Abstract
The influence of clinical and treatment factors on the risk of recurrence was analyzed from a retrospective series of 74 children and adolescents with thyroid cancer (55 girls, 19 boys; age 2–20 years). Two groups, comparable in terms of age, sex, and previous radiotherapy, were compared according to the presence (group 1) or absence (group 2) of cervical lymph nodes identified by palpation or ultrasonography. Total thyroidectomy (TT) with lymph node dissection (LND) was performed in the 19 group 1 patients, whereas in group 2 patients (n = 55) lobectomy was performed in 29, TT in 26, and LND in 7. Pathology studies showed papillary thyroid carcinoma in 95% of cases. In group 1, tumors were more frequently multifocal (89% vs. 16% in group 2), invasive with extension beyond the thyroid capsule (68% vs. 5% in group 2), and of the diffuse sclerosing variety (63% vs. 4% in group 2) (p < 0.001). With a median follow-up of 61 months, lymph node recurrence was seen in 53% of group 1 patients and in no patients in group 2. Three group 2 patients (10%) were reoperated for a local recurrence after lobectomy. Risk factors for reintervention were young age (< 15 years) (p < 0.01) and cervical lymph nodes (p < 0.001). Survivals without reintervention at 5 and 10 years were, respectively, 58% and 38% for group 1 and 94% and 90% for group 2 (p < 0.001). At the time of analysis, 68% of group 1 patients and 98% of group 2 patients were in remission. In conclusion, the presence of palpable cervical lymph nodes at diagnosis is associated with more invasive forms of malignancy and is a predictive factor of recurrence regardless of the extent of the initial surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Differentiated thyroid carcinoma is rare in young subjects and represents 0.5% to 3.0% of childhood carcinomas [1, 2, 3]. The incidence increases with age, and peak incidence is observed between 15 and 19 years of age. Thyroid cancer in children is characterized by frequent clinical aggressiveness with cervical lymph node involvement in 60% to 80% of cases and lung metastases at diagnosis in 20% of cases [4, 5, 6, 7, 8, 9, 10, 11, 12]. The prognosis remains excellent with a low rate of mortality even in advanced stages [12, 13, 14], but local recurrence is more frequent than in adults, leading to reoperation [8, 9, 10, 11].
Predictive factors of recurrence remain incompletely known, although some factors have been suggested from retrospective studies [6, 7, 8, 9, 15]. They include young age (< 16 years), lymph node involvement or distant metastases at diagnosis, and some histopathologic characteristics (mainly the diffuse sclerosing papillary variant, which is frequent in children) [16, 17, 18].
Because of the lack of randomized studies, the optimal initial surgical treatment is controversial, and the impact of the initial surgery on the outcome remains unclear. Total thyroidectomy associated with lymph node dissection is most often recommended, whatever the extent of the primary tumor, to reduce the rate of recurrence [19, 20, 21]. However, neck dissection is associated with morbidity [21, 22, 23, 24], and the impact of this strategy on patients with disease confined to the thyroid has not been determined. The present study was undertaken as a retrospective series of 74 children and adolescents with differentiated thyroid cancer to analyze the influence of the preoperative characteristics of the patients and the surgical procedures on the risk of recurrence.
Patients and Methods
Patients
A total of 74 children and adolescents (55 girls, 19 boys) underwent surgery for a differentiated thyroid cancer between 1985 and 2001 at Hôpital de l’Antiquaille, Lyon, France. At the time of the initial surgery, their median age was 17 years (range 2–20 years), with 25 patients younger than 15 years. In 12 patients (16%), previous radiotherapy had been performed for neuroblastoma in 4, acute leukemia in 3, medulloblastoma in 1, nephroblastoma in 1, cerebral tumor in 1, ethmoidal rhabdomyosarcoma in 1, and malignant histiocytosis in 1. The median age of the patients was 12 years (range 8–15 years), and the median delay from radiotherapy was 8 years (range 4–15 years).
Surgical Treatment
Total or near-total thyroidectomy was performed in 45 patients, associated with central neck dissection in 7 patients and with central and lateral neck dissection in 19 patients. Lobectomy was performed in 29 patients. The extent of the initial surgery depended on the clinical presentation. Total thyroidectomy was not performed systematically in cases of limited disease without evidence of lymph node involvement at surgery.
Histopathology
Histopathologic examination was performed by the same physician. The histologic classification was performed in accordance with the World Health Organization classification. Special attention was given to multifocality and to the presence of the diffuse sclerosing variant. The pTNM classification was used to categorize the extent of the tumor.
Follow-up
After the initial surgery, postoperative radioiodine ablation was performed in 25 patients. All patients were further submitted to l-thyroxine treatment at a suppressive dose. Clinical examination, cervical ultrasonography (US), and serum thyroglobulin measurements were performed every 3 months during the first 2 years and thereafter at least every 6 months. At the time of analysis, the median follow-up was 61 months (6–185 months), more than 5 years in 38 patients, and more than 10 years in 16 patients.
Patients were considered in remission when US demonstrated the absence of lymph node or thyroid bed recurrence and when the serum thyroglobulin concentration [immunoradiometric (IRMA) method] was less than 2 ng/ml after l-thyroxine withdrawal or undetectable under l-thyroxine treatment.
Statistical Analysis
Disease-free survival and survival without reintervention were estimated using the Kaplan-Meier method. We consider the initial time as the date of surgery. Prognostic factors of recurrence were analyzed using the mantel-Cox test. The following variables were studied: sex, age at diagnosis (≤ 15 years versus > 15 years), previous radiotherapy, and presence of lymph node metastasis at diagnosis. Differences in groups according to multifocality, histopathology, and extent of tumor were analyzed by the ċ2 test. A value of p < 0.05 was considered significant.
Results
Patients were retrospectively classified into two groups according to presentation at diagnosis. Group 1 consisted of 19 patients with cervical lymph nodes, identified preoperatively, by palpation (n = 15) or US (n = 4). Group 2 comprised 55 patients without clinical or US evidence of lymph node involvement. As shown in Table 1, there was no difference between the two groups according to sex, age, or previous radiotherapy.
Initial treatment
Total thyroidectomy associated with central and lateral cervical lymph node dissection was performed in all patients in group 1. For group 2 patients, the surgical procedure consisted of lobectomy in 29 patients, total thyroidectomy in 19 patients, and total thyroidectomy associated with central lymph node dissection in 7 patients with questionable lymph nodes at surgery. Postoperative morbidity occurred only in group 1, with laryngeal nerve palsy in three patients (4% of the whole series) (due to deliberate surgical resection in one patient) and hypocalcemia in one patient (1.4% of the whole series). Postoperative radioiodine ablation was performed in 16 group 1 patients and in 9 group 2 patients. In four patients belonging to group 1, lung metastases were found at radioactive iodine whole-body scan, leading to iterative 131I therapy; three of these patients were younger than 15 years.
Histopathology
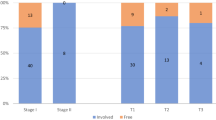
Histopathology showed papillary thyroid carcinoma in the 19 group 1 patients and in 52 of the 55 group 2 patients. As shown in Table 2, tumors of both groups differed in extent and aggressiveness. In group 1 patients, they were more frequently multifocal (p < 0.001), of the diffuse sclerosing variety (p < 0.001), and invasive with extrathyroidal involvement (p < 0.001). In group 2, pT1 and pT2 were more represented, including eight of nine microcarcinomas. Lymph node invasion was present in the 19 group 1 patients and in 4 of the 7 group 2 patients who underwent lymph node dissection (p < 0.002).
Follow-up
The median follow-up was 61 months and did not differ between the two groups. Lymph node recurrence was seen in 10 of the 19 group 1 patients (53%), leading to reoperation surgery in 9 patients (associated with complementary 131I therapy in 8) and to 131I therapy alone in a single patient. Recurrences occurred in seven patients during the first postoperative year. The two other children were reoperated at 36 and 102 months, respectively. In one child, reoperative surgery was performed at 12, 21, and 54 months. Lymph node recurrences were seen mostly in younger patients; in fact, 87.5% of group 1 patients younger than 15 years had to be reoperated versus 27% of group 1 patients older than 15 years of age (p < 0.001).
No patient in group 2 presented with lymph node recurrence. Among the 29 patients for whom lobectomy had been performed, 3 patients (10%) with a carcinoma diameter ranging from 21 to 37 mm, had a recurrence in the contralateral thyroid lobe, leading to surgery at 33, 54, and 82 months, respectively. Two of these three patients were older than 15 years.
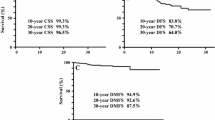
Risk factors for reintervention, identified by univariate analysis, were age [with more interventions in patients < 15 years than patients ≥ 15 years (p < 0.01)] and initial presence of lymph nodes (p < 0.001) (Table 3). There was no influence of sex or previous radiotherapy. Disease-free survivals at 5 and 10 years were, respectively, 58% and 38% for group 1 and 94% and 90% for group 2 (Fig. 1).
All patients were alive at the time of analysis, with 68% of group 1 patients and 98% of group 2 patients disease-free. Persistent disease was observed in six patients of group 1, four of whom were the patients with lung metastases. Stabilization of computed tomography (CT)-scanned lesions was obtained in two cases after 500 to 900 mCi of 131I. In the two other patients, iodine whole-body scans were negative after two courses of 131I, but the thyroglobulin level remained elevated, at 150 and 40 µg/ml, respectively, after l-thyroxine withdrawal. In the remaining two patients, with the thyroglobulin level at 11 and 12 ng/ml, respectively, persistent disease was related to lymph node metastases despite reoperative surgery and 131I treatment.
Only one patient in group 2 had persistent disease. He had undergone a total thyroidectomy with positive central neck dissection and radioiodine ablation for a diffuse sclerosing variant of papillary thyroid cancer. His serum thyroglobulin remained elevated at 21 µg/ml (normal less than 2 µg/ml) without any radioiodine uptake site or lesionat conventional imaging.
Discussion
Thyroid cancer in children is characterized by clinical aggressiveness with local recurrence in 20% to 30%, leading to reoperative surgery, radioiodine ablation, or both [19, 20, 21, 22, 23, 25, 26]. However, the prognosis remains excellent, with 90% to 95% survival at 20 years [12, 13, 14] and 70% to 80% disease-free survival at 5 years [7, 9, 11, 20, 22, 26]. Accordingly, in the present large retrospective series, no patient died and 90% of children were in remission after a median follow-up of 61 months; 14% of patients had a lymph node recurrence. Some authors have suggested the need for extensive treatment with total thyroidectomy plus lymph node dissection in all patients to reduce the rate of recurrence. A favorable outcome has been reported in short, uncontrolled studies using this strategy [19, 20, 23]. However, because all patients were similarly treated, the impact of treatment on disease confined to the thyroid could not be evaluated. Moreover, extensive lymph node dissection has been associated with not insignificant postoperative morbidity [4, 11, 21, 22, 23, 24].
Our hypothesis was that surgical treatment may be adapted, based on the preoperative characteristics of patients, with the objective of reducing the rate of recurrence while limiting postoperative morbidity. Lymph node invasion has been reported in 60% to 80% of young patients and has been suggested to be a predictive factor of recurrence [6, 7, 8, 10, 11, 26, 27]. Thus in the present study, patients were classified according to the presence of lymph nodes preoperatively identified by palpation or US. The surgical strategy depended on the clinical presentation (i.e., extensive in patients with lymph nodes present and more limited in patients without preoperative evidence of cervical lymph node metastasis). Our results clearly show that clinical presentation is related to the severity of the disease. Indeed, of 19 patients with palpable or US-detected lymph nodes at the time of diagnosis, 20% presented with lung metastases, 53% had lymph node recurrence leading to reoperative surgery, and 30% had persistent disease at the time of analysis. In contrast, despite more limited surgery in group 2, no patient presented with lymph node recurrence, only 10% of patients had to be reoperated for a contralateral recurrence after partial thyroidectomy, and 98% were in remission.
The fact that only 25% of patients were classified as group 1 mainly reflects the fact that our classification does not take into account histologic invasion. Only 7 of the 55 group 2 patients underwent neck dissection; and the 4 patients of this group with microscopic lymph node invasion remained classified as group 2 based on their preoperative presentation. Clinical presentation may reflect an evolving form or a difference in the extent and aggressiveness of tumors. Group 1 patients exhibited a higher frequency of extrathyroidal involvement, multifocality, and presence of the diffuse sclerosing papillary variant.
All of these factors have been clearly identified as predictors of recurrence in young patients [6, 7, 8, 9, 10, 18], especially, the diffuse sclerosing variant of papillary carcinoma, which is more frequently observed in children than adults and is associated with aggressive behavior [1, 16, 17, 18]. In our study, the 13 patients with the diffuse sclerosing variant also had lymph node invasion, and 2 had lung metastases. Other risk factors for recurrence have been suggested from retrospective studies. Previous radiotherapy is known to increase the risk of thyroid cancer in children but, in keeping with our results, does not influence the prognosis [28]. A number of studies have noted the high rate of recurrence in children less than 15 years of age [5, 15, 26]. It has been suggested that young age is associated with more extensive forms of thyroid cancer [15]. This was not the case in the present study, as young patients are equally distributed between the two groups. However, recurrences were mostly observed in the youngest patients of group 1, as 87% experienced a recurrence. In contrast, in group 2 there is no difference in the recurrence rate as a function of age. Thus particular attention must be given to treatment of young patients with preoperative cervical lymph node invasion.
Because of the low prevalence of thyroid cancer in children, prospective clinical trials are difficult to perform, and the optimal surgical treatment remains a matter of discussion. Most studies have included a limited number of patients, heterogeneous in terms of severity of the disease. In some, the better predictor of recurrences is the extent of the initial surgical treatment [19, 20, 21, 22, 25, 26]. For instance, in the large study by Jarzab et al. [23] total thyroidectomy was associated with 97% survival, whereas lobectomy led to a 59% recurrence rate at 5 years. In contrast, Alessandri et al. [15] suggested that there is no relation between the extent of surgery and the evolution of the disease. In the study by Newman et al. [14], where surgical extent was adapted to the clinical conditions of these patients, with more extensive surgery in high risk patients, progressive disease-free survival rates were the same after lobectomy or more extensive procedures. Moreover, Ben Arush et al. [29] recommended performing lymph node dissection only in patients with palpable lymph nodes.
Comparably, in the present series, total thyroidectomy associated with lymph node dissection was performed only in patients with suspicious lymph nodes. Thus extensive surgery was performed in all group 1 patients, whereas in group 2 lobectomy was performed in somewhat more than half of the patients and lymph node dissection in only 15% of patients with questionable lymph nodes at surgery. Despite the fact that the extent of the initial surgery was more limited in group 2 patients, the disease-free survivals at 5 and 10 years were significantly greater than for group 1 patients. No group 2 patient had to be reoperated for a lymph node recurrence, although microscopic involvement was present in a number of cases. Three patients underwent reoperative surgery for contralateral recurrence after lobectomy. No patient who underwent total thyroidectomy developed a recurrence.
This suggests that the presence of clinical lymph nodes at diagnosis is a strong predictive factor of recurrence. In the present study, they occurred mostly during the first year, suggesting persistent disease in relation to incomplete lymph node dissection due to technical limitations. Lymph node dissection, as extensive as possible, is necessary, especially in the younger patients, who are more prone to recurrence. In these patients, radioiodine ablation is performed to ablate residual thyroid tissue and any microscopic foci.
In contrast, in patients with disease confined to the thyroid, total thyroidectomy without lymph node dissection may be sufficient to prevent local and lymph node recurrence if there is no evidence of suspicious lymph nodes at surgery. Such a conservative strategy limits morbidity in these patients because, in accordance with previous studies [20, 21, 22], postoperative morbidity is low (5% of cases in the present series) and is observed only in patients who undergo extensive lymph node dissection. Intraoperative frozen section examination is widely indicated for the diagnosis of questionable lymph nodes. The interest of peroperative ultrasonography and sophisticated radioisotopic techniques that may provide additional information regarding the decision of whether to perform extensive dissection must be evaluated.
Résumé
L’impact de la présentation clinique et de l’étendue du geste chirurgical sur le risque de récidives a été analysé rétrospectivement chez 74 enfants et adolescents présentant un cancer thyroïdien (55 filles, 19 garçons; âge: 2–20 ans). Deux groupes, comparables pour l’âge, le sexe et les antécédents de radiothérapie, ont été constitués en fonction de la présence (groupe 1) ou de l’absence (groupe 2) d’adénopathies cervicales identifiées par la palpation ou l’échographie pré opératoire. Une thyroïdectomie totale avec curage ganglionnaire a été réalisé chez les 19 patients du groupe 1, alors que dans le groupe 2 (n = 55) une lobectomie a été pratiquée chez 29 patients, une thyroïdectomie totale chez 26 et un curage ganglionnaire chez 7. L’histologie a mis en évidence un carcinome papillaire dans 95% des cas. Les tumeurs du groupe 1 étaient plus fréquemment multifocales, invasives et du type sclérosant diffus (p < 0.001). Au cours d’un suivi médian de 61 mois, une récidive ganglionnaire est survenue chez 53% des patients du groupe 1 et aucun patient du groupe 2. Trois patients du groupe 2 (10%) ont été réopérés pour une récidive controlatérale après lobectomie. Les facteurs de risque de réintervention étaient le jeune âge (< 15 ans) (p < 0.01) et la présence d’adénopathies cervicales (p < 0.001). La survie sans réintervention à 5 et 10 ans était respectivement, de 58 et 38% dans le groupe 1 et de 94 et 90% dans le groupe 2 (p < 0.001). Au moment de l’analyse, 68% des patients du groupe 1 et 98% des patients du groupe 2 étaient en rémission. En conclusion, la présence d’adénopathies cervicales est associée à des formes plus agressives de cancer thyroïdien et constitue un facteur de risque de récidive quelle que soit l’étendue du geste chirurgical initial.
Resumen
La influencia de factores de orden clínico y terapéutico sobre el riesgo de recurrencia fue investigada en una serie retrospectiva de 74 niños y adolescentes con cáncer tiroideo (55 niñas, 19 muchachos, con edades 2–20 años). Se compararon dos grupos similares en términos de edad, sexo o radioterapia previa, según la presencia (grupo I) o la ausencia (grupo II) de ganglios linfáticos, identificados por palpación o ultrasonografía. Se practicó tiroidectomía total (TT) con disección ganglionar (DG) en los 19 pacientes del grupo I, en tanto que en el grupo II (n = 55) se practicó lobectomía en 29, TT en 26 y DG en 7. El estudio de patología reveló carcinoma papilar en 95% de los casos. En el grupo I los tumores fueron más frecuentemente multifocales (89% vs. 16% en el grupo 2), invasor con extensión más allá de la cápsula (68% vs. 5% en el grupo 2) y de la variedad esclerosante difusa (63% vs 4% en el grupo 2) (p < 0.001). Con una media de seguimiento de 61 meses se presentó recurrencia ganglionar en 53% de los pacientes del grupo 1 y en ningún paciente del grupo 2. Tres del grupo 2 (10%) fueron reoperados por recurrencia local luego de lobectomía. Los riesgos de reintervención fueron la edad joven (< 15 años) (p < 0.01) y los ganglios cervicales (p < 0.001). La supervivencia sin reintervención a los 5 y 10 años fue 58% y 38% en el grupo 1 y 94% y 90% en el grupo 2, respectivamente (p < 0.001). En el momento del análisis, 68% de los pacientes del grupo 1 y 98% del grupo 2 se encontraban en remisión. En conclusión, los ganglios palpables en el momento del diagnóstico se asocian con formas más invasoras del neoplasma y constituyen un factor predictor de recurrencia no importa cual sea la extensión de la cirugía.
References
W Hung NJ Sarlis (2002) ArticleTitleCurrent controversies in the management of pediatric patients with well-differentiated nonmedullary thyroid cancer: a review Thyroid 12 683–702 Occurrence Handle10.1089/105072502760258668 Occurrence Handle12225637
HR Harash ED William (1995) ArticleTitleChildhood thyroid cancer in England and Wales Br. J. Cancer 72 777–783 Occurrence Handle7669594
P Bucsky T Parlowsky (1997) ArticleTitleEpidemiology and therapy of thyroid cancer in childhood and adolescence Exp. Clin. Endocrinol. Diabetes 105 70–73 Occurrence Handle1:CAS:528:DyaK2sXnvVygt7w%3D
R Feinmesser E Lubin K Segal et al. (1997) ArticleTitleCarcinoma of the thyroid in children: a review J. Pediatr. Endocrinol. Metab. 10 561–568 Occurrence Handle1:STN:280:DyaK1c7ivVWkug%3D%3D Occurrence Handle9467125
M Schlumberger F Vathaire ParticleDe JP Travagli et al. (1987) ArticleTitleDifferentiated thyroid carcinoma in childhood: long term follow-up of 72 patients J. Clin. Endocrinol. Metab. 65 1088–1094 Occurrence Handle1:STN:280:BieD2MbkvFQ%3D Occurrence Handle3680475
J Farahati P Bucsky T Parlowsky et al. (1997) ArticleTitleCharacteristics of differentiated thyroid carcinoma in children and adolescents with respect to age, gender and histology Cancer 80 2156–2162 Occurrence Handle10.1002/(SICI)1097-0142(19971201)80:11<2156::AID-CNCR16>3.0.CO;2-Y Occurrence Handle1:STN:280:DyaK1c%2Flt1agsA%3D%3D Occurrence Handle9392339
MP Quaglia ParticleLa T Black GW Holcomb et al. (2000) ArticleTitleDifferentiated cancer: clinical characteristics treatment and outcome in patients under 21 years of age who present with distant metastases; a report from the Surgical Discipline Committee of the Children’s Cancer Group J. Pediatr. Surg. 35 955–959 Occurrence Handle10.1053/jpsu.2000.6935 Occurrence Handle10873043
PW Grigsby A Gal-or JM Michalsky et al. (2002) ArticleTitleChildhood and adolescent thyroid carcinoma Cancer 95 724–729 Occurrence Handle10.1002/cncr.10725 Occurrence Handle12209714
CA Welch Dinauer RM Tuttle DK Robie et al. (1998) ArticleTitleClinical features associated with metastasis and recurrence of differentiated thyroid cancer in children, adolescents and young adults Clin. Endocrinol. (Oxf.) 49 619–628 Occurrence Handle10.1046/j.1365-2265.1998.00584.x Occurrence Handle1:STN:280:DyaK1M3ht1yhtQ%3D%3D
R Vassilopoulou-Sellin H Goepfert B Raney et al. (1998) ArticleTitleDifferentiated thyroid cancer in children and adolescents: clinical outcome and mortality after long term follow-up Head Neck 20 549–555 Occurrence Handle10.1002/(SICI)1097-0347(199809)20:6<549::AID-HED10>3.0.CO;2-R Occurrence Handle1:STN:280:DyaK1czmsl2hsg%3D%3D Occurrence Handle9702543
AM Samuel B Rajashekharrao DH Shah (1998) ArticleTitlePulmonary metastases in children and adolescents with well-differentiated thyroid cancer J. Nucl. Med. 39 1531–1536 Occurrence Handle1:STN:280:DyaK1cvhsFGrtA%3D%3D Occurrence Handle9744337
JS Brink JA Heerden Particlevan B McIver et al. (2000) ArticleTitlePapillary thyroid cancer with pulmonary metastases in children: long term prognosis Surgery 128 881–886 Occurrence Handle10.1067/msy.2000.109728 Occurrence Handle1:STN:280:DC%2BD3M%2FnsFegtA%3D%3D Occurrence Handle11114619
NJ Beasley J Lee S Eski et al. (2002) ArticleTitleImpact of nodal metastases on prognosis in patients with well differentiated thyroid cancer Arch. Otolaryngol. Head Neck Surg. 128 825–828 Occurrence Handle12117344
KD Newman T Black G Heller et al. (1998) ArticleTitleDifferentiated thyroid cancer: determinants of disease progression in patients < 21 years of age at diagnosis: a report from the Surgical Discipline Committee of the Children’s Cancer Group Ann. Surg. 227 533–541 Occurrence Handle10.1097/00000658-199804000-00014 Occurrence Handle1:STN:280:DyaK1c3itlSjtA%3D%3D Occurrence Handle9563542
AJ Alessandri KJ Goddard GK Blair et al. (2000) ArticleTitleAge is the major determinant of recurrence in pediatric differentiated thyroid carcinoma Med. Pediatr. Oncol. 53 41–46 Occurrence Handle10.1002/1096-911X(200007)35:1<41::AID-MPO7>3.3.CO;2-Z
C Arici O Erdogan H Altunbas et al. (2002) ArticleTitleDifferentiated thyroid cancer in children and adolescents: clinical characteristics, treatment and outcome of 15 patients Horm. Res. 57 153–156 Occurrence Handle10.1159/000058375 Occurrence Handle1:CAS:528:DC%2BD38XksVygsbs%3D Occurrence Handle12053086
D Giuffreda C Scollo G Pellegretti et al. (2002) ArticleTitleDifferentiated thyroid cancer in children and adolescents J. Endocrinol. Invest. 25 18–24 Occurrence Handle11883862
U Hallwirth J Flores K Kaserer et al. (1999) ArticleTitleDifferentiated thyroid cancer in children and adolescents: the importance of adequate surgery and review of the literature Eur. J. Pediatr. Surg. 9 359–363 Occurrence Handle1:STN:280:DC%2BD3c7isFCrtw%3D%3D Occurrence Handle10661843
CA Welch Dinauer M Tuttle DK Robie et al. (1999) ArticleTitleExtensive surgery improves recurrence-free survival for children and young patients with class I papillary thyroid carcinoma J. Pediatr. Surg. 34 1799–1804 Occurrence Handle10.1016/S0022-3468(99)90316-0 Occurrence Handle1:STN:280:DC%2BD3c%2FptVartg%3D%3D Occurrence Handle10626858
K Segal J Shvero Y Stern et al. (1998) ArticleTitleSurgery of thyroid cancer in children and adolescents Head Neck 20 293–297 Occurrence Handle10.1002/(SICI)1097-0347(199807)20:4<293::AID-HED2>3.0.CO;2-U Occurrence Handle1:STN:280:DyaK1c3kvVWitg%3D%3D Occurrence Handle9588700
T Steinmuller J Klupp S Wenkings et al. (1999) ArticleTitleComplications associated with different surgical approaches in differentiated thyroid carcinoma Arch. Surg. 384 50–53 Occurrence Handle1:STN:280:DyaK1M3psVSmsg%3D%3D
JW Haveman KM Tol Particlevan CW Rouwe et al. (2003) ArticleTitleSurgical experience in children with differentiated thyroid carcinoma Ann. Surg. Oncol. 10 15–20 Occurrence Handle10.1245/ASO.2003.03.002 Occurrence Handle12513954
B Jarzab DH Handkiewicz Junak J Wloch et al. (2000) ArticleTitleMultivariate analysis of prognostic factors for differentiated thyroid carcinoma in children Eur. J. Nucl. Med. 27 833–841 Occurrence Handle10.1007/s002590000271 Occurrence Handle1:STN:280:DC%2BD3M%2Fot1aqsA%3D%3D Occurrence Handle10952495
APM Stael JT Plukker DA Piers et al. (1995) ArticleTitleTotal thyroidectomy in the treatment of thyroid carcinoma in childhood Br. J. Surg. 82 1083–1085 Occurrence Handle1:STN:280:ByqA2snitVA%3D Occurrence Handle7648159
S Ortiz JM Rodriguez P Parrilla et al. (2001) ArticleTitleRecurrent papillary thyroid cancer: analysis of prognostic factors including the histological variant Eur. J. Surg. 167 406–412 Occurrence Handle10.1080/110241501750243734 Occurrence Handle1:STN:280:DC%2BD38%2FisFCktw%3D%3D Occurrence Handle11471663
J Soares E Limbert M Sobrinho-Somoes (1989) ArticleTitleDiffuse sclerosing variant of papillary thyroid carcinoma Pathol. Res. Pract. 185 200–206 Occurrence Handle1:STN:280:By%2BD3MjgsFM%3D Occurrence Handle2798220
ML Carcangiu G Zampi A Pupi et al. (1985) ArticleTitlePapillary thyroid carcinoma of the thyroid: a clinicopathologic study of 241 cases treated at the University of Florence, Italy Cancer 55 805–828 Occurrence Handle1:STN:280:BiqD1MfpsVw%3D Occurrence Handle3967175
S Acharya K Sarafoglu M Quaglia ParticleLa et al. (2003) ArticleTitleThyroid neoplasms after therapeutic radiation for malignancy during childhood and adolescence Cancer 97 2397–2403 Occurrence Handle10.1002/cncr.11362 Occurrence Handle12733137
MW Arush ParticleBen ME Stein M Perez Nahum et al. (2000) ArticleTitlePediatric thyroid carcinoma: 22 years of experience at the Northern Israel Oncology center (1973-1995) Pediatr. Hematol. Oncol. 17 85–92
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Borson-Chazot, F., Causeret, S., Lifante, JC. et al. Predictive Factors for Recurrence from a Series of 74 Children and Adolescents with Differentiated Thyroid Cancer . World J. Surg. 28, 1088–1092 (2004). https://doi.org/10.1007/s00268-004-7630-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-004-7630-y