Abstract
Children with end-stage liver disease have been found to have cognitive deficits. The aim of this study was to examine whether cholestatic jaundice causes spatial deficits in rats and if these cognitive deficits are reversed by biliary drainage. Rats were randomly divided into three groups. In the first group, the bile duct was ligated for 3 weeks (BDL group); in the second group, the proximal bile duct was ligated with a Broviac CV catheter for 2 weeks followed by a tube bilioduodenostomy (TBD group); in the third group, a sham operation was performed (SHAM group). All the surviving rats were assessed for spatial learning and memory (a major cognitive function in rats) by the Morris water maze task about 3 weeks after the first operation. Blood was aspirated by cardiocentesis and assayed for total bilirubin, albumin, ammonia, and hemoglobin levels on the day following the water maze task. During the four consecutive acquisition trial days of the Morris water maze, jaundiced rats (BDL group) had a significant longer latency to escape than the SHAM group (p < 0.05). Rats that underwent biliary decompression for 1 week (TBD group) showed improved status of the spatial deficit, as they required less time to reach the escape platform, approaching the performance of the SHAM group. The BDL group had a significantly higher serum ammonia level, higher bilirubin level, and lower hemoglobin level than the other two groups. After biliary decompression for 1 week, the serum albumin concentration in the TBD group still did not return to the level of the SHAM group. The results of this study suggest that long-term cholestasis results in spatial memory deficits in rats that correlate with anemia and hyperbilirubinemia encephalopathy. Early biliary decompression of obstructive jaundice improves spatial memory deficits, possibly related to the recovery of the serum ammonia and hemoglobin levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Children with end-stage liver disease have been found to have cognitive deficits. For example, children with biliary atresia have deficits in their performance intelligence quotient (IQ) and spatial and sequential scores before liver transplantation [1]. Unfortunately, after liver transplantation many patients still have deficits in their performance IQ, learning and memory, and visuospatial function [2]. Many factors relate to posttransplantation cognitive deficits, such as surgery itself, the recovery process, and steroid and immunosuppressant treatment [3, 4].
In adults with liver disease, visuospatial function relates to clinical measures of liver function: serum albumin and serum ammonia levels [5, 6, 7]. Information regarding the long-term effects of cholestasis on cognitive performance is scarce, and the role of reducing the bilirubin level in the recovery of cognitive function remains largely unknown. In the present study, we examined the cognitive function in rats with obstructive jaundice using the Morris water maze, a standard test for assessing spatial learning and memory function in rodents [7].
The study was designed to address three specific areas: (1) the spatial performance of rats with obstructive jaundice; (2) the relation between spatial memory deficit and measures of liver disease severity; and (3) whether biliary drainage improves the spatial memory deficit caused by bile duct obstruction.
Materials and Methods
Animals
This experiment was performed under the Guidelines for Animal Experiments of Chang Gung Memorial Hospital and Chang Gung University. Male Sprague-Dawley rats weighing 250 to 300 g were used. Attempts were made to minimize the number of animals used. The animals were kept in individual cages and acclimated for ≥ 7 days before use. All animals were housed in a room maintained at 24°C with 12-hour light/dark cycles; they had free access to water and standard laboratory chow. Before each operation, animals were fasted overnight with free access to water.
Experimental Design
The experimental design is presented in Figure 1. All surgical procedures were performed under pentobarbital (Nembutal) (50 mg/kg) anesthesia with clean surgical techniques as previously described [8]. Briefly, preparation for obstructive jaundice was done by opening a midline incision in the abdomen and placing a Broviac 2.7F single-lumen CV catheter (Bard Access System, Salt Lake City, UT, USA) in the proximal common bile duct. After ligating the proximal and distal bile ducts, the common bile duct was divided. The distal end of the Broviac tube was sealed. For the 10 rats in the BDL group, the bile duct was ligated (BDL group) for 3 weeks. Three of these animals died during the experiment owing to a ruptured choledochocele. For the 10 rats in the TBD group, the bile duct was ligated for 2 weeks, then tube bilioduodenostomy (TBD group) was performed according to the method of Ryan et al. [9] with minor modification. After biliary obstruction for 2 weeks, the abdomen was reopened, and the sealed end of the tube was opened, inserted into the duodenum about 1.5 cm from the pylorus, and then tied in position with two 7-0 PDS purse-string sutures. Five TBD animals died during surgery or hours later, and the surviving rats were studied after another week. Finally, six rats underwent sham ligation of the bile duct (SHAM group) and served as the controls.
From the 22nd to the 27th day after the first operation, all rats were tested in the Morris water maze. On the following day, after completion of the water maze task, blood was aspirated by cardiocentesis and assayed for total bilirubin, albumin, ammonia, and hemoglobin levels.
Morris Water Maze
Eighteen rats (SHAM, n = 6; BLD, n = 7; TBD, n = 5) were evaluated for spatial memory in the Morris water maze, as previously described [10]. The Morris water maze, a test of spatial learning and memory commonly used in rodents, is considered to be hippocampus-dependent [11]. The probe trial assesses spatial bias in the rat’s search pattern during retrieval [12]. A circular steel tank (180 cm diameter × 50 cm high) was filled with water (26 ± 16 cm) to a depth of 25 cm; the water was made opaque by adding 100 ml of evaporated milk, which prevented visualization of the platform. Room lights illuminated the pool, and visual clues around the room (window, cabinets, furniture) were kept at a constant location from day to day. Four points on the perimeter of the pool were designed—north (N), east (E), south (S), and west (W)—thereby dividing the pool into four quadrants (NW, NE, SE, SW).
A 10 × 10 cm Plexiglas platform, onto which the rat could escape, was positioned in the center of one of the quadrants 1 cm below the water surface. A video camera was set above the center of the pool and was connected to a video-traction system (Ethovision, Noldus, The Netherlands). On the first day, each rat was placed in the pool for 60 seconds without the platform present; this free swim enabled the rat to become habituated to the training environment (training trial). On days 2 to 5 the rats were subjected to 24 trials (six trials a day) to locate and escape onto the submerged platform (acquisition trial). The quadrant in which the platform was located remained constant for each rat, but the point of immersion into the pool varied between N, E, S, and W in a quasirandom order for the 24 trials so the rat was not able to predict the platform location from the point at which it was placed in the pool.
On mounting the platform, the rats were given a 30-second rest period, after which the next trial was started. If the rat did not find the platform in 120 seconds, it was manually placed on the platform for a 30-second rest. At the start of each trial, the rat was held facing the perimeter and dropped into the pool to ensure immersion. Latencies to escape onto the platform were recorded. On day 6, the platform was removed. The rat was allowed 60 seconds of free swimming. The search pattern was tested to assess memory for platform location (probe trial). The testing procedure for locating the hidden platform is considered a measure of spatial reference memory, and the probe trial is considered a measurement of memory retrieval and strength of spatial learning [12].
Blood Analysis
The hemoglobin level was measured in EDTA-mixed whole blood using an automated technique by Sysmex Ne-α (Sysmex, Osaka, Japan). Plasma was separated from heparinized blood to determine the albumin and total bilirubin levels using a Hitachi 7450 (Hitachi, Tokyo, Japan) and the ammonia level by a Beckman CX-9 (Beckman, Fullerton, CA, USA).
Statistical Analysis
Comparisons of the escape latencies during the 24 trials of place learning of the Morris water maze and the data of blood analysis were analyzed by one-way analysis of variance (ANOVA) with the least significant difference (LSD) post hoc test and repeated measures. The swimming speed and the probe trial were analyzed with the nonparametric Kruskal-Wallis H test. Values were expressed as the mean ± SEM, and significance was defined as p < 0.05 for all tests.
Results
Morris Water Maze
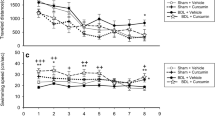
Figure 2 shows the escape latency in the water maze as a function of days. Although all groups displayed improvements over the 4 days of training, the performance of this task among these groups was significantly different, with the maximum difference on the last testing day (F2,15 = 4.86, p < 0.05). Post hoc testing showed that there was no difference between the SHAM group and the TBD group over the four testing days. This finding demonstrated that obstructive jaundice (BDL group) impaired spatial learning of rats, and the early tube bilioduodenostomy correction in rats with jaundice ameliorated the spatial memory deficits. There was no significant difference in swimming speed among the three groups (p > 0.1). Additionally, in the probe trial, there was an increasing percentage of time in the target quadrant for all groups, but the differences did not reach statistical significance (p > 0.1).
Latencies to escape in the Morris water maze (mean ± SEM) for the sham controls, jaundiced rats with BDL, and jaundiced rats corrected with TBD. There were significant differences among groups over the 4 days of the test, with maximum latency on the last day (F2,15 = 4.86; p < 0.05). Furthermore, the post hoc test revealed that, compared with the BDL group, the TBD group had differences on the first 2 days (p < 0.05), whereas the SHAM group showed significant differences over all 4 days (p < 0.05). §Statistical difference (p < 0.05) among three groups. *Statistical difference (p < 0.05) compared with the BDL group.
Blood sample Analysis The data from the blood analyses are shown in Table 1. The BDL group had significantly higher serum concentrations of ammonia and total bilirubin and a lower serum hemoglobin level than the SHAM or the TBL group (p < 0.05). The BDL and TBD groups both had lower serum albumin levels than the SHAM group (p < 0.05). In addition, there was no difference in serum bilirubin, ammonia, or hemoglobin concentration between the TBD and SHAM groups. These data suggest that biliary drainage improved the serum liver function test results (bilirubin and ammonia), but the serum albumin concentration in the TBD group was still lower than that of the SHAM group.
Discussion
The results of this study revealed that jaundiced rats had worse spatial memory and lower serum ammonia and hemoglobin levels than nonjaundiced rats. Our data also showed that early surgical correction in rats with obstructive jaundice might improve spatial memory deficits. Restoration of serum ammonia and hemoglobin levels is associated with the recovery of spatial deficits.
In the Morris water maze task, animals must learn and use spatial strategies to locate a hidden platform. In the present study, jaundiced rats had a poor performance regarding acquisition memory (days 2–5) compared with nonjaundiced rats. However, the spatial deficit was reversed by surgical correction of the biliary obstruction. The probe trial (day 6) is considered a measurement of memory retrieval and strength of spatial learning [12]. In this experiment, however, there was no significant difference in spatial retrieval between jaundiced and nonjaundiced rats.
Biliary atresia is the most common variant of infantile obstructive cholangiopathy, a major indication for liver transplantation in children. The present study clearly demonstrated that relief of jaundice resulted in better spatial memory performance in rodents. Although extrapolation of rodent experiments to human conditions is difficult, this study suggests that early surgical intervention for irreversible or progressive liver diseases before the development of obvious liver failure are beneficial for cognitive function.
Circulating neurotoxins play a role in cognitive deficits in liver failure patients [13]. In this study, the BDL group showed impaired spatial learning and memory that was related to the bilirubin level, nutritional state, and hemoglobin value. Liver function assessments were normalized after 7 days of biliary decompression. The concentrations of serum total bilirubin, ammonia, and hemoglobin recovered in the TBD group, accompanied by improved spatial performance. Because hypoalbuminemia persisted into the second week despite biliary decompression, our data do not indicate that the serum albumin level is related to spatial memory performance.
The hippocampus is critically involved in the acquisition and consolidation of memory for spatial learning in animals [14]. Ammonia exerts a deleterious effect on cerebral function [15]. Furthermore, excess ammonia is reported to inhibit excitatory neurotransmission and firing in hippocampal CA1 neurons [16]. Our data support the concept that a high ammonia concentration is detrimental to the brain. In addition, we provide new evidence that a high ammonia concentration plays a role in cognitive deficits in cholestatic rats. Anemia may impair cognitive function in both adults [17] and infants [18]. Similarly, perinatal iron deficiency may lead to decreased cytochrome c oxidase activity (an indicator of neuronal activity [19]) in selected brain regions involved in cognition [20]. The main targets of iron deficiency are hippocampal formation and prefrontal projection, both of which structures are implicated in the explicit memory circuit [21]. An increased hemoglobin concentration might deliver more oxygen and hence improve cognitive function [17, 22].
Conclusions
Cognitive deficits may be induced by obstructive jaundice before liver failure. Early biliary decompression might improve the cognitive deficits and associated anemia as well as the liver function tests. The findings of this study imply that biliary decompression has some value in reversing spatial memory impairment following obstructive jaundice.
Résumé.
On sait que certains enfants porteurs d’insuffisance hépatique terminale ont des déficits cognitifs. Le but de cette étude a été de déterminer si l’ictère choléstatique provoque des déficits spatiaux chez le rat et si ces déficits cognitifs peuvent être guéris par un drainage biliaire. Trois groupes de rats, traités différemment selon un tirage au sort, ont été étudiés: dans le premier groupe, la voie biliaire a été liée pendant trois semaines (groupe BDL); dans le deuxième groupe, la voie biliaire a été liée avec un cathéter Broviac CV inséré dans la voie biliaire proximale pendant deux semaines et ensuite une anastomose bilio duodénale a été réalisée sur tube (groupe TBD); dans le troisième groupe, une intervention factice a été pratiquée (groupe SHAM). Tous les rats ayant survécu ont été évalués pour l’apprentissage spatial et la mémoire, une fonction cognitive majeure chez le rat, par le test « tâches en labyrinthe d’eau » de Morris, trois semaines après la première opération. On a prélevé du sang par cardiocentèse pour doser la bilirubine totale, l’albumine, l’ammoniémie et l’hémoglobine le jour suivant le test de Morris. Pendant les quatre jours consécutifs du test de Morris, le temps que les rats ictériques (groupe BDL) mettaient pour s’échapper était plus long que pour le groupe SHAM (p < 0.05). Les rats ayant reçu une décompression biliaire pendant une semaine (groupe TBD) ont montré une amélioration du déficit spatial car ils ont nécessité moins de temps pour atteindre la plateforme pour s’échapper, une performance pas très différente des rats du groupe SHAM. Le groupe BDL avaient un taux d’ammoniémie et de bilirubinémie significativement plus élevé et un taux d’hémoglobine significativement plus bas en comparaison aux autres groupes. Après une décompression biliaire d’une semaine, les taux d’albumine sérique dans le groupe TBD n’est pas revenu aux niveaux de ceux du groupe SHAM. Les résultats de cette étude suggèrent que la cholestase à long terme provoque des déficits de mémoire spatiale chez le rat qui corrèlent avec le taux d’anémie et l’incidence d’encéphalopathie secondaire à l’hyperbilirubinémie. La décompression biliaire précoce de l’ictère par obstruction améliore les déficits de mémoire spatiale, possiblement en rapport avec la normalisation des taux de l’ammoniémie et de l’hémoglobinémie.
Resumen.
Se ha encontrado que los niños con enfermedad hepática terminal presentan déficits de cognición. El propósito del presente estudio fue investigar si la ictericia colestásica causa déficits espaciales y si tales déficits cognitivos pueden ser revertidos mediante drenaje biliar. Se hizo aleatorización de ratas en tres grupos: en el primero se ligó el conducto biliar por un periodo de 3 semanas (grupo LCB); en el segundo se practicó la ligadura en la región proximal con un catéter VC Broviac por 2 semanas y luego se realizó una bilioduodemostomía de tubo (grupo BDT); en el tercer grupo se realizó una operación “fantasma” (sham-operation) (grupo SHAM). Se procedió a evaluar la capacidad de aprendizaje espacial y la memoria en las ratas supervivientes, que es una función cognitiva mayor en la rata, mediante la prueba de agua y laberinto de Morris a las tres semanas después de la primera operación. Se tomaron muestras de sangre por cardiocentesis para determinación de bilirrubina total, albúmina, amoniaco y hemoglobina en el día siguiente a la prueba de agua y laberinto. En el curso de los cuatro días consecutivos de adquisición de la prueba de Morris, las ratas ictéricas (grupo LCB) exhibieron latencias de escape significativamente más prolongadas, en comparación con el grupo SHAM (p < 0.05). Las ratas que recibieron descompresión biliar por una semana (grupo BDT) mostraron mejoría del déficit espacial en cuanto a que requirieron menos tiempo para alcanzar la plataforma de escape y mostraron un rendimiento semejante al de grupo SHAM. El grupo LCB exhibió niveles séricos significativamente más elevados de amoniaco y de bilirrubina y niveles más bajos de hemoglobina en comparación con los otros dos grupos. Luego de la descompresión biliar por una semana, la concentración de albúmina en el grupo BDT todavía no alcanzó a retornar al nivel del grupo SHAM. Los resultados de este estudio sugieren que la colestasis a largo plazo resulta en déficits de memoria espacial en la rata, lo cual se correlaciona con anemia y encefalopatía de hiperbilirrubinemia. La descompresión precoz de una ictericia obstructiva mejora los déficits de memoria especial, por un mecanismo tal vez relacionado con la normalización de los niveles de amoniaco y de hemoglobina.
References
SM Stewart RA Cambell D McCallon et al. (1992) ArticleTitleCognitive patterns in school-age children with end-stage liver disease J. Dev. Behav. Pediatr. 13 331–338 Occurrence Handle1:STN:280:ByyD3Mnpt1w%3D Occurrence Handle1401116
SM Stewart C Hiltebeitel J Nici et al. (1991) ArticleTitleNeuropsychological outcome of pediatric liver transplantation Pediatrics 87 367–376 Occurrence Handle1:STN:280:By6C2MnktFI%3D Occurrence Handle2000277
B Gridelli A Lucianetti G Rodriguez et al. (1994) ArticleTitleNeurologic complications following pediatric orthotopic liver transplantation Transplant Proc. 26 193–194 Occurrence Handle1:STN:280:ByuC2M7ptFU%3D Occurrence Handle8108938
BP Garg LE Walsh MD Pescovitz et al. (1993) ArticleTitleNeurologic complications of pediatric liver transplantation Pediatr. Neurol. 9 444–448 Occurrence Handle10.1016/0887-8994(93)90023-6 Occurrence Handle1:STN:280:ByqA38bhvVI%3D Occurrence Handle7605552
SJ Gilberstadt H Gilberstadt L Zieve et al. (1980) ArticleTitlePsychomotor performance defects in cirrhotic patients without overt encephalopathy Arch. Intern. Med. 140 519–521 Occurrence Handle10.1001/archinte.140.4.519 Occurrence Handle1:STN:280:Bi%2BC2M3lt1w%3D Occurrence Handle7362383
H Schomerus W Hamster H Blunck et al. (1981) ArticleTitleLatent portasystemic encephalopathy: nature of cerebral functional defects and their effect on fitness to drive Dig. Dis. Sci. 28 622–630
RGM Morris P Garrud JNP Rawlins et al. (1982) ArticleTitlePlace navigation is impaired in rats with hippocampal lesions Nature 297 681–683 Occurrence Handle1:STN:280:Bi2B38%2Fgtl0%3D Occurrence Handle7088155
CS Hsieh CC Huang JJ Wu et al. (2001) ArticleTitleAscending cholangitis provokes IL-8 and MCP-1 expression and promotes inflammatory cell infiltration in the cholestatic rat liver J. Pediatr. Surg. 36 1623–1628 Occurrence Handle10.1053/jpsu.2001.27933 Occurrence Handle11685687
CJ Ryan T Than LH Blumgart (1977) ArticleTitleCholedochoduodenostomy in the rat with obstructive jaundice J. Surg. Res. 23 321–331 Occurrence Handle909295
LT Huang SL Yang CW Liou et al. (2002) ArticleTitlePentylenetetrazol-induced recurrent seizures in rat pups: time course on spatial learning and long-term effects Epilepsia 43 567–573 Occurrence Handle10.1046/j.1528-1157.2002.29101.x Occurrence Handle12060014
R Morris (1984) ArticleTitleDevelopments of a water-maze procedures for studying spatial learning in the rat J. Neurosci. Methods 11 47–60 Occurrence Handle10.1016/0165-0270(84)90007-4 Occurrence Handle1:STN:280:BiuB1Mzps1w%3D Occurrence Handle6471907
H Jeltsch F Bertrand C Lazarus et al. (2001) ArticleTitleCognitive performances and locomotor activity following dentate granule cell damage in rats: role of lesion extent and type of memory tested Neurobiol. Learn. Mem. 76 81–105 Occurrence Handle10.1006/nlme.2000.3986 Occurrence Handle1:STN:280:DC%2BD3MvotFClsQ%3D%3D Occurrence Handle11525255
CC Lui CL Chen YF Cheng et al. (1998) ArticleTitleRecovery of neurological deficits in a case of Wilson’s disease after liver transplantation Transplant Proct. 30 3324–3325 Occurrence Handle10.1016/S0041-1345(98)01048-3 Occurrence Handle1:STN:280:DyaK1M%2FlsFynug%3D%3D
J O’Keefe L Nadel (1978) The Hippocampus as a Cognitive Map Oxford University Press New York
JC Szerb RF Butterworth (1992) ArticleTitleEffects of ammonium ions on synaptic transmission in the mammalian central nervous system Prog. Neurobiol. 39 135–153 Occurrence Handle10.1016/0301-0082(92)90008-3 Occurrence Handle1:CAS:528:DyaK38XltVyls7Y%3D Occurrence Handle1354386
P Fan J Lavoie NL Le (1990) ArticleTitleNeurochemical and electrophysiological studies on the inhibitory effects on ammonium ions on synaptic transmission in slices of rat hippocampus: evidence for a postsynaptic action Neuroscience 37 327–334 Occurrence Handle10.1016/0306-4522(90)90403-Q Occurrence Handle1:CAS:528:DyaK3MXktVag Occurrence Handle1966824
RB Weiskopf JH Kramer M Viele et al. (2002) ArticleTitleAcute severe isovolemic anemia impairs cognitive function and memory in humans Anesthesiology 92 407–413
T Walter I Andrance ParticleDe P Chadud et al. (1989) ArticleTitleIron deficiency anemia: adverse effects on infant psychomotor development Pediatrics 84 7–17 Occurrence Handle1:STN:280:BiaB1MnjvF0%3D Occurrence Handle2472596
MTT Wong-Riley (1989) ArticleTitleCytochrome oxidase: an endogenous metabolic marker for neuronal activity Top. Neurosci. 12 94–101 Occurrence Handle10.1016/0166-2236(89)90165-3 Occurrence Handle1:CAS:528:DyaL1MXitV2lurc%3D
M DeUngria R Rao JD Wobken et al. (2000) ArticleTitlePerinatal iron deficiency decrease cytochrome c oxidase (CytOx) activity in selected regions of neonatal rat brain Pediatr. Res. 48 169–176 Occurrence Handle1:CAS:528:DC%2BD3cXlvVyitr4%3D Occurrence Handle10926291
T Steckler WHIM Drinkenburg A Sahgal et al. (1998) ArticleTitleRecognition memory in rats. II. Neuroanatomical substrates Prog. Neurobiol. 54 313–332 Occurrence Handle10.1016/S0301-0082(97)00061-0 Occurrence Handle1:STN:280:DyaK1c7kt1yjsg%3D%3D Occurrence Handle9481801
JC Stivelman (2000) ArticleTitleBenefits of anaemia treatment on cognitive function Nephrol. Dial. Transplant. 15 29–35 Occurrence Handle10.1093/ndt/15.suppl_6.29
Acknowledgments.
The authors thank Mr. Nyuk-Kong Chang for his technical assistance. This study was supported in part by grants from the National Science Council of the Republic of China (NSC-89-2314-B-182A-081 and NSC-89-2314-B-182A-178 to Dr. Chih-Sung Hsieh; CMRP G8059 from Chang Gung Memorial Hospital to Dr. Li-Tung Huang; and CMHFR9135 from Chi Mei Foundation Hospital to Dr. Ming-Chi Lai.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Huang, LT., Hsieh, CS., Chou, MH. et al. Obstructive Jaundice in Rats: Cause of Spatial Memory Deficits with Recovery after Biliary Decompression . World J. Surg. 28, 283–287 (2004). https://doi.org/10.1007/s00268-003-7209-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-003-7209-z