Abstract
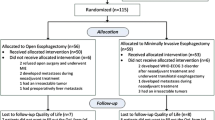
Patients with advanced, incurable gastric cancer may present with mild symptoms or require immediate therapeutic intervention. The influence of the intensity of preoperative symptoms on postoperative survival and quality of life (QoL) was evaluated in a palliative setting. In a historical cohort analysis of 492 patients with gastric cancer treated between 1992 and 2001, a total of 169 (34.4%) patients had incurable disease (i.e., pTxNxM1). Patients were classified as having major symptoms if they presented with upper gastrointestinal bleeding (i.e., hematemesis or bloody stools), gastric inlet or outlet obstruction (i.e., symptomatic and endoscopically proven stenosis), or perforation caused by the tumor. All other patients were defined as having minor symptoms. QoL was assessed prospectively using the EORTC questionnaire. The questionnaire was given to the patients before operation, before discharge, and 3 months after operation; and it was analyzed by the Mann-Whitney U-test. Survival, demographic data, and histopathologic characteristics were assessed and analyzed by the log-rank test and the χ2 test, respectively. Of the 169 patients, 75 (44.3%) presented with major symptoms and 94 (55.7%) with minor symptoms. The distribution of patients undergoing resection or exploration was comparable for the two groups [major: 61 (81.5%)/14 (18.5%); minor: 77 (81.9%)/17 (18.1%)]. Despite comparable demographic and histopathologic characteristics with equal hospital mortality and morbidity (14.6% vs. 8.5%/49.3% vs. 40.4%), the median survival rates in two groups were 4 and 6 months, respectively (p < 0.05). This was not influenced by the type of operation. QoL was not different in patients with major or minor symptoms before operation or 3 months thereafter. However, preoperative symptoms such as nausea/vomiting and melena were rated significantly higher in patients with major symptoms. In patients with incurable gastric cancer the preoperative intensity of symptoms has a significant impact on survival and QoL, which is not influenced by the operation. The necessity of surgery in patients with minor symptoms requires careful consideration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Patients with advanced, incurable gastric cancer (metastatic disease, pTxNxM1) may present with symptoms such as bleeding, perforation, or obstruction, leading to immediate endoscopic or surgical intervention. Another group of patients may present with only moderate symptoms. For gastric cancer patients in a palliative situation, studies have demonstrated the benefit of gastrectomy with regard to postoperative survival [1, 2, 3]. The rationale for resecting the tumor is to avoid complications such as bleeding, perforation, and obstruction [4]. This approach has been practiced in our department as the procedure of choice. In contrast, other studies have demonstrated no benefit of tumor resection under these circumstances [5, 6, 7].
In none of these studies, however, has the preoperative intensity of symptoms been considered. Furthermore, postoperative quality of life has become an important factor when evaluating operative results in general and oncologic operations in particular. Hence, this information needs to be included, as demonstrated by our group and others [8, 9].
The aim of this study was to determine the impact of the intensity of preoperative symptoms on postoperative survival and quality of life. In addition, we evaluated the effect of the type of operation and the extent of resection (i.e., lymphadenectomy and splenectomy) on postoperative survival.
Materials and Methods
The hospital records of 492 patients with gastric cancer treated in our hospital during the period 1992–2001 were reviewed.
Study Design
Demographic data, preoperative symptoms, type of operation, localization of the tumor and of metastases, hospital morbidity and mortality, and length of hospital stay were recorded. The disease was staged according to the TNM system. In addition, we extracted information from the follow-up period, including data about the quality of life (QoL).
The operative procedure was defined as palliative when distant metastases were found pre- or intraoperatively (TxNxM1; i.e., stage IV) (n = 169, 34.4%). Histopathologic specimens of the distant metastasis were obtained from all of these patients. The operation was defined as curative if no distant metastases were found (M0) and there was no residual tumor (R0) (n = 305, 61.9%). Patients without distant metastases and who were therefore candidates for potentially curative surgery and who had residual tumor after the operation (R2) (n = 0) or resection margins with tumor (R1) (n = 14, 2.8%) were excluded from the study. Furthermore, patients who turned out to have M1 disease in the final histopathologic specimen were also excluded (n = 4, 0.8%) because during the operation the team believed themselves to be in a curative setting.
Staging and histopathologic differentiation was obtained from the hospital records. For patients in whom no tumor was resected during the operation, this information was obtained from biopsies during the operation or from the preoperative endoscopic specimen.
Definition of Symptoms
Patients were deemed to have major symptoms if they initially presented with gastrointestinal bleeding from the tumor, perforation, ileus, or gastric inlet or outlet obstruction caused by the tumor. All other patients were classified as having minor symptoms.
Gastrointestinal bleeding was defined as the presence of hematemesis, bloody bowel movements, or melena associated with anemia (n = 20). Perforation was diagnosed by free air in the abdomen on plain radiography of the abdomen associated with abdominal pain (n = 3), and ileus was diagnosed in patients who had an acute abdomen with nausea and vomiting combined with radiologic signs of ileus (i.e., large bow-shaped loops in a ladder pattern and fluid levels in the intestine) (n = 4). Inlet or outlet obstruction of the stomach was diagnosed if the patient presented with recurrent dysphagia or vomiting associated with an endoscopically stenotic tumor of the stomach (n = 48).
For patients undergoing total gastrectomy, proximal and distal gastric resections were grouped under “resection,” whereas those undergoing laparotomy only or bypass surgery were grouped under “exploration.”
Disease-specific long-term survival was calculated, and the patients’ status was determined by follow-up questionnaires. All survival curves exclude hospital mortality and represent disease-specific long-term survival.
Assessment of Health-related Quality of Life
In 1998 the model Center of Operative Oncology was established by the Department of Surgery of the University of Kiel. A main focus of this project was to promote a high standard of treatment for cancer patients, thereby improving their survival as well as their QoL. A routine assessment of QoL started before the operation and continued for up to 2 years as part of quality management. Patients were given questionnaires preoperatively (baseline), before discharge, and 3-, 6-, 12-, and 24 months after surgery. All patients with metastatic gastric cancer who underwent surgery from 1998 to 2001 in the Department for General and Thoracic Surgery were included in the QoL analysis. Because of the limited median survival in the cohort and to obtain groups of sufficient size (n > 10), only QoL data for three time points (i.e., preoperatively, before discharge, and 3 months after surgery) were included in this analysis. Because of the small sample a cross-sectional analysis was chosen; that is, all patients providing preoperative QoL data were compared to all those providing QoL data before discharge and 3 months after surgery. In total, QoL data were assessed in 50 patients.
Instruments
Health-related quality of life (HRQOL) was assessed using the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30 core questionnaire and a disease-specific module. The EORTC QLQ-C30 is a cancer-specific 30-item questionnaire [10] that incorporates five functional scales (physical, role, cognitive, emotional, social), three symptoms scales (fatigue, pain, nausea/vomiting), and a global health status/QoL scale. There are also a number of single items assessing additional symptoms commonly reported by cancer patients (dyspnea, loss of appetite, insomnia, constipation, diarrhea) and the perceived financial impact of the disease.
In the QLQ-C30 all items have response categories with four levels, from “not at all” to “very much,” except the two items for overall physical condition and overall QoL, which use 7-point items ranging from “very poor” to “excellent.” High functional scale scores represent good levels of functioning, and high scores for symptoms scales or items represent high levels of symptoms or problems [11].
Statistical Analysis
Results are presented as total numbers or means ± SD. All distribution and frequencies were compared using the χ2 test. Age and length of hospital stay were compared by t-test. Because the QoL data were not normally distributed, nonparametric methods were used for the statistical analysis. QoL analysis comparing two groups (patients with major or minor symptoms) was performed with the Mann-Whitney U-test. Differences in more than two groups (i.e., tumor localization) were analyzed via the Kruskal-Wallis test. QoL was scored according to the EORTC QLQ-C30 scoring manual [11]: Scales were calculated when at least half of the items were completed by the patients.
Survival is presented as a Kaplan-Meier curve and was analyzed with a log-rank test. A p value of less than 0.05 was considered significant.
Results
Histopathologic Findings
Of the 169 patients with incurable gastric cancer, 75 (44.3%) presented with major symptoms and 94 (55.7%) with minor symptoms. The histopathologic features of these two groups are displayed in Table 1. The patients had similar characteristics (Table 1). There were no differences in the distribution of the T stages according to the TNM classification following the International Union Against Cancer (UICC), nor were there any differences in the numbers and sites of metastases [lymph node (N3 node metastasis)], peritoneal seeding, or metastasis to the liver or other sites.
Demographic and Operative Characteristics
The clinicopathologic characteristics of the two groups of patients are shown and compared in Table 2. No differences of the given characteristics were detectable. Patients presenting with major symptoms were operated on using the same approaches as for patients presenting with minor symptoms.
Postoperative Characteristics
Patients with incurable gastric cancer had high hospital mortality (11.3%), with no differences between patients with major (11/14.6%) or minor (8/8.5%) symptoms (Table 3). Patients were similar regarding the characteristics evaluated in Table 3. With regard to the length of hospital stay, patients with minor symptoms undergoing exploration had a significantly (p < 0.05) shorter length of stay in the hospital than did equivalent patients with major symptoms. Furthermore, patients undergoing exploration with minor symptoms spent significantly less time (p < 0.05) in the hospital overall and postoperatively than did the patients with minor symptoms undergoing resection.
Survival
Patients with minor symptoms had a median survival of 6 months. This was significantly (p < 0.05) longer than patients with major symptoms (4 months) (Fig. 1). The disease-specific survival rate of these patients was not influenced by the type of operation (Fig. 2). Patients undergoing exploration survived only 5 months (median), regardless of the intensity of the preoperative symptoms. In contrast, patients with major symptoms undergoing resection died after 4 months (median), whereas those with minor symptoms survived 6 months (median) (log-rank, p < 0.05).
Disease-specific survival according to preoperative symptoms classified as minor or major and type of operation for patients with metastatic (stage IV) gastric cancer excluding operative deaths. Major-Res.: patients with major symptoms undergoing resection; Major-Expl.: patients with major symptoms undergoing laparotomy or the bypass procedure; Minor-Res.: patients with minor symptoms undergoing resection; Minor-Expl.: patients with minor symptoms undergoing laparotomy or the bypass procedure. Data are presented as a Kaplan-Meier curve. #Log-rank test: p < 0.05 major vs. minor.
To determine if patients undergoing resection may profit from an extended lymphadenectomy (D2 lymphadenectomy) or even splenectomy, the disease-specific survivals of these two conditions were evaluated (Fig. 3). Patients with minor symptoms survived significantly longer (p < 0.05), irrespective of the extent of the lymphadenectomy (after D1 and D2 lymphadenectomy), than did the group of patients with major symptoms (Fig. 3A). Furthermore, patients with minor symptoms survived significantly longer than their counterparts with major symptoms following splenectomy and if the spleen was preserved (Fig. 3B). No significant differences were seen within the groups.
Disease-specific survival according to preoperative symptoms classified as minor or major and extent of lymphadenectomy (A) or splenectomy (B) for patients with metastatic (stage IV) gastric cancer undergoing tumor resection excluding operative deaths. Major D2: patients with major symptoms undergoing D2 lymphadenectomy; Major D1: patients with major symptoms undergoing D1 lymphadenectomy; Minor D2: patients with minor symptoms undergoing D2 lymphadenectomy; Minor D1: patients with minor symptoms undergoing D1 lymphadenectomy; Major-Spl: patients with major symptoms without splenectomy; Major+Spl: patients with major symptoms undergoing splenectomy; Minor-Spl: patients with minor symptoms without splenectomy; Minor+Spl: patients with minor symptoms undergoing splenectomy. Data are presented as a Kaplan-Meier curve. #Log-rank test: p < 0.05 major vs. minor.
Quality of Life
According to the analysis of the EORTC QLQC30 questionnaires, patients with major symptoms had significantly more melena (minor 1.0 ± 0; major 2.06 ± 1.2; p < 0.05, t-test) and more nausea and vomiting before the operation. These symptom scales equalized between the two groups postoperatively (Fig. 4).
EORTC-QLQ30 scales according to preoperative symptoms classified as minor or major for patients with metastatic (stage IV) gastric cancer preoperatively (A), before discharge (B), and 3 months after surgery (C). PF: physical functioning; RF: role functioning; EF: emotional functioning; CF: cognitive functioning; SF: social functioning; GH: global health; FA: fatigue; NV: nausea/vomiting; PA: pain; DY: dyspnea; SL: insomnia; AP: appetite loss; CO: constipation; DI: diarrhea; FI: financial difficulties. Data are presented as means. # t-test: p < 0.05 for major vs. minor.
In general, QoL was not different in patients with major or minor symptoms before operation. Before discharge, patients with major symptoms perceived their QoL as higher than patients with minor symptoms. For instance, they estimated their role functioning significantly better than that of the patients with minor symptoms. This trend continued following discharge. At 3 months after the operation, patients with major symptoms estimated their QoL in general better than those who had minor symptoms. The difference was statistically significant (p < 0.05) for social functioning (Fig. 4C).
Discussion
In the present study we demonstrated that postoperative long-term survival of patients with metastatic gastric cancer correlates with their preoperative symptoms. Surgery (resection versus exploration) had no influence on the median survival or QoL regardless of the degree of symptoms. All patients except one man died during the observation period. The survivor had pT2pN2pM1 (hepatic metastasis) adenocarcinoma of the middle third with minor symptoms. He underwent total gastrectomy with D2 lymphadenectomy in 1993 at age 72 years and is currently alive without proven metastasis.
The distribution of demographic, operative, postoperative, and histopathologic characteristics were comparable for the two groups of patients with minor or major symptoms. Despite these well distributed groups of patients, those presenting with major symptoms had a median survival of 4 months and those with minor symptoms 6 months. Although this difference was statistically significant, the difference of 2 months does not seem to be clinically important. The median survival of around 4 to 6 months is in accordance with the results of other studies of patients with incurable gastric cancer [8, 12, 13]. In the study of Kikuchi et al. [13] the intensity of preoperative symptoms had no influence on survival. However, in this study only symptoms related to gastric inlet or outlet obstruction were recorded, whereas in the present study bleeding, ileus, and perforation were also included.
Some studies reported a potential benefit from resection in a palliative setting [1, 2, 3, 12, 14], whereas other studies could not demonstrate any advantage of resection in such patients [5, 6, 7]. In contrast to reports by Doglietto et al. [12] and Sugarbaker and Yonemura [1], resection of the tumor had no influence on the median survival. Studies promoting the rationale of tumor resection/debulking, even for metastatic disease, originate from the early 1980s [3, 15, 16]. These studies demonstrated a beneficial effect of tumor resection in samples of 40 to 90 patients, with an increase in median survival from 4 to 5 months to 10 to 12 months. In the present study the median survival was 4 to 6 months irrespective of tumor resection or only laparotomy/gastrojejunostomy.
With almost 170 patients, our study represents one of the largest cohorts studied in this field. Furthermore, patients of the studies that reported a beneficial effect of tumor resection were only partially comparable with our cohort. In the present study only patients with metastatic disease (pTxNxM1, stage IV), discovered intraoperatively at the latest, were included. We excluded patients with residual tumor at the surgical margins (R1 resection) after potentially curative surgery as well as those patients for whom only the final histopathologic report showed distant metastasis. This reflects the clinical situation in which the surgeon, knowing it is a palliative situation, has the choice to either resect the tumor or perform a gastrojejunostomy. Doglietto and associates [12], who reported a benefit of tumor resection in a palliative setting, also included patients with residual tumor after potentially curative surgery (R1 resection). In contrast, Hanazaki et al. [14] included patients with M1 and T4 staging. Therefore, because survival following R1 and R2 resections on the one hand and survival of those with metastatic disease and locally advanced disease on the other hand are different, the cohort presented in this study and those of Doglietto et al. [12] and Hanazaki et al. [14] differ. The choice of a homogeneous population in our study might have led to the lack of beneficial effects of tumor resection observed in this study. Whereas Sugarbaker and Yonemura [1] and Kaibara et al. [15] were able to demonstrate beneficial effects of tumor resection combined with local peritonectomy in patients with peritoneal metastasized gastric cancer, Kikuchi et al. [7] failed to find these beneficial effects under the same circumstances, regardless of the site of the peritoneal seeding, when tumor resection was combined with local peritonectomy and D2 lymphadenectomy. The extent of the lymphadenectomy (D1 versus D2) had no influence on survival in our study, which is in accordance with the findings of Kikuchi et al. [7]. Moreover, we have demonstrated that splenectomy has no beneficial effect in patients with metastatic gastric cancer. This is in accordance with the observation that splenectomy also has no beneficial effects on long-term survival of patients with curable gastric cancer, and it increases morbidity [17, 18].
In addition to the possible survival advantage, the rationale for tumor resection in the palliative setting was to avoid possible complications such as bleeding or obstruction, suggesting that they are part of the natural course of this disease. Therefore, one could speculate that patients presenting with major symptoms have more advanced disease and therefore die earlier. In the present study, we found that patients with major symptoms die significantly earlier than those with minor symptoms. However, the histopathologic findings (the distribution of T stage and ≥ N3 lymph node metastases), the site of metastasis, and the histologic differentiation of patients with minor and major symptoms were similar. A possible influence of the site of metastasis has been reported by Hanazaki et al. [14]. They found a shorter survival for patients with liver metastasis. In the present study, the distribution of liver and other metastases was equal. Although this suggests that gastric cancer does not necessarily lead to complications such as bleeding, perforation, or obstruction, this question was not one of those explored by our study.
Quality of life is an important outcome in patients undergoing surgery in general and oncologic resection in particular. In patients with metastatic disease and a median survival of 5 to 10 months, QoL becomes even more important. The QoL was determined by the EORTC QLQC30 questionnaire, a reliable, standardized instrument [10, 11] that has not been used previously in patients with palliative gastric cancer. Other studies evaluating QoL used such factors as relief of preoperative symptoms [12] or “hospital-free survival” [6], but they were not evaluated for their reliability in terms of QoL. In our study, the preoperative QoL was influenced by the definitions of individuals with major and minor symptoms, which revealed a significantly higher proportion of patients with nausea/vomiting and melena among those with major symptoms.
It is remarkable that despite these major symptoms, the preoperative scales were not different for the two groups. Furthermore, postoperatively there were no obvious differences between the groups in terms of their QoL. The only exceptions were that role functioning was better before discharge in patients who had major symptoms initially, and social functioning was better in the same group of patients after 3 months. One might speculate that patients initially compromised by major symptoms estimated their postoperative QoL as relatively better than those who had only mild symptoms before the operation and, then, after the operation learned that they had incurable disease. However, preoperatively patients with minor symptoms perceived their QoL as no better than did patients with major symptoms: They had almost identical scores for the single items.
Finally, patients with minor symptoms who underwent only laparotomy or gastrojejunostomy stayed 8.5 days less in the hospital than patients with major symptoms. In addition, they stayed about a week less than patients with minor symptoms who underwent tumor resection. With a median survival of 4 to 6 months and with no influence by the type of operation, 7 to 8 days in the hospital seem to be a significant percentage of the life expectancy. Furthermore, the hospital mortality for patients undergoing surgery for metastatic gastric cancer was significantly higher than that for patients undergoing surgery for curable disease (11.3% vs. 4.0%), also having a negative impact on the life expectancy of this group of patients.
Conclusions
This study demonstrated that the intensity of preoperative symptoms influences postoperative survival, with a significantly lower survival rate for patients with major symptoms. Survival was not influenced by tumor resection, extended lymphadenectomy, or splenectomy. Furthermore, the pre- and postoperative QoL is partially influenced by the intensity of the preoperative symptoms, with a trend to a better QoL in patients with major preoperative symptoms.
Endoscopic or surgical treatment is necessary in patients with major symptoms. Because patients with minor symptoms do not benefit from tumor resection or lymphadenectomy and splenectomy, and their QoL is not enhanced following operation, the need for any endoscopic or surgical therapeutic approach requires careful consideration. Therefore, to stratify patients for therapy, preoperative transgastric ultrasonography or staging laparoscopy (or both) might be helpful. Moreover, the possible benefits from neoadjuvant/palliative therapy under these circumstances should be elucidated.
Résumé.
Les patients atteints de cancer de l’estomac incurable se présentent parfois avec des symptômes modérés ou ailleurs, nécessitent un traitement d’urgence. On a évalué ici l’influence de l’intensité des symptômes préopératoires sur la survie postopératoire et la qualité de vie (QdV) chez des patients soignés en situation palliative. Dans une analyse de cohorte historique de 492 patients porteurs de cancer gastrique traités entre 1992 et 2001, 169 (34.4%) patients avaient une maladie incurable (i.e., pTxNxM1). Les patients ont été classés selon qu’ils avaient des symptômes majeurs lorsqu’ils se sont présentés comprenant soit une hémorragie du tube digestif supérieur (par exemple, hématémèse ou du sang dans les selles), soit un syndrome d’obstruction gastrique (c’est-à-dire une sténose prouvée endoscopiquement ou symptomatique) ou une perforation en rapport avec la tumeur. Tous les autres patients ont été définis comme ayant des symptômes mineurs. La QdV a été évaluée prospectivement par le questionnaire EORTC, rempli par les patients en préopératoire, avant leur sortie et trois mois après l’intervention. Les résultats ont été analysés par le test «u» de Mann-Whitney. La survie et les données démographiques et histopathologiques ont été évaluées et analysées, respectivement, par les tests de log-rank et χ2. 75 des 169 patients (44.3%) se sont présentés avec des symptômes majeurs et 94 (55.7%), avec des symptômes mineurs. La répartition des patients ayant eu une résection ou une exploration était comparable entre les deux groupes [majeure: 61 (81.5%)/14 (18.5%); mineure: 77 (81.9%)/17 (18.1%)]. En dépit des données démographiques et histopathologiques comparables, associées à une mortalité et morbidité hospitalière similaire (14.6% vs. 8.5%/49.3% vs. 40.4%), la médiane de survie dans les deux groupes a été, respectivement, de 4 et 6 mois (p < 0.05). Ce résultat n’a pas été influencé par le type d’intervention. La QdV ne différait pas entre les patients se présentant avec des symptômes majeurs ou mineurs avant l’intervention ou trois mois après. Cependant, il y avait significativement plus de symptômes préopératoires comme des nausées/vomissements chez les patients présentant des symptômes majeurs. Chez les patients porteurs de cancer gastrique incurable chirurgicalement, l’intensité préopératoire des symptômes a un impact significatif sur la survie et la QdV qui n’a pas été influencé par le type d’intervention. La décision d’opérer le patient présentant des symptômes mineurs doit être dûment réfléchie
Resumen.
Los pacientes con cáncer gástrico avanzado, incurable, pueden presentar una sintomatología leve o bien requerir intervención terapéutica inmediata. En un contexto paliativo, se hizo la evaluación de la influencia de la intensidad de los síntomas preoperatorios sobre la supervivencia postoperatoria y la calidad de vida (CDV). En el análisis histórico de una cohorte de 492 pacientes con cáncer gástrico tratados entre 1992 y 2001, 169 (34.4%) presentaban enfermedad incurable (i.e., pTxNxM1). Los pacientes fueron clasificados en aquellos con síntomas mayores si presentaban sangrado gastrointestinal alto (i.e., hematemesis o deposiciones sanguinolentas), obstrucción de entrada o salida del estómago (i.e., estenosis sintomática y comprobada por endoscopia) o perforación causada por el tumor. Todos lo demás fueron clasificados como con sintomatología menor. La CDV fue evaluada prospectivamente mediante un cuestionario, el cual fue dado a los pacientes antes de la operación, antes del egreso hospitalario y a los 3 meses luego de la operación utilizando la prueba u de Mann-Whitney. También se hizo la valoración estadística de la supervivencia, los aspectos demográficos y las características histopatológicas. 75 de 169 pacientes (44.3%) presentaron síntomas mayores y 94 (55.7%) síntomas menores. La distribución de los que fueron sometidos a resección o exploración apareció similar en los dos grupos [mayor: 61 (81.5%)/14(18.5%); menor: 77 (81.9%)/17 (18.1%)]. A pesar de las comparables características demográficas e histopatológicas con igual mortalidad hospitalaria y morbilidad (14.6% vs 8.5%/49.3% vs 40.4%), la media de supervivencia en los dos grupos fue 4 y 6 meses, respectivamente (p < 0.05), lo cual no apareció influenciado por el tipo de operación. La CDV no se vio diferente entre el grupo con síntomas mayores o menores antes de la operación o a los 3 meses postoperatorios. Sin embargo, síntomas preoperatorios tales como náusea/vómito y melena aparecieron con significativa mayor incidencia en pacientes con síntomas mayores. En pacientes con cáncer gástrico incurable la intensidad preoperatoria de síntomas tiene un impacto significativo sobre la supervivencia y sobre la CDV, lo cual no es influenciado por la operación. La indicación para realizar cirugía en pacientes con síntomas menores requiere cuidados a consideración.
References
PH Sugarbaker Y Yonemura (2000) ArticleTitleClinical pathway for the management of resectable gastric cancer with peritoneal seeding: best palliation with a ray of hope for cure Oncology 58 96–107 Occurrence Handle10.1159/000012086 Occurrence Handle1:STN:280:DC%2BD3c7ntFOiuw%3D%3D Occurrence Handle10705236
JR Monson JH Donohue DC McIlrath et al. (1991) ArticleTitleTotal gastrectomy for advanced cancer: a worthwhile palliative procedure Cancer 68 1863–1868 Occurrence Handle1:STN:280:By2D3crivVM%3D Occurrence Handle1717128
S Meijer OJ Bakker ParticleDe HF Hoitsma (1983) ArticleTitlePalliative resection in gastric cancer J. Surg. Oncol. 23 77–80 Occurrence Handle1:STN:280:BiyB3MjltlU%3D Occurrence Handle6190045
A Schmid B Kremer (2000) ArticleTitleChirurgische Prinzipien beim Magenkarzinom Chirurg 71 974–986 Occurrence Handle10.1007/s001040051168 Occurrence Handle1:STN:280:DC%2BD3cvmt1Oqsg%3D%3D Occurrence Handle11013820
R Kuhn K Ridwelski (2000) ArticleTitleDie Therapie des fortgeschrittenen Magenkarzinoms Akt. Studienkonzepte Zentralbl. Chir. 125 176–181
K Ouchi T Sugawara H Ono et al. (1998) ArticleTitleTherapeutic significance of palliative operations for gastric cancer for survival and quality of life J. Surg. Oncol. 69 41–44 Occurrence Handle10.1002/(SICI)1096-9098(199809)69:1<41::AID-JSO8>3.0.CO;2-K Occurrence Handle1:STN:280:DyaK1cvjtlymtg%3D%3D Occurrence Handle9762890
S Kikuchi Y Arai N Kobayashi et al. (2000) ArticleTitleIs extended lymphadenectomy valuable in palliatively gastrectomized patients with gastric cancer and simultaneous peritoneal metastasis? Hepatogastroenterology. 47 563–566 Occurrence Handle1:STN:280:DC%2BD3c3ltFygtw%3D%3D Occurrence Handle10791239
J Schmier A Elixhauser MT Halpern (1999) ArticleTitleHealth-related quality of life evaluation of gastric and pancreatic cancer Hepatogastroenterology. 46 1998–2004 Occurrence Handle1:STN:280:DyaK1MzlslCmsQ%3D%3D Occurrence Handle10430384
A Thybusch-Bernhardt C Schmidt T Kuchler et al. (1999) ArticleTitleQuality of life following radical surgical treatment of gastric carcinoma World J. Surg. 23 503–508 Occurrence Handle10085401
NK Aaronson S Ahmedzai B Bergman et al. (1993) ArticleTitleThe European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology J. Natl. Cancer Inst. 85 365–376 Occurrence Handle10.1093/jnci/85.5.365 Occurrence Handle1:STN:280:ByyC28vivVc%3D Occurrence Handle8433390
Fayers P, Aaronson NK, Bjordal D, et al. EORTC QLQ-C30 Scoring Manual, 2nd edition, Paris, EORTC
GB Doglietto F Pacelli P Caprino et al. (2000) ArticleTitleSurgery: independent prognostic factor in curable and far advanced gastric cancer World J. Surg. 24 459–464 Occurrence Handle10.1007/s002689910073 Occurrence Handle1:STN:280:DC%2BD3c7ntlOqug%3D%3D Occurrence Handle10706920
S Kikuchi O Tsutsumi N Kobayashi et al. (1999) ArticleTitleDoes gastrojejunostomy for unresectable cancer of the gastric antrum offer satisfactory palliation? Hepatogastroenterology. 46 584–587 Occurrence Handle1:STN:280:DyaK1M3ksFGnuw%3D%3D Occurrence Handle10228865
K Hanazaki H Sodeyama Y Mochizuki et al. (2001) ArticleTitlePalliative gastrectomy for advanced gastric cancer Hepatogastroenterology. 48 285–289 Occurrence Handle1:STN:280:DC%2BD3M7mvVeltA%3D%3D Occurrence Handle11268986
N Kaibara T Okamoto O Kimura et al. (1983) ArticleTitlePossible role of lymph node dissection in the surgical treatment of gastric cancer with disseminating peritoneal metastasis Jpn. J. Surg. 13 404–408 Occurrence Handle1:STN:280:BiuC3sbmtlY%3D Occurrence Handle6668774
S Koga H Kawaguchi H Kishimoto et al. (1980) ArticleTitleTherapeutic significance of noncurative gastrectomy for gastric cancer with liver metastasis Am. J. Surg. 140 356–359 Occurrence Handle1:STN:280:Bi6D3sjit1E%3D Occurrence Handle6158880
A Schmid A Thybusch B Kremer et al. (2000) ArticleTitleDifferential effects of radical D2-lymphadenectomy and splenectomy in surgically treated gastric cancer patients Hepatogastroenterology. 32 579–585
Y Noguchi Y Yamamoto S Morinaga et al. (2002) ArticleTitleDoes pancreaticosplenectomy contribute to better survival? Hepatogastroenterology. 47 1436–1440
Acknowledgments.
This study was supported by funds from the Department for General and Thoracic Surgery, University of Kiel, Kiel, Germany.
Author information
Authors and Affiliations
Corresponding author
Additional information
Andreas Schmid, M.D. is now at the Department of Surgery, DRK-Krankenhaus Mölln-Ratzeburg, Röpersberg 2, 23909 Ratzeburg, Germany
Rights and permissions
About this article
Cite this article
Kahlke, V., Bestmann, B., Schmid, A. et al. Palliation of Metastatic Gastric Cancer: Impact of Preoperative Symptoms and the Type of Operation on Survival and Quality of Life. World J. Surg. 28, 369–375 (2004). https://doi.org/10.1007/s00268-003-7119-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-003-7119-0