection if necessary.
-
I.
If bowel compromise is suspected, a transabdominal approach is advised. This algorithm may also be used if the diagnosis is made intraoperatively in an abdominal operation.
-
J.
Depending on surgical expertise availability, an open lower midline laparotomy incision or laparoscopic approach may be used. The hernia sac should be reduced and the sac content inspected for viability.
-
K.
If the bowel is viable and an open approach was used, then the preperitoneal space may be entered by opening the parietal peritoneum. Once in the preperitoneal cavity, a Stoppa repair maybe performed by placing a synthetic mesh over the obturator orifice as well as the rest of the myopectineal orifice. If a laparoscopic approach was used, then the TAPP technique may be used to complete the repair by incising the peritoneum and entering the preperitoneal space.
-
L.
If the bowel is necrotic and an open approach was used, then an open bowel resection should be performed. Due to concern for infection, a synthetic mesh is not advisable in the setting of strangulation, perforation, gross contamination, or bowel resection. The hernia defect may be suture repaired in two layers [4]. Alternatively, a biologic mesh may be used or the defect may be reinforced with adjacent tissues such as periosteal flaps, bladder wall, uterine fundus, or ligaments [2]. If a laparoscopic approach was used, then a laparoscopic bowel resection may be performed if surgical expertise is available. The hernia defect then may be repaired primarily. Alternatively, a delayed mesh repair may be performed at a later date.

Algorithm 192.1
References
Stamatiou D, Skandalakis LJ, Zoras O, Mirilas P. Obturator hernia revisited: surgical anatomy, embryology, diagnosis, and technique of repair. Am Surg. 2011;77(9):1147–57.
Salameh JR. Primary and unusual abdominal wall hernias. Surg Clin North Am. 2008;88(1):45–60, viii.
Hodgins N, Cieplucha K, Conneally P, Ghareeb E. Obturator hernia: a case report and review of the literature. Int J Surg Case Rep. 2013;4(10):889–92.
Shipkov CD, Uchikov AP, Grigoriadis E. The obturator hernia: difficult to diagnose, easy to repair. Hernia J Hernias Abdominal Wall Surgery. 2004;8(2):155–7.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Hu, Q.L., Chen, D.C. (2019). Obturator Hernia. In: Docimo Jr., S., Pauli, E. (eds) Clinical Algorithms in General Surgery . Springer, Cham. https://doi.org/10.1007/978-3-319-98497-1_192
Download citation
DOI: https://doi.org/10.1007/978-3-319-98497-1_192
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98496-4
Online ISBN: 978-3-319-98497-1
eBook Packages: MedicineMedicine (R0)