Abstract
Thyroid cancer is the most common malignancy in the endocrine system. Papillary thyroid carcinoma (PTC) is the most common differentiated thyroid cancer. There are considerable discrepancies regarding the role and extent of prophylactic central lymph node dissection (PCLND) for patients with PTC. Our primary goal was the evaluation of CLN involvement based on the tumor features and staging on the eight version of the American Joint Committee on Cancer and also the TNM method. Our secondary aim was to evaluate the features of the CLNs with tumoral features and also features associated with the development of transient hypoparathyroidism. This prospective case-controlled study was performed among PTC patients. Total thyroidectomy and bilateral dissection of the CLNs of the central compartment of the neck was performed, and samples were sent for pathological evaluation. CLN involvement, tumoral features and transient hypoparathyroidism were cross-evaluated and analyzed with SPSS version 26.0. In this study, out of 61 patients, 11 (18%) were male, the average age was 37.3 ± 13.7 years, based on AJCC staging, 53 (86.9%) were stage I and 8 (13.1%) were stage II, and based on TNM staging, 39 patients (66.1%) were T1, including 13 (22.0%) T1a and 26 (44.1%) T1b, 15 patients (25.4%) were T2, and five patients (8.5%) were T3. Based on permanent pathology evaluation, the majority of patients (n = 48; 78.7%) had CLN involvement. None of the preoperative and tumor features had a significant association with CLN involvement. 75% of stage I and 100% of stage two cases, while 76.9% of T1, 86.7% of T2, and 80.0% of T3 cases had CLN involvement. There was no significant association between the involvement of CLN and the AJCC staging (P = 0.184) or TNM staging (P = 0.875). The involved to dissected CLN ratio was significantly higher in stage II patients compared to stage I (72.5 vs. 34.8%; P = 0.006), and also with higher T staging (0.009). There was a statistically significant association between the larger CLN size and older patients’ age, higher postoperative thyroglobulin levels, and smaller tumor size. Higher postoperative thyroglobulin level was significantly associated with larger tumors size and thyroid capsule invasion. Also, 26 (44.8%) of patients developed transient hypoparathyroidism, which was significantly associated with vascular invasion (P = 0.048), bilateral location of tumor (P = 0.048) or on the right side (0.005), and larger size of the tumor (P = 0.016). Tumor features and staging were not associated with CLN involvement features. Therefore, full extent PCLND should be carried out to avoid reoperation or metastasis in PTC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer is the most common malignancy of the endocrine system, which is divided into different histological types [1], in which Papillary thyroid carcinoma (PTC) is the most common type and accounts for about 80% of all thyroid malignant neoplasm [2]. Although PTC has a great prognosis, it is also characterized with high tendency to spread to central lymph node (CLN) [3]. The incidence rate of central lymph node metastasis ranges from 40 to 90% in all patients with PTC and 20 to 40% in clinically node negative (cN0) PTC patients [4, 5]. It has been reported that CLN metastasis is associated with increased recurrence rate; however, according to many studies lymph node (LN) involvement does not affect the mortality rate of PTC patients [6, 7].
Prophylactic central lymph node dissection (PCLND) is defined as removing central neck compartment LNs when there is no evidence of pathologic lymphadenopathy in preoperative or intraoperative evaluation [8]. At present, central lymph node dissection (CLND) is recommended for PTC patient who are suspicious of CLN metastasis in pre-op evaluation, but PCLND in cN0 patients is a great controversial matter. According to some studies PCLND will result in lower recurrence rates and a more precise staging of the tumor which could later affect our therapeutic choices and managements [9, 10]. American thyroid association (ATA) guideline suggested that PCLND be considered for PTC patients especially in advanced stages (T3 and T4) [11]. On the other hand, some studies do not recommend routinely performing PCLND due to potential complications including hypoparathyroidism, laryngeal nerve injury and chyle leakage [12, 13]. Therefore, PCLND in cN0 PTC patients is now considered an endocrinological debate which require further investigations.
Most endocrine surgeons agree that compartment-based LN dissection is an appropriate and effective treatment for large LNs that can be detected by preoperative imaging or physical examination or during surgery by observation or touch. However, there is a considerable discrepancy regarding the role of PCLND for patients with PTC [14]. Studies have shown that Ipsilateral CLND can be a good alternative to bilateral CLND in PTC cases with clinically negative LNs because its short-term oncological outcome is similar to bilateral CLND and the risk of complications is lower [15,16,17,18,19].
Therefore, this study was carried out to identify the incidence rate of CLN metastasis and the effectiveness of PCLN in cN0 PTC patients based on permanent pathology result, which were categorized based on the eight version of American Joint Committee on Cancer (AJCC) and TNM staging method. We analyzed the features of PTC and the patients based on CLNs involvement. The relationship between postoperative serum thyroglobulin and the features of the tumor was also investigated. The incidence rate of transient hypoparathyroidism following the surgery and factors associated with its development were assessed as well. We also intend to investigate the pathology results obtained from samples sent from LNs removed from bilateral CLND patients with PTC undergoing thyroidectomy and the relationship between the LNs on the involved side with the tumor features, and whether unilateral CLND can be appropriate and sufficient for patients with PTC cancer. The results of our study aim to give better guidance in the surgical and therapeutical management of PTC patients.
Materials and methods
Study design
This prospective cohort study was conducted among patients referring to Shariati Hospital, in which PTC was confirmed by Fine Needle Aspiration Biopsy. All patients underwent physical examination and ultrasonography for the presence of LN. The exclusion criteria included a previous history of surgery or neck radiation and the presence of palpable lateral LN on physical examination or detected on preoperative ultrasound.
Pre-operative evaluation
A complete clinical history and physical examination were obtained from the patients and they were evaluated for the presence of palpable cervical LNs. A chest X-ray was also performed for evidence of pulmonary metastasis, and cervical ultrasound (by a single radiologist) was performed to determine the presence of LNs in the central and lateral cervical compartments.
Surgical intervention
After preparing the necessary measures and induction of general anesthesia, a standard transverse neck incision was made. Total thyroidectomy with parathyroids preservation was performed. Patients then underwent bilateral CLND [20,21,22], including Level VI and VII thyroid tissue, along with all the removed LNs, including both sides of the central compartment, were labeled for permanent pathological evaluation of metastasis, multifocal tumor, and capsular or extracapsular extension of the tumor, and also the correspondence between the location of the primary tumor and the metastatic site (ipsilateral or contralateral). The size and location of the primary tumor and the size of the largest LNs in the ipsilateral and central contralateral compartments were also recorded based on pathology tissues. A single-blinded pathologist examined thyroid tissue and dissected LN samples after staining with hematoxylin–eosin (H & E) using a 40% objective lens.
Postoperative evaluation
All patients were evaluated for dysphonia by the surgeon after surgery. Transient hypoparathyroidism was also documented as a postoperative complication in patients with serum calcium levels of less than 8 mg/dL during the first 24 h after surgery. Furthermore, blood samples were obtained three months after surgery while levothyroxine was halted for patients to measure serum thyroglobulin levels.
Outcome evaluation
Our primary goal was the evaluation of CLN involvement based on the current guidelines and protocols. Therefore, we categorized our cases based on the eight version of the American Joint Committee on Cancer (AJCC) [23] and also the TNM staging method. Our secondary aims were to evaluate the features of the CLNs with tumoral features and also features associated with the development of transient hypoparathyroidism.
Statistical analysis
The data were entered into SPSS software version 26 and based on the laboratory and pathology results, postoperative complications, and serum thyroglobulin, and the dose of radioactive iodine was evaluated using statistical tests. Data analysis was performed using descriptive and inferential statistics. Quantitative data were described as mean ± standard deviation, and qualitative data as frequency and relative frequency. The Chi-Square test was used to compare the frequency of qualitative variables. To compare the means of quantitative variables, if the distribution was normal based on the Kolmogorov–Smirnov test, Independent Samples T tests, or One-way ANOVA, and if the distribution was not normal, non-parametric tests (Mann–Whitney test and Kruskal–Wallis’s test, respectively) were used. The sample size was estimated based on a study by Takami et al. [24] and Roh et al. [25], considering an 80% incidence of central compartment LN involvement in patients with non-LN PTC, clinically identified on physical examination or ultrasound report, α = 0.05 and accuracy of 0.1, the final sample size was calculated as 61 participants.
Ethical considerations
The study objectives were explained to the patients, and written informed consent was obtained from them or their legally authorized representatives before their participation. Patients were reassured that their dissatisfaction with participating in the study would not interfere with their treatment. Attempts were made to observe the patients’ rights as well as the principle of confidentiality. The study was approved by the ethics committee of the Tehran University of Medical Sciences (IR.TUMS.REC.1394.1972). It was conducted in compliance with local regulatory requirements, Good Clinical Practice (GCP), and the Declaration of Helsinki [26].
Results
Out of 61 patients with PTC, 11 (18%) were male and the average age was 37.3 ± 13.7 years. Also, based on AJCC staging, 53 (86.9%) were stage I and 8 (13.1%) were stage II. Based on TNM staging, 39 patients (66.1%) were T1, 15 patients (25.4%) were T2, and five patients (8.5%) were T3. After operation and evaluation, the majority of patients, including 48 (78.7%), had CLN involvement. Table 1 demonstrates preoperative PTC features of our patients based on CLN involvement. As demonstrated, none of the preoperative and tumoral features had a significant association with CLN involvement. Also, there were no pathological changes in the thymus and parathyroid biopsies in our study.
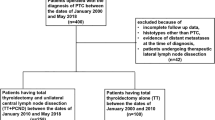
As demonstrated in Table 1 and Fig. 1, 75% of stage I and 100% of stage two cases had CLN involvement. However, 24.5% of stage I cases had no CLN involvement. There was no significant association between the involvement of CLN and the AJCC staging. (P = 0.184) Also, 76.9% of T1, 86.7% of T2, and 80.0% of T3 cases had CLN involvement, without any significant association (P = 0.875) (Fig. 1).
As demonstrated in Table 2, there was no significant difference among the total number of dissected CLNs in the patients; however, the number of involved CLNs were significantly higher in T2 compared to T1 size tumor patients. Also, the involved to dissected CLN ratio was significantly higher in stage II patients compared to stage I (72.5 vs. 34.8%). Based on the tumor size, an increase from T1 to T3 was significantly associated with higher involved to dissected CLN ratio.
Our secondary evaluations were regarding the CLN features and patients’ features. Regarding the size of CLN, there was a statistically significant association between the larger CLN size of the CLN and the older patients’ age (correlation coefficient = 0.827 and 0.684; P value < 0.001 and < 0.001 for right and left CLN, respectively), higher postoperative thyroglobulin levels (Pearson correlation; P value = 0.021; 0.874 and 0.018; 0.893, for right and left, respectively), and smaller tumor size (Correlation coefficient; P value = − 0.006; 0.965 and − 0.159; 0.220 for right and left, respectively). However, the size of CLN had no significant association with the patients’ gender (P = 0.069 and 0.055 for right and left side, respectively), and the tumor’s location (P values = 0.844 for right, 0.512 for left, 0.744 bilateral, and 0.464 for isthmus) (Table 3).
When evaluating the lateralization of the tumor with the involved CLN side, our results showed no significant association between right side tumor and the involvement of right-side CLN (P=0.728), but a significant association with the left-side and bilateral CLN involvement (P=0.009 and 0.019, respectively). Regarding left-side tumor involvement, there was no significant association with right-side, left-side, or bilateral CLN involvement (P=0.536, 0.256, and 0.500, respectively). In bilateral tumor involvement, no significant association was achieved with right-side, left-side, or bilateral CLN involvement (P=0.344, 0.163, and 0.171, respectively) (Table 4).
Also, the relationship between lymphatic involvement in the central compartment of the neck and the primary tumor characteristics was determined. It was found that there is no association between CLN involvement and tumoral features including multifocal tumor (n= 5, P=0.337), Intra/extracapsular invasion (n = 1, P=0.05), vascular invasion (n=2, P=0.602), tumor size (1.90±1.18 vs. 2.03±1.15, for positive vs. negative CLN involvement, respectively; P=0.741), and post-op thyroglobulin (0.80 vs. 0.65ng/ml for positive vs. negative CLN involvement, respectively; Pearson correlation=0.746).
Postoperative thyroglobulin level was significantly associated with tumors size category, in which a significant increase in thyroglobulin was observed from T1 to T3 type patients. (P=0.002) The amount of thyroglobulin in T2 and T3 tumors was higher than in T1 tumors, and this amount was statistically significant (P = 0.018). But statistical analysis comparing thyroglobulin levels did not show a significant difference between T2 and T3 (P = 0.875). Also, post-op thyroglobulin levels had no significant association with location of tumor (P=0.12); multifocality of tumor (P=0.520); extracapsular invasion (P=0.871); transient hypoparathyroidism (P=0.060); however, there was a significant association with size of tumor (Pearson correlation= 0.266; P=0.046), thyroid capsule invasion (1.31 vs 0.47 for positive vs negative; P=0.028).
Following CLND in patients with PTC, it was found that 26 (44.8%) of patients developed transient hypoparathyroidism and 32 patients (55.2%) had no hypo parathyroid complications. There was no significant association between transient hypoparathyroidism and the tumors size or staging. However, hypoparathyroidism was significantly associated with vascular invasion (P=0.048), bilateral location of tumor (P=0.048) or on the right side (0.005), and larger size of the tumor (P=0.016) (Table 5).
Discussion
Based on the controversies regarding the extent of CLND, especially among inexperienced surgeons, and the chance of nerve or extensive tissue damage, we conducted this study to evaluate the relationship between CLN involvement and tumoral features. As demonstrated, none of the preoperative and tumor features had a significant association with CLN involvement. Also, CLN involvement had no significant association with the features when categorized by AJCC or TNM criteria. Only higher T staging was associated with higher capsular invasion and thyroglobulin levels. Therefore, based on our results, we believe that preoperative prediction of CLN involvement based on current criteria and guidelines is not accurate and further large database and multicentral studies are required to obtain more detailed conclusions into this matter. On the other hand, based on permanent pathological evaluation, the majority of patients, including 48 (78.7%), had CLN involvement. Based on our study, 75% of stage I and 100% of stage two case, and also 76.9% of T1, 86.7% of T2, and 80.0% of T3 cases had CLN involvement. Furthermore, the involved to dissected CLN ratio was significantly higher in stage II patients compared to stage I (72.5 vs. 34.8%), and also with higher T staging. Although no statistically significance was achieved between CLN involvement and tumor staging, the clinical importance and high CLN metastatic rate cannot be overlooked and we believe that this high involvement rate justifies the necessity of PCLND, even in low staging tumors.
PCLND is generally indicated to prophylactically remove occult metastasis to reduce recurrence and possible morbidity from reoperation. Also, PCLND is utilized to plan adjuvant radioiodine (RAI) therapy through accurately assessing the pathologic stage, and allow for circumvention of succeeding routine RAI therapy for clinically unknown nodes of the neck through confirmation of cN0 of the neck [27, 28] PCLND may also have a role in patients with aggressive primary tumors or higher risk primary tumors, such as those with extrathyroidal extension (T3 or T4) or diffuse sclerosing, insular, or poorly differentiated tumors. [29] Oh et al. showed that even when preoperative work up revealed a cN0 neck, male sex and young age (40 years) were more frequently found to have large-volume lymph node metastasis [30]. PCLND was also advised in a consensus report by the European Society of Endocrine Surgeons for patients with larger tumors (T3 or T4), those who were older than 45 or younger than 15, men, patients with bilateral or multifocal tumors, or those who had known lateral cervical neck disease [31]. Reduce recurrence is another reason to perform PCLDN during primary surgery, as shown by a recent meta-analysis that found PCLND with thyroidectomy appears to significantly lower locoregional recurrence compared with total thyroidectomy alone [28]. Studies have shown that this procedure can be carried out safely by skilled surgeons at high-volume centers with low morbidity, despite the possibility of an increased risk of parathyroid and nerve injury [32]. In comparison to initial surgery, reoperative surgery for recurrent PTC in the central compartment typically results in more morbidity for the parathyroid glands and the recurrent laryngeal nerve [33, 34]. A select group of patients who would benefit from avoiding the need for reoperative surgery may benefit from PCLND. [35].
Lymphadenectomy is the best treatment when LN metastasis is clearly present on physical examination, or LN involvement is found on ultrasound [36]. But since LN involvement does not occur in all patients with PTC, not all patients benefit from this strategy, and there are conflicting results on this issue [37,38,39]. Surgeons who choose PCLND emphasize that metastasis is found in 50 to 80% of patients who are cN0 and that their resection reduces recurrence. On the other hand, adversaries of this method believe that routine dissection is unnecessary because the recurrence rate is only 1.4%, and the 5 year mortality rate is 0.9 to 17% [24]. Some surgeons recommend thyroidectomy alone in PTC without evidence of central and lateral LN involvement, and reoperation for LN dissection if the LNs become enlarged during follow-up, which usually occurs in 10–15% of patients. [14]. Opponents of this method argue that reoperation for CLND is accompanied by a higher recurrence rate and risk than primary CLND due to postoperative scarring and abnormal central neck anatomy after thyroidectomy [40, 41]. Some surgeons recommend routine removal of CLNs in the neck simultaneously as primary total thyroidectomy for PTC, intending to reduce the risk of recurrence and clean the central compartment so that reoperation would not be required in the dissected area [19, 40, 41]. The operation gained so many supporters that the 2006 Thyroid Association Guideline made significant changes, which recommended that all patients undergoing thyroidectomy for PTC, CLND be performed regardless of whether the LNs are enlarged [21]. The American Thyroid Association guideline, revised in 2009, states that PCLND (epithelial or bilateral) be performed in patients with cN0 PTC, especially for advanced (such as T3, T4, and grade C). However, this guideline recommends that due to the increase in morbidity, this surgery should be performed only among experienced surgeons [20]. Unfortunately, CLND in the neck has significant complications, even in the hands of experienced surgeons [42, 43]. The location of the CLNs in the neck in the tracheoesophageal groove puts the recurrent laryngeal nerves at risk of injury. In addition, large LNs may mimic healthy parathyroid tissue with the same blood supply. Some studies have shown that CLND of the neck is associated with an increase in postoperative hypoparathyroidism [44] and increases in surgery duration [14, 41, 43, 45, 46]. Our high-volume center is among the main center performing endocrine surgery centers, while also routinely performing exercising the PCLND technique in PTC patients. Based on our report, only 26 (44.8%) of patients developed transient hypoparathyroidism, which resolved shortly after during follow-ups. We also demonstrated that our cases of transient hypoparathyroidism were significantly associated with vascular invasion, bilateral or right-side location of tumor, and larger size of the tumor. In cases in which bilateral CLND cannot be performed either due to the patients or the surgeons features, ipsilateral CLND can be a good alternative to bilateral CLND in PTC cases with cN0-CLNs because its short-term oncological outcome is similar to bilateral CLND and the risk of complications is lower [15,16,17,18,19], however, bilateral metastasis can still occur in 20–50% of patients [16,17,18, 47].
The secondary purpose of this study was to answer the question of whether unilateral central lymphadenopathy can be appropriate and sufficient for patients with PTC cancer, in which based on our study, bilateral central lymphadenectomy is recommended. Our results generally showed no notable pattern of CLN involvement based on the tumors location. Furthermore, no association between CLN involvement and tumoral features including multifocal tumor, Intra/extracapsular invasion, vascular invasion, tumor size, and postop thyroglobulin. Also, postoperative thyroglobulin level was significantly associated with thyroid capsule invasion and tumors size category, in which a significant increase in thyroglobulin was observed from T1 to T3 type patients. Although some studies have reported tumor size can be an independent risk factor for CLN metastasis [16] .In a study by Chen et al., bilateral CLN metastasis was significantly associated with initial tumor size (above 1 cm), capsular invasion, peritracheal LN metastasis, and lateral and ipsilateral CLN metastasis. In contrast, age, sex, and location of the tumor were not associated with bilateral CLN metastasis [48]. Another study reported that tumor foci did not affect LN metastasis in smaller than 1 cm tumors [17]. The study by Zhang et al. showed that extrathyroid expansion and tumor size were independent risk factors for ipsilateral CLN metastasis; on the other hand, ipsilateral metastasis was an independent risk factor for CLN metastasis [49]. In a study by Yoon Kyoung et al. among 551 patients, 202 (37%) had subclinical CLN metastasis. Male gender, multifocal tumor, and extrathyroidal tumor were independent predictors of subclinical central metastasis. Significant risk factors for recurrence of the disease were reported to be the number of LN metastases (more than 10) and LN metastases with extracapsular expansion and measured thyroglobulin levels [50]. Significant risk factors for disease recurrence were reported, including the number of LN metastases (more than 10) and LN metastases with extracapsular expansion and measured thyroglobulin levels 6–12 months after initial treatment [51]. In a study by Jiang et al., latent metastasis to the CLNs was observed in 52.41% (533 out of 1017) PTCs. Multivariate analysis showed that age of 35 years and younger, tumor size above 1.5 cm, capsular or extracapsular invasion, tumors located in the upper and middle border bridge, and tumors located throughout the total thyroid lobe were risk factors for central LN metastasis. [52] Ito et al. study showed that CLN metastasis was observed in 63% of patients, and the frequency increased in relation to tumor size. The prevalence of lateral LN metastasis was 62%, which was also directly related to tumor size. In multivariate analysis of tumors larger than 1 cm, CLN metastasis was a predictor of survival. The frequency of parathyroid metastases on the opposite side of the tumor was significantly higher in tumors larger than 1 cm, but metastasis to this region did not independently predict worse survival. [53].
Among the limitations of our study is the short follow-up and small sample size, along with the single institutional nature of our research. More extensive multicentral studies are required to obtain further data and utilize multivariate regression analysis to distinguish risk factors for metastasis in thyroid cancer patients.
Conclusion
PCLND is a controversial matter, but in the hands of expert surgeons and in high-volume center, we believe that the benefits outweigh its risks. Based on our study, 75% of stage I and 100% of stage two case, and also 76.9% of T1, 86.7% of T2, and 80.0% of T3 cases had CLN involvement. CLN involvement had no significant association with the features when categorized by AJCC or TNM criteria, while also none of the preoperative and tumor features had a significant association with CLN involvement. However, the clinical importance and high CLN metastatic rate cannot be overlooked and we believe that this high involvement rate justifies the necessity of PCLND, even in low staging tumors. Furthermore, since tumor location was not associated with CLN involvement features, bilateral CLND should be carried out to avoid reoperation or metastasis in PTC patients.
Data availability
SPSS data of the participants can be requested from the authors. Please write to the corresponding author if you are interested in such data.
Abbreviations
- AJCC:
-
American joint committee on cancer
- ATA:
-
American thyroid association
- CLND:
-
Central lymph node dissection
- cN0:
-
Clinically node negative
- LN:
-
Lymph node
- PCLD:
-
Prophylactic central lymph node dissection
- PTC:
-
Papillary thyroid carcinoma
- RAI:
-
Radioactive iodine
References
Seib CD, Sosa JA (2019) Evolving understanding of the epidemiology of thyroid cancer. Endocrinol Metab Clin North Am 48(1):23–35
Guo Z, Ge M, Chu YH, Asioli S, Lloyd RV (2018) Recent advances in the classification of low-grade papillary-like thyroid neoplasms and aggressive papillary thyroid carcinomas: evolution of diagnostic criteria. Adv Anat Pathol 25(4):263–272
Shi X, Liu R, Basolo F, Giannini R, Shen X, Teng D et al (2016) Differential clinicopathological risk and prognosis of major papillary thyroid cancer variants. J Clin Endocrinol Metab 101(1):264–274
Rubinstein JC, Dinauer C, Herrick-Reynolds K, Morotti R, Callender GG, Christison-Lagay ER (2019) Lymph node ratio predicts recurrence in pediatric papillary thyroid cancer. J Pediatr Surg 54(1):129–132
Jiang LH, Yin KX, Wen QL, Chen C, Ge MH, Tan Z (2020) Predictive risk-scoring model for central lymph node metastasis and predictors of recurrence in papillary thyroid carcinoma. Sci Rep 10(1):710
Shuai Y, Yue K, Duan Y, Zhou M, Fang Y, Liu J et al (2021) Surgical extent of central lymph node dissection for papillary thyroid carcinoma located in the isthmus: a propensity scoring matched study. Front Endocrinol (Lausanne) 12:620147
Liu FH, Kuo SF, Hsueh C, Chao TC, Lin JD (2015) Postoperative recurrence of papillary thyroid carcinoma with lymph node metastasis. J Surg Oncol 112(2):149–154
Eltelety AM, Terris DJ (2019) Neck dissection in the surgical treatment of thyroid cancer. Endocrinol Metab Clin North Am 48(1):143–151
Chen L, Wu YH, Lee CH, Chen HA, Loh EW, Tam KW (2018) Prophylactic central neck dissection for papillary thyroid carcinoma with clinically uninvolved central neck lymph nodes: a systematic review and meta-analysis. World J Surg 42(9):2846–2857
Çolakoğlu B, Sağlam B, Sezer H, Kapran Y, Aydın Ö, Demirkol MO et al (2020) Effect of prophylactic central neck dissection on the surgical outcomes in papillary thyroid cancer: experience in a single center. Eur Arch Otorhinolaryngol 277(5):1491–1497
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 26(1):1–133
Park I, Her N, Choe JH, Kim JS, Kim JH (2018) Management of chyle leakage after thyroidectomy, cervical lymph node dissection, in patients with thyroid cancer. Head Neck 40(1):7–15
Sippel RS, Robbins SE, Poehls JL, Pitt SC, Chen H, Leverson G et al (2020) A Randomized controlled clinical trial: no clear benefit to prophylactic central neck dissection in patients with clinically node negative papillary thyroid cancer. Ann Surg 272(3):496–503
Shen WT, Ogawa L, Ruan D, Suh I, Kebebew E, Duh QY et al (2010) Central neck lymph node dissection for papillary thyroid cancer: comparison of complication and recurrence rates in 295 initial dissections and reoperations. Arch Surg (Chicago, III: 1960) 145(3):272–5
Chae BJ, Jung CK, Lim DJ, Song BJ, Kim JS, Jung SS et al (2011) Performing contralateral central lymph node dissection in papillary thyroid carcinoma: a decision approach. Thyroid 21(8):873–877
Koo BS, Choi EC, Yoon YH, Kim DH, Kim EH, Lim YC (2009) Predictive factors for ipsilateral or contralateral central lymph node metastasis in unilateral papillary thyroid carcinoma. Ann Surg 249(5):840–844
Moo TA, Umunna B, Kato M, Butriago D, Kundel A, Lee JA et al (2009) Ipsilateral versus bilateral central neck lymph node dissection in papillary thyroid carcinoma. Ann Surg 250(3):403–408
Raffaelli M, De Crea C, Sessa L, Giustacchini P, Revelli L, Bellantone C et al (2012) Prospective evaluation of total thyroidectomy versus ipsilateral versus bilateral central neck dissection in patients with clinically node-negative papillary thyroid carcinoma. Surgery 152(6):957–964
Son YI, Jeong HS, Baek CH, Chung MK, Ryu J, Chung JH et al (2008) Extent of prophylactic lymph node dissection in the central neck area of the patients with papillary thyroid carcinoma: comparison of limited versus comprehensive lymph node dissection in a 2-year safety study. Ann Surg Oncol 15(7):2020–2026
Cooper DS, Doherty GM, Haugen BR, Kloos RT, American Thyroid Association Guidelines Taskforce on Thyroid N, Differentiated Thyroid C et al (2009) Revised American thyroid association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 19(11):1167–214
Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ et al (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer: the American thyroid association guidelines taskforce. Thyroid 16(2):109–142
Grodski S, Cornford L, Sywak M, Sidhu S, Delbridge L (2007) Routine level VI lymph node dissection for papillary thyroid cancer: surgical technique. ANZ J Surg 77(4):203–208
Lydiatt WM, Patel SG, O’Sullivan B, Brandwein MS, Ridge JA, Migliacci JC et al (2017) Head and neck cancers-major changes in the American joint committee on cancer eighth edition cancer staging manual. CA Cancer J Clin 67(2):122–37
Takami H, Sasaki K, Ikeda Y, Tajima G, Kameyama K (2003) Detection of sentinel lymph nodes in patients with papillary thyroid cancer. Asian J Surg/Asian Surg Assoc 26(3):145–148
Roh JL, Park CI (2008) Sentinel lymph node biopsy as guidance for central neck dissection in patients with papillary thyroid carcinoma. Cancer 113(7):1527–1531
Association WM (2013) World medical association declaration of helsinki: ethical principles for medical research involving human subjects. JAMA 310(20):2191–2194
Lundgren CI, Hall P, Dickman PW, Zedenius J (2006) Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer 106(3):524–531
Zhao WJ, Luo H, Zhou YM, Dai WY, Zhu JQ (2017) Evaluating the effectiveness of prophylactic central neck dissection with total thyroidectomy for cN0 papillary thyroid carcinoma: an updated meta-analysis. Eur J Surg Oncol 43(11):1989–2000
Ma B, Wang Y, Yang S, Ji Q (2016) Predictive factors for central lymph node metastasis in patients with cN0 papillary thyroid carcinoma: a systematic review and meta-analysis. Int J Surg 28:153–161
Oh HS, Park S, Kim M, Kwon H, Song E, Sung TY et al (2017) Young age and male sex are predictors of large-volume central neck lymph node metastasis in clinical N0 papillary thyroid microcarcinomas. Thyroid 27(10):1285–1290
Sancho JJ, Lennard TW, Paunovic I, Triponez F, Sitges-Serra A (2014) Prophylactic central neck disection in papillary thyroid cancer: a consensus report of the European society of endocrine surgeons (ESES). Langenbeck’s Archives of Surg/Deutsche Gesellschaft fur Chirurgie 399(2):155–163
Chisholm EJ, Kulinskaya E, Tolley NS (2009) Systematic review and meta-analysis of the adverse effects of thyroidectomy combined with central neck dissection as compared with thyroidectomy alone. Laryngoscope 119(6):1135–1139
Uruno T, Miyauchi A, Shimizu K, Nakano K, Takamura Y, Ito Y et al (2004) Prognosis after reoperation for local recurrence of papillary thyroid carcinoma. Surg Today 34(11):891–895
Moley JF, Lairmore TC, Doherty GM, Brunt LM, DeBenedetti MK (1999) Preservation of the recurrent laryngeal nerves in thyroid and parathyroid reoperations. Surgery 126(4):673–7 (discussion 7–9)
Goode A (1991) Surgery of the thyroid and parathyroid glands third Edition Blake Cady and Ricardo L. Rossi. WB Saunders company: Philadelphia, 1991. ISBN 0-7216-3462-1. Price£ 46.00 ($75.00). J Laryngol Otol 105(4):326
Caron NR, Clark OH (2005) Papillary thyroid cancer: surgical management of lymph node metastases. Curr Treat Options Oncol 6(4):311–322
Arch-Ferrer J, Velazquez D, Fajardo R, Gamboa-Dominguez A, Herrera MF (2001) Accuracy of sentinel lymph node in papillary thyroid carcinoma. Surgery 130(6):907–913
Hughes DT, White ML, Miller BS, Gauger PG, Burney RE, Doherty GM (2010) Influence of prophylactic central lymph node dissection on postoperative thyroglobulin levels and radioiodine treatment in papillary thyroid cancer. Surgery 148(6):1100–6 (discussion 006–7)
Pereira JA, Jimeno J, Miquel J, Iglesias M, Munne A, Sancho JJ et al (2005) Nodal yield, morbidity, and recurrence after central neck dissection for papillary thyroid carcinoma. Surgery 138(6):1095–100 (discussion 100–1)
Low TH, Delbridge L, Sidhu S, Learoyd D, Robinson B, Roach P et al (2008) Lymph node status influences follow-up thyroglobulin levels in papillary thyroid cancer. Ann Surg Oncol 15(10):2827–2832
White ML, Gauger PG, Doherty GM (2007) Central lymph node dissection in differentiated thyroid cancer. World J Surg 31(5):895–904
Cheah WK, Arici C, Ituarte PH, Siperstein AE, Duh QY, Clark OH (2002) Complications of neck dissection for thyroid cancer. World J Surg 26(8):1013–1016
Palestini N, Borasi A, Cestino L, Freddi M, Odasso C, Robecchi A (2008) Is central neck dissection a safe procedure in the treatment of papillary thyroid cancer? Our experience. Langenbeck’s Arch Surg/Deutsche Gesellschaft fur Chirurgie 393(5):693–698
Cavicchi O, Piccin O, Caliceti U, De Cataldis A, Pasquali R, Ceroni AR (2007) Transient hypoparathyroidism following thyroidectomy: a prospective study and multivariate analysis of 604 consecutive patients. Otolaryngol--Head Neck Surg 137(4):654–8
Carling T, Long WD 3rd, Udelsman R (2010) Controversy surrounding the role for routine central lymph node dissection for differentiated thyroid cancer. Curr Opin Oncol 22(1):30–34
Rotstein L (2009) The role of lymphadenectomy in the management of papillary carcinoma of the thyroid. J Surg Oncol 99(4):186–188
Raffaelli M, De Crea C, Sessa L, Giustacchini P, Bellantone R, Lombardi CP (2013) Can intraoperative frozen section influence the extension of central neck dissection in cN0 papillary thyroid carcinoma? Langenbeck’s Arch Surg/Deutsche Gesellschaft fur Chirurgie 398(3):383–388
Rui Chen, Jingqiang Zhu, Tao Wei, Rixiang Gong, Zhihui Li, Xiuhe Zou, Feng Liu, Yu Ma. Predictors of bilateral central neck lymph node dissection in unilateral papillary thyroid carcinoma. Journal of Clinical Oncology 2014(32):15. suppl e17012–e17012
Zhang Y, Zhang B, Wan H, Yan D, Xu Z, Tang P (2014) Factors related to central lymph node metastasis in different subregions for unilateral papillary thyroid carcinoma with clinical N0 stage. Zhonghua er bi yan hou tou jing wai ke za zhi = Chin J Otorhinolaryngol Head Neck Surg 49(10):807–11
So YK, Son YI, Hong SD, Seo MY, Baek CH, Jeong HS et al (2010) Subclinical lymph node metastasis in papillary thyroid microcarcinoma: a study of 551 resections. Surgery 148(3):526–531
Leboulleux S, Rubino C, Baudin E, Caillou B, Hartl DM, Bidart JM et al (2005) Prognostic factors for persistent or recurrent disease of papillary thyroid carcinoma with neck lymph node metastases and/or tumor extension beyond the thyroid capsule at initial diagnosis. J Clin Endocrinol Metab 90(10):5723–5729
Jiang LH, Chen C, Tan Z, Lu XX, Hu SS, Wang QL et al (2014) Clinical characteristics related to central lymph node metastasis in cN0 papillary thyroid carcinoma: a retrospective study of 916 patients. Int J Endocrinol 2014:385787
Ito Y, Jikuzono T, Higashiyama T, Asahi S, Tomoda C, Takamura Y et al (2006) Clinical significance of lymph node metastasis of thyroid papillary carcinoma located in one lobe. World J Surg 30(10):1821–1828
Acknowledgements
None to declare.
Funding
The study was financially supported by the office of the vice-chancellor for research at the Tehran University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
SN: designed the study while SMM, KR, SS : collected the data. RS: performed the literature review, analyzed the data and drafted the manuscript. SMM and SN: revised the manuscript. All authors proofread the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval and consent to participate
Iran University of Medical Sciences Human Ethics Committee approved the study (IR.TUMS.MED.REC.1394.1972). A written informed consent form was obtained from all the participants enrolled in this trial. All patients’ information was de-identified and documented confidentially, and patients were able to exit any time during the trial if they desired. All ethical principles of the Declaration of Helsinki were considered in this trial.
Consent to publication
Not applicable.
Research involving human participants and/or animals
A written informed consent form was obtained from all the participants enrolled in this trial. All patients' information was de-identified and documented confidentially, and patients were able to exit any time during the trial if they desired.
Informed consent
All ethical principles of the Declaration of Helsinki were considered in this trial. Iran University of Medical Sciences Human Ethics Committee approved the study (IR.TUMS.MED.REC.1394.1972).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shahriarirad, R., Meshkati Yazd, S.M., Zahedi, R. et al. Evaluation of the role of prophylactic bilateral central neck lymph node dissection in patients with papillary thyroid carcinoma: a case controlled study. Updates Surg 75, 679–689 (2023). https://doi.org/10.1007/s13304-022-01440-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01440-0