Abstract
Background
The number of patients undergoing mastectomy and immediate breast reconstruction with tissue expanders followed by post-mastectomy radiotherapy (PMRT) is exponentially increasing. To reduce the rate of complications, in 2011, the senior author of this manuscript described the use of protective lipofilling in patients undergoing unplanned PMRT to the expander with a specific protocol aiming to decrease the rate of complications.
Objectives
A study was performed to evaluate the thickness of the breast irradiated tissue to create a standard pattern of “protective” lipofilling infiltration on limited key areas that could re-establish a thickness similar to non-radiotreated tissues.
Methods
We studied 15 patients who had modified radical mastectomy (MRM) with immediate breast reconstruction with tissue expanders and PMRT (Group 1) before expansion (Time1), before PMRT (Time2), after PMRT (Time3), 3 months after “protective” lipofilling (Time4), and 6 months after “protective” lipofilling (Time5). As a control group, we studied 15 patients who had MRM and immediate breast reconstruction with tissue expanders that would not undergo PMRT (Group 2) at the same time points of GROUP 1 (Time1,2,3). Tissue thickness was studied in specific areas using ultrasounds (US) and magnetic resonance imaging (MRI).
Results
US and MRI measurements obtained 6 weeks after PMRT and 3 months after lipofilling showed an initial decrease and then an average increase in tissue thickness reaching values even higher than the non-radiotreated control group.
Conclusions
This preliminary report shows how a one-step “fat belt” surgical pattern of lipofilling delivered to central “selected” areas of the breast can achieve adequate tissue thickness in patients who underwent breast reconstruction with PMRT reaching a thickness similar (and in most cases higher) to non-radiotreated tissues. Further follow-up studies are needed to analyze long-term complications of tissue thinning such as ulceration and implant exposure, in comparison with the “fat capsule” pattern.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The number of patients undergoing mastectomy and immediate breast reconstruction with tissue expanders followed by post-mastectomy radiotherapy (PMRT) is exponentially increasing [1,2,3,4,5,6]. Several studies are now expanding adjuvant radiotherapy indications, currently including patients with stage II cancers and less than four involved nodes [1, 7,8,9,10]. As a consequence, immediate and delayed complications caused by PMRT, such as capsular contracture, infection, ulceration, and implant exposure [11,12,13,14], are expected to increase. In 2011, the senior author (DR) of this manuscript described the use of protective lipofilling in patients undergoing unplanned PMRT to the expander with a specific protocol (two lipofillings 6 weeks after PMRT to the expander followed by substitution with definitive implant 3 months after lipofilling) [15, 16] aiming to decrease the rate of complications. Since then, the indications have been broadened (2013) with excellent results. PMRT is no longer considered a contraindication to breast reconstruction with an expander implant [15,16,17,18,19,20]. The application of this protocol led to lower rates of local infection/ulceration with final extrusion of the implant and Baker 4 capsular contracture, achieving comparable results to those of reconstructed patients who did not receive PMRT [15,16,17,18,19,20]. Throughout the years, this approach has gained wide consensus, becoming very popular, especially in Italy, as evidenced by the papers published by Bonomi [21] and Majone [22].
However, in our first case series [15, 16], protective lipofilling was applied all over the expanded irradiated skin, thus creating a sort of “fat capsule.” As remarked in our previous studies [15, 16], the reduction of the rate of complications was considerable. Nevertheless, two sessions of lipofilling were usually necessary to reach this goal. Subsequently we focused our attention on those areas that were considered at higher risk of ulceration and implant exposure, to detect “key zones” that would benefit the most from “fat protection.” As far as we know, currently, there are no studies analyzing ulceration and implant exposure rates, depending on the different irradiated areas of the breast.
However, in our experience, areas localized along the Stewart mastectomy scar, such as the middle third of the breast, the parasternal area, below the retracted pectoralis major muscle, were considered at higher risk for such complications (Figs. 1a–2b). Tissues usually become thin after PMRT, especially in the zones previously mentioned which would benefit the most from targeted fat coverage that could be achieved in a single-stage procedure. In this regard, we identified “key areas” on the expanded irradiated skin and measured the tissue thickness of the expanded irradiated tissue to create a standard pattern of protective lipofilling infiltration that could re-establish a thickness similar to non-radiotreated tissues.
Methods
From September 2015 to April 2016, 75 patients underwent immediate breast reconstruction with expanders after MRM (modified radical mastectomy) at our Institution. Fifteen out of 75 patients received PMRT to the expander. These non-consecutive female patients (Group 1) were studied before expansion (Time1), before PMRT (Time2), after PMRT (Time3), 3 months after protective lipofilling (Time4), and 6 months after protective lipofilling (Time5). Inclusions criteria were: BMI ≤ 30, no smoking, and no diabetes.
We enrolled 15 non-consecutive female patients as a control group. They had MRM and immediate breast reconstruction with tissue expanders that would not undergo PMRT (Group 2), and they were controlled at the same time points as GROUP 1.
Inclusions criteria in Group 2 patients were the same as reported for Group 1.
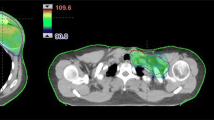
Tissue thickness of selected areas was evaluated using ultrasound (US) (EsaoteMylab 50 with a linear array ultrasound probe with a frequency of 7.5 MHz) and MRI (Siemens Magnetom1 T—T2 TIRM sequences). US and MR imaging were analyzed by two dedicated breast radiologists. The areas selected for evaluation were: (A) at the inframammary fold, (B) the parasternal area, at the end of the Stewart mastectomy scar, and (C) at the point of maximal tissue expansion, usually located in the middle of the mastectomy scar and (D) in the middle of the area located above the pectoralis muscle, 4 cm from the mastectomy scar (Fig. 3). Following MRM, all patients were reconstructed with medium height anatomic expanders (Mentor SILTEX Medium Height Contour Profile) and total muscle coverage, and a drain was inserted.
Female patient, 49 years old, treated with tissue expander and PMRT. Clinical view of the measured areas. The dots stand for the measured areas. The dotted line stands for the inframammary fold. The lower continuous line stands for the mastectomy scar. The upper continuous line stands for the lower border of the pectoralis major muscle
Expanders were inflated every week with 50 ml of saline, exceeding 10% of the maximum indicated volume. Group 1 patients were then treated with PMRT, according to the “AIRO” (Associazione Italiana Radioterapia Oncologica) 2013 guidelines, with a standard dose of 50 Gy divided into 25 fractions of 2 Gy over 5 weeks [23].
All patients signed a consent form before every procedure referring to the Declaration of Helsinki guidelines. General anesthesia was performed in every case. The fat grafting procedure was scheduled 6 weeks after PMRT for every patient in GROUP 1.
The fat graft was harvested from the abdominal or trochanteric areas, depending on patient’s preference, and then grafted in one single operating session. The average quantity was 120 cc per breast (range: 80–160 cc), using structural fat micrografting. Harvested fresh fat was transferred to 2.5 mL syringes using a three-way stopcock [24, 25] and injected in Group 1 patients subcutaneously and multidirectionally, from superficial to deep layer tissues. Multiple tunnels were created and filled progressively with small amounts of fat, thus avoiding piling up fat cells allowing for easier revascularization. The entire surgical procedure lasted approximately 50 min. The injected area resembling a “fat belt” occupies a transverse area with the lower border located 3 cm above the inframammary fold, the upper border located 4 cm above the Stewart mastectomy scar, reaching the palpable margin of the retracted pectoralis muscle. We define “fat belt” as the concave area going from the medial margin of the breast to the lateral one (Fig. 4). Measurements in Group 1 patients were taken before expansion, after expansion, and after PMRT and then repeated 3 months after lipofilling.
In Group 2 patients, measurements were recorded before and after full expansion, at the level of the same “areas” as for Group 1 patients. Statistical comparisons were made using Fisher’s exact test. Values of p lower than 0.05 were considered statistically significant. A maximum follow-up of 12 months has been applied for every patient in both groups searching for any complication. Longer follow-up could not be performed as permanent implants were inserted no further than 12 months after the mastectomy.
Results
Patients in Group 1 had a mean BMI of 23.44 (range: 19.55–28) and a mean age of 53 (range: 42–68). The tissue expander was filled reaching an average of 300 cc in Group 1 and 325 cc in Group 2. In Group 1 patients, measurements were taken before expansion (Time1), before PMRT (Time2), after PMRT (Time3), 3 months after protective lipofilling (Time4), and 6 months after protective lipofilling (Time5). In this group, the inframammary fold (A) had an average thickness of 1.89 cm (range: 1.7–2.08 cm) before expansion (DS (σ): 0.09), slightly decreased after expansion (average: 1.82 cm, range: 1.65–2 cm. DS (σ): 0.08), and did not have large variations after PMRT and lipofilling. The parasternal area (B) had an average initial thickness of 1.30 cm (range: 0.95–1.65 cm) (DS (σ): 0.18). This area had an important decrease after expansion (average: 0.73 cm, range: 0.55–1 cm, DS (σ): 0.14), and also after PMRT (average: 0.67 cm, range: 0.48–0.95 cm, DS (σ): 0.14). After lipofilling, thickness in this point returned to an average of 1.17 cm (range: 0.74–1.42 cm, DS (σ): 0.20), with an average increase of 0.50 cm. The central mastectomy scar (C) was greatly affected by both expansion and radiotherapy. The average of initial thickness was 1.39 cm (range: 1.15–1.6 cm, DS (σ): 0.15), 0.88 cm (average) after expansion (range: 0.6–1.2 cm, DS (σ): 0.13), and 0.75 (average) after PMRT (range: 0.55–0.84 cm, DS (σ): 0.07), and returned to 1.24 (average) after lipofilling (range: 1.14–1.45 cm, DS (σ): 0.12).
Finally, the pectoralis measurement (D) was only partially affected by expansion and PMRT, with an initial average thickness of 1.62 cm (range: 1.45–1.95 cm, DS (σ): 0.14), down to 1.45 (average) after expansion (range: 1.25–1.7 cm, DS (σ): 0.15), and 1.22(average) after PMRT (range: 0.98–1.55 cm, DS (σ): 0.15), and remained almost the same after lipofilling (Tables 1, 2, 3, 4, 5) (Figs. 5, 7). Measurements taken 6 months after protective lipofilling showed a stable behavior of subcutaneous tissue with minimal thickness variations.
Group 1 average measurement progression. (A: inframammary fold, B: parasternal area, C: mastectomy scar, D: above the pectoralis muscle) (1: pre-expansion, 2: post-expansion, 3: pre-PMRT, 4: post-“fat belt,” 5: 6 months follow-up). As shown in the graph, there was a notable increase in thickness in the treated areas
Patients in Group 2 had a mean BMI of 24.25 (range: 20.22–27.50) and a mean age of 53 (range: 44–66). Measurements in Group 2 patients were taken in the first two phases and at 6 months follow-up and had no significant variations from Group 1 (Tables 5, 6, 7, 8) (Figs. 6, 7). Statistical comparisons made with Fisher’s exact test gave these results: As per the measurements taken at the inframammary fold (A) and at the area above the pectoralis muscle (D), the p values were, respectively, 1 and 0.5, which is absolutely normal due to the lack of changes in thickness in these two areas. On the other hand, p values for the measurements taken at the parasternal area and at the mastectomy scar were, respectively, 0.01 and 0.006 due to the large changes, in terms of thickness, that these two areas went through (Figs. 5, 6, 7). Local complications such as ulceration or implant exposure were not noticed (Figs. 8a–9b). One seroma was noted in Group 1 patients, and one hematoma requiring surgery in Group 2 was described after a maximum follow-up of 12 months before permanent implant insertion (mean follow-up 9 months, ranged from 4 to 12 months in Group 1 patients and mean follow-up 8 months, ranged from 5 to 12 months in Group 2 patients).
Group 2 average measurement progression. (A: inframammary fold, B: parasternal area, C: mastectomy scar, D: above the pectoralis muscle) (1: pre-expansion, 2: post-expansion, 3: 6 months follow-up). As shown in the graph, there was a notable decrease in thickness in the treated areas with no significant variations from Group 1 before PMRT
Group 1 and 2 average measurement progression. (A: inframammary fold, B: parasternal area, C: mastectomy scar, D: above the pectoralis muscle) (1: Group 1 pre-expansion, 2: Group 1 post-expansion, 3: Group 1 pre-PMRT, 4: Group 1 post-“fat belt,” 5: Group 1 at 6 months follow-up, 6: Group 2 pre-expansion, 7: Group 2 post-expansion, 8: Group 2 at 6 months follow-up)
a Female patient, 52 years old, included in study Group 1, treated with tissue expander and PMRT. Clinical view after maximum expansion of the tissue expander. b Same patient as a. Clinical view 12 months after the “fat belt” protective lipofilling. No suffering skin areas were noticed during the follow-up
a Female patient, 48 years old, included in study Group 2, treated with tissue expander without PMRT. Clinical view after maximum expansion of the tissue expander. No lipofilling was performed. b Same patient as a. Clinical view 12 months after insertion of mammary implant. No suffering skin areas were noticed during the follow-up
Discussion
The process of skin and muscle expansion, which takes place during breast reconstruction with expanders and implants, greatly modifies tissue thickness. Thinning of the tissues is greater in the central part of the mastectomy scar, where the focus of pressure applied by the expander is at its greatest. The parasternal area and inframammary fold also suffer from pressure (and weight), whereas the central pectoral area is only marginally affected [26,27,28,29,30].
This phenomenon is exacerbated by radiation damage after PMRT. As widely reported, damage from radiation therapy depends on the dose of radiation, the distribution of hisodoses, the release of a boost of electrons to the scar, and lastly, the use of wedges. In fact, during PMRT, dose distribution is not homogeneous; the hisodose, i.e., the percentage of ionizing radiations absorbed by tissues, is greater in the medial and lateral portions of the breast, reaching up to 108%. This explains how and why these areas are at greater risk of ulceration and implant exposure, together with the central area, where often an additional dose of 10 Gy is given to the scar. Thus, pressure and radiation are the reasons for such a high rate of complications observed in the central areas of the breast. As a matter of fact, when ulceration begins due to extreme thinning, radiated tissue is not able to heal, due to vessel atrophy and sclerosis. Restoring thickness and vessel viability is critical in the central breast quadrant, and this can be achieved with lipofilling as demonstrated in many studies [31,32,33]. Infiltrating fat in the upper breast quadrants or in the inframammary fold, areas that always have a thickness over 1.0 cm, is not worthwhile, only resulting in additional surgeries, higher costs [14], and eventually a waste of time. In this regard, we identified “key areas” on the expanded irradiated skin that would benefit the most from targeted fat coverage.
The “fat belt” could be achieved in a single-stage procedure, saving time, lowering operative costs, and resulting in a tailored and better performing protection to the most irradiated areas, at greater risk of developing complications. Nevertheless, this paper shows some limitations due to its nature of preliminary report and as a consequence of the lack of a longer term follow-up (which should be at least 36 months), and the need for a larger cohort of patients. More patients and a longer follow-up will be considered for publication in an upcoming paper.
Conclusion
This preliminary report shows how a one-step “fat belt” surgical pattern of lipofilling delivered to central “selected” areas of the breast can achieve adequate tissue thickness in patients who underwent breast reconstruction with PMRT reaching a thickness similar (and in most cases higher) to non-radiotreated tissues. Further follow-up studies are needed to analyze long-term complications of tissue thinning such as ulceration and implant exposure, in comparison with the “fat capsule” pattern.
References
Ragaz J, Olivotto IA, Spinelli JJ, Phillips N, Jackson SM, Wilson KS, Knowling MA, Coppin CM, Weir L, Gelmon K, Le N, Durand R, Coldman AJ, Manji M (2005) Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst 97:116–126
Overgaard M, Nielsen HM, Overgaard J (2007) Is the benefit of postmastectomy irradiation limited to patients with four or more positive nodes, as recommended in international consensus reports? A subgroup analysis of the DBCG 82 b&c randomized trials. Radiother Oncol 82:247–253
NATIONAL COMPREHENSIVE CANCER NETWORK (NCCN) (2008) Clinical practice guidelines in oncology: breast cancer ver. 1.2009. NCCN, Fort Washington
SUPREMO, an MRC Phase III randomised trial to assess the role of adjuvant chest wall irradiationin“intermediate risk” operable breast cancer following mastectomy. http://www.controlled-trials.com/ISRCTN61145589. Accessed 4–11 Jan 2009
Katz A, Strom EA, Buchholz TA, Theriault R, Singletary SE, Mcneese MD (2001) The influence of pathologic tumor characteristics on locoregional recurrence rates following mastectomy. Int J Radiat Oncol Biol Phys 50:735–742
Baildam A, Bishop H, Boland G, Dalglish M, Davies L, Fatah F, Gooch H, Harcourt D, Martin L, Rainsbury D, Rayter Z, Sheppard C, Smith J (2007) Weiler-Mithoff EEe, Winstanley J, Church J. Association of breast surgery at Baso, association of breast surgery at Bapras, training interface group in breast surgery, oncoplastic breast surgery—a guide to good practice. Eur J Surg Oncol 33(Suppl 1):S1–S23
Overgaard M, Jensen MB, Overgaard J et al (1999) Postoperative radiotherapy in high-risk postmenopausal breast-cancer patients given adjuvant tamoxifen: Danish Breast Cancer Cooperative Group DBCG 82c randomised trial. Lancet 353:1641–1648
Whelan TJ, Olivotto I, Ackerman I et al (2011) NCIG-CTG MA- 20: an intergroup trial of regional nodal irradiation in breast Cancer. J Clin Oncol. Abstract presented at the 2011 ASCO annual meeting
Frasier LL, Holden S, Holden T, Schumacher JR, Leverson G, Anderson B, Greenberg CC, Neuman HB (2016) Temporal trends in postmastectomy radiation therapy and breast reconstruction associated with changes in national comprehensive cancer network guidelines. JAMA Oncol 2(1):95–101
Meattini I, Cecchini S, Muntoni C, Scotti V, De Luca Cardillo C, Mangoni M, Bonomo P, Nori J, Casella D, Simoncini R, Orzalesi L, Bianchi S, Livi L (2014) Cutaneous and cardiac toxicity of concurrent trastuzumab and adjuvant breast radiotherapy: a single institution series. Med Oncol 31(4):891
Lam TC, Hsieh F, Boyages J (2013) The effects of postmastectomy adjuvant radiotherapy on immediate two-stage prosthetic breast reconstruction: a systematic review. Plast Reconstr Surg 132(3):511–518
Anker CJ, Hymas RV, Ahluwalia R, Kokeny KE, Avizonis V, Boucher KM, Neumayer LA, Agarwal JP (2015) The effect of radiation on complication rates and patient satisfaction in breast reconstruction using temporary tissue expanders and permanent implants. Breast J 21(3):233–240
El-Sabawi B, Carey JN, Hagopian TM, Sbitany H, Patel KM (2016) Radiation and breast reconstruction: algorithmic approach and evidence-based outcomes. J Surg Oncol. https://doi.org/10.1002/jso.24143
Voineskos SH, Frank SG, Cordeiro PG (2015) Breast reconstruction following conservative mastectomies: predictors of complications and outcomes. Gland Surg 4(6):484–496
Ribuffo D, Atzeni M, Serratore F, Guerra M, Bucher S (2011) Cagliari University Hospital (CUH) protocol for immediate alloplastic breast reconstruction and unplanned radiotherapy. A preliminary report. Eur Rev Med Pharmacol Sci 15:840–844
Ribuffo D, Atzeni M, Guerra M et al (2013) Treatment of irradiated expanders: protective lipofilling allows immediate prosthetic breast reconstruction in the setting of postoperative radiotherapy. Aesthetic Plast Surg 37:1146–1152
Lo Torto F, Vaia N, Casella D, Marcasciano M, Cigna E, Ribuffo D (2017) Delaying implant-based mammary reconstruction after radiotherapy does not decrease capsular contracture: an in vitro study. J Plast Reconstr Aesthet Surg 70:1210–1217
Lo Torto F, Vaia N, Casella D, Marcasciano M, Cigna E, Ribuffo D (2018) Delaying implant-based mammary reconstruction after radiotherapy does not decrease capsular contracture: an in vitro study. J Plast Reconstr Aesthet Surg 71:28–29
Lo Torto F, Vaia N, Ribuffo D (2017) Postmastectomy radiation therapy and two-stage implant-based breast reconstruction: is there a better time to irradiate? Plast Reconstr Surg 139(6):1364e–1365e
Ribuffo D, Vaia N, Petrianni GM (2016) Comparison of delayed and immediate tissue expander breast reconstruction in the setting of postmastectomy radiation therapy. Ann Plast Surg 76(6):743–744
Bonomi S, Misani M, Settembrini F (2012) Radiotherapy and implant-based, two-stage breast reconstruction: how to minimize complications and maximize aesthetic outcomes. Plast Reconstr Surg 130:745e–748e
Maione L, Forcellini D, Vinci V, Lisa A, Caviggioli A, Klinger F (2012) The effects of postmastectomy adjuvant radiotherapy on immediate two-stage prosthetic breast reconstruction: a systematic review. Plast Reconstr Surg 133:729e–730e
La Radioterapia dei Tumori della Mammella Indicazioni e Criteri Guida—AIRO 2013 guidelines
Dessy LA, Marcasciano M, Rossi A, Mazzocchi M (2015) Response to “comments on a simple device for syringe-to-syringe transfer during lipofilling”. Aesthet Surg J 35(7):NP242-3
Dessy LA, Marcasciano M, Pacitti F, Rossi A, Mazzocchi M (2015) A simple device for syringe-to-syringe transfer during lipofilling. Aesthet Surg J 35(1):91–93
Cordeiro PG (2012) Discussion. In: Kronowitz SJ (ed) Current status of implant-based breast reconstruction in patients receiving postmastectomy radiation therapy. Plast Reconstr Surg 130: 513e
Kane WJ, McCaffrey TV, Wang TD et al (1992) The effect of tissue expansion on previously irradiated skin. Arch Otolaryngol Head Neck Surg 118:419–426
Fajardo LF, Berthrong M (1988) Vascular lesions following radiation. Pathol Annu 23:297–330
Goodman CM, Miller R, Patrick CW Jr et al (2002) Radiotherapy: effects on expanded skin. Plast Reconstr Surg 110:1080–1083
Lo Torto F, Cigna E, Kaciulyte J, Casella D, Marcasciano M, Ribuffo D (2017) National breast reconstruction utilization in the setting of postmastectomy radiotherapy: two-stage implant-based breast reconstruction. J Reconstr Microsurg. https://doi.org/10.1055/s-0037-1604389
Pallua N, Pulsfort AK, Suschek C, Wolter TP (2009) Content of the growth factors bFGF, IGF-1, VEGF, and PDGF-BB in freshly harvested lipoaspirate after centrifugation and incubation. Plast Reconstr Surg 123:826e33
Yamaguchi M, Matsumoto F, Bujo H et al (2005) Revascularization determines volume retention and gene expression by fat grafts in mice. Exp Biol Med (Maywood) 230:742e8
Pallua N, Baroncini A, Alharbi Z, Stromps JP (2014) Improvement of facial scar appearance and microcirculation by autologous lipofilling. J Plast Reconstr Aesthet Surg 67(8):1033–1037
Acknowledgements
The authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vaia, N., Lo Torto, F., Marcasciano, M. et al. From the “Fat Capsule” to the “Fat Belt”: Limiting Protective Lipofilling on Irradiated Expanders for Breast Reconstruction to Selective Key Areas. Aesth Plast Surg 42, 986–994 (2018). https://doi.org/10.1007/s00266-018-1120-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-018-1120-3