Abstract
Restoration of the esthetic neck contour is an integral component of facial rejuvenation. Characters of the aging neck include lipodystrophy, platysmal bands and jowls that extend into the neck, reducing the esthetic characters of the lower face. The authors present a new, simplified and economic method to manage platysmal bands as an office procedure under local anesthesia using a standard 18-gauge syringe needle as a cutting tool. The new technique was used on a selected group of female patients classified as non-surgical cases according to Rorich classification. Twenty-five female patients shared in this study, with a follow-up period standardized to 1 year; one patient showed up after 1.5 years with preserved esthetic outcome. One patient showed residual band managed by recutting immediately after bruising and edema resolved. The technique was proven safe regarding important neurovascular structures of the neck. Patients gave no negative comments regarding results of surgery. Kappa statistical analysis showed perfect interobserver agreement between patients and an independent assessor. The authors concluded that the studied new technique is safe, effective, and valuable for management of platysmal bands in a selected group of patients.
Level of Evidence IV This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Restoration of the esthetic neck contour is an integral component of facial rejuvenation. As the anterior neck is often the first region to capture the eye of the observer when viewing an aging face, patients frequently express dissatisfaction with their neck contour during their initial consultation for facial rejuvenation [1]. Characteristic signs of the aging neck include lipodystrophy, platysmal bands (lateral and medial), and jowls that extend into the neck, reducing the esthetic quality of the lower face [2].
Rohrich et al. [1] classified neck aging combinations and their management as follow:
Surgical group:
-
Type I: Excellent skin tone, and lipodystrophy.
-
Type II: Mild skin laxity with or without narrow medial platysmal bands (< 2 cm).
-
Type III: Moderate skin laxity with or without wide platysmal bands (> 2 cm).
-
Type IV: Moderate–severe skin laxity and significant lipodystrophy.
Treatment is tailored according to type, but principles of treatment include fat reduction by liposuction or directly, medial vs. lateral incision of platysma at the level of the thyroid cartilage and medial vs. lateral platysma plication and/or excess skin excision vs waiting for skin redraping.
Non-surgical group:
-
Patients who had previous esthetic neck surgery, e.g., liposuction and have residual platysmal bands.
-
Patients who have excellent skin tone and no lipodystrophy and have only platysmal bands.
These are managed by botulinum toxin injection according to Rorich et al. [1].
The treatment of the non-surgical group is a subject of debate. As some authors adopted the use of botulinum toxin therapy [1, 3, 4], others adopted percutaneous surgical cutting of these bands [5,6,7,8]. Actually closed surgical cutting of these bands is not new; it was reported as early as 1926 by Bourguet [8].
There is another debate among advocates for this percutaneous surgery about the method used. Some advocated cutting by special stainless steel wires (Aptos wire®) [5], some used mini-incisions for dissection and cutting of bands using electrocautary thus modernizing the Bourgeut technique [6], some used a special surgical device [7] and others used ordinary Vicryl® thread to saw the bands [8].
Surgical anatomy considerations [1, 3, 4, 9,10,11,12,13,14]:
The platysma originates from the fascia overlying the pectoralis and deltoid muscles and inserts in multiple points above the angle of the mandible. Its fibers intertwine with the muscles of the lower third of the face before inserting into the SMAS at the level of the commissures helping depression of the lower lip and angle of the mouth. Central fibers insert directly into periosteum of the mandible and help in its depression. Anterior fibers from both muscles either show partial decussation in approximately 75% of the population, total muscular decussation from mandible to the level of the thyroid cartilage (15%) and no decussation (10%). If decussation is absent or partial, the free medial edges can be responsible for most of the anterior neck deformity, which appears as two vertical bands. Sometimes, these bands appear involuntarily while the person is speaking and does not appear at rest.
The superficial cervical fascia envelops the platysma. The platysma is bound to the skin by multiple dense connective tissue bands that anchor the superficial fascia to the underside of the dermis.
The platysma muscle has anatomical relations to important neurovascular structures, and thus, these structures should be protected during any surgical procedure that includes cutting, dissecting, plicating, and/or suturing the platysma muscle. These structures are the marginal mandibular and cervical branches of the facial nerve, the great auricular nerve (GAN), the external jugular vein, and anterior jugular vein.
The platysma muscle function preservation is important for facial expression; it shows expressions like pain and anger by sharing in depression of the lower lip and angle of the mouth.
Aim of the Work
The aim of this work is to present and assess a simple, safe, reliable, and low-cost technique to treat patients with isolated deforming platysmal bands.
Materials and Methods
This is a case series done on 25 female patients complaining of platysmal bands who presented to our outpatient clinic in the period from January 2015 to February 2017. All of the patients were classified into the non-surgical group in the classification suggested by Rorich et al. [1], i.e.,
-
patients with overt platysmal bands, good skin tone, and no fat excess neither superficial nor deep to the platysma.
-
patients with good skin tone and overt platysmal bands after submental liposuction.
All patients were subjected to full clinical history confirming the absence of coagulopathies, uncontrolled hypertension, obligatory antiplatelet and anticoagulants drug administration and of previous surgery in the head and neck (other than liposuction to the submental area); otherwise, patients were excluded from this study.
Full general and local examination was done to each patient including assessment of facial nerve function and the neck bands. Bleeding time and coagulation time were ordered for each patient.
An informed consent was signed by the patients including scientific photography, videos, and scientific publishing.
Marking and Photography
The patients were marked standing or sitting to show the bands better; any bands appear while speaking and any apparent vein closely related to bands were marked. Front, lateral, and oblique view photography was taken to the neck area following the footsteps of Daher [7] to which we added views to the neck with maximum contraction of the platysma.
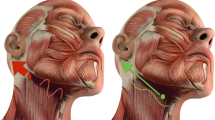
Operative Steps (Fig. 1, 2)
Patients are placed in the supine position with the neck in slight hyperextension. The anterolateral neck is disinfected with povidone iodine solution and draped in a manner that allows the patient to sit if needed.
Marking and operative steps. a, b Marking the bands according to preoperative examination of each patient, any visible vein should be marked. c Local anesthetic injection and band transfixation, needle is secured by hemostat. d, e, f Cutting the band. g, h Successful cutting testing by asking patient to put platysma into action “Bands were obviously cut”
The patient is asked to show the platysmal bands by active contraction of platysma (if the bands were not overt enough the patient is asked to show the bands in the sitting position). The surgeon seizes the band with his index and thumb. Using CarpuleR dental ampules [2% lignocain + adrenaline (1:80,000)] in a 5-cc syringe and 24-gauge needle, the band is percutaneously transfixed (the local anesthetic is injected while transfixing the band in the subcutaneous tissue before the band, within the band and in the subcutaneous tissue after the band). The tip of the injecting needle is secured by an artery forceps to prevent accidental pricking the surgeon. The syringe is removed and the position of the injection needle transfixing the band is confirmed by its up and down motion when the patient contracts and relaxes the platysma. Using the fixed transfixing injection needle as a deep limit to muscle cutting a standard hypodermic 18-gauge injection needle is inserted just superficial and parallel to the transfixing needle stopping just short of penetrating the dermis the surgeon gently feels its tip just deep to the dermis close to hemostat). The blade of the 18-gauge needle is used to cut the band carefully without cutting the skin open.
The cut is considered successful when the arch of the band flattens. The cutting needle is felt just deep to the dermis along the distance between the inlet and exit point of the transfixing needle, loss of upward then downward motion of the transfixing needle when the platysma contracts and relaxes, and finally a defect in the band will appear when platysma actively contracts (Fig. 2g, h). Bleeding (if overt) is controlled by pinching compression for a few minutes. The previous steps are repeated for all the marked platysmal bands (a cut every 2 cm). For the medial bands, cuts are done from the level of the hyoid bone to the suprasternal notch. For the lateral bands, cuts are done only in the level overlie the lower two thirds of sternomastoid muscle to avoid the danger zones of the great auricular nerve, the facial nerve branches and the external jugular vein.
Postoperative Care and Follow-Up
The skin is cleaned by antiseptic solution and painted with antibiotic cream and light dressings were applied. Patients were asked to remove the dressing the next day and to apply antibiotic cream three to four times daily for 5 days. No systemic antibiotics were needed, and paracetamol tablets were prescribed as an analgesic. Patients were advised to use warm fomentations as much as possible from the next day to help clearance of anticipated bruising (Fig. 3).
Patients were asked to come for follow-up the next day (Fig. 3), after a week, then after a month, then every 3 months before final photography is taken 1 year postoperative. In the last visit, the patients were photographed and asked to rate the results of the procedure according to their opinion after assessment of their photography giving one mark regarding a positive opinion in these questions about:
-
1.
Band disappearance.
-
2.
Any residual scarring.
-
3.
Valuable improvement of the cervicomental angle.
The subjective opinions were summarized according to total marks as follow:
-
Poor = 0.
-
Fair = total 1 marks.
-
Very good = total 2 marks.
-
Excellent = total 3 marks.
The pre- and postoperative photography were assessed by an independent observer (other plastic surgeon) for an objective opinion using the same questionnaire.
The collected data of the degrees of satisfaction of both patient and objective opinion were used to measure patient/objective assessment agreement by Kappa statistical analysis (no agreement K = 0, slight agreement K = less than 0.2, fair agreement K = 0.21–0.4, moderate agreement K = 0.4 to 0.6, substantial agreement K = 0.6–0.8 and perfect agreement K = 0.8–1) [16].
Results
Twenty-five female patients shared in this study. The age of our patients ranged from 32 to 55 years. All of our patients had disfiguring platysmal bands and some degree of poor definition of the cervicomental angle. Our patients were non-surgical patients according to the Rohrich et al. suggested algorithm [1]. Twenty-two of our patients did not have any neck surgery before and three of them developed these bands after liposuction to the submandibular area done by other surgeons.
Platysmotomy was done in this study as an office procedure without hospital admission and under local anesthesia only with observed good tolerability from all patients
We did not have any major neurovascular injury in our cases, bleeding after cutting the bands was properly controlled by digital compression for a few minutes by the index and thumb.
We had temporary neck bruises in 80% of our cases (Fig. 3) all resolved spontaneously within 2 weeks. The edematous cut edge of the bands persisted in patients (4 patients) with thicker bands but finally disappeared within 3 weeks. We had a single patient who needed 2 additional cuts to a resistant band (done once bruising was resolved); otherwise, no recurrences were detected in 1 year follow-up and one patient followed up for 18 months (Fig. 5). No patient had any kind of visible scars in this series. Twenty-three patients rated the results excellent, while two rated results very good without any negative ratings. The Kappa analysis [16] showed that the agreement between patients’ opinions and objective opinions was perfect as regard to results (K = 0.842). A sample of our results is shown in Figs. 4, 5, 6, 7 (4 cases).
Clinical photographs of 53-year-old woman complaining of neck bands which appear involuntarily a–f preoperative views. g–l Postoperative views after 1 year. f Preoperative photograph of platysmal band s when platysma is in action. l One-year postoperative photograph of platysmal bands when platysma is in action
Clinical photographs of 50-year-old woman complaining of neck band that appears involuntarily and asking for better definition of the lower jaw. a–g Preoperative views. g Preoperative markings. h–m Postoperative views after 1 year. n–r Postoperative views after 1.5 years. f Preoperative photograph of platysmal bands when platysma is in action. m One-year postoperative photograph of platysmal bands when platysma is in action. r One and one-half year postoperative photograph of platysmal bands when platysma is in action
a–f Preoperative photographs of 45-year-old woman mainly complaining of neck bands after liposuction of the submental area by another surgeon 1 year before. f Preoperative markings. g–l Postoperative views after 1 year. e Preoperative photograph of platysmal bands when platysma is in action. l One-year postoperative photograph of platysmal bands when platysma is in action
Clinical photographs of 48-year-old woman complaining of poor cervicomental angle and neck bands which appear involuntarily. a–g Preoperative views. g Preoperative markings. h–m Postoperative views after 1 year e, f Preoperative photographs of platysmal bands when platysma is in action. l, m One-year postoperative photographs of platysmal bands when platysma is in action
Discussion
The treatment of platysma bands is a constant challenge for surgeons performing rejuvenation surgeries in the cervical region [7]. The correction of platysma bands, whether as an isolated procedure or in association with face-lifting, has received innumerable surgical refinements over recent decades including isolated or combined procedures to the skin, the platysma, the superficial musculoaponeurotic system (SMAS), and adipose deposits when present. Famous examples of these procedures includes skin-platysma muscle anchoring by Fogli, vest-over-pants platysmarrhaphy by Gyron et al., and corset platysmaplasty by Fledman [1, 3, 5, 7, 8, 17,18,19]. Despite the variety of surgical techniques, there is a significant group of patients who can be managed non-surgically or using much less invasive surgical methods. The latter group was the target of this work.
The 25 patients who shared in this work had no excess fat in the submental area (22 patients) or had their excess fat removed by liposuction done by other surgeons (3 patients). Daher [7] operated on 11 patients with 3 patients undergoing closed platysmotomy combined with face lift, while Gonzales gave no data about the number of his patients and if he used isolated closed platysmotomy or combined [8]. We believe that to adequately assess a technique, it should be studied isolated with a standardized inclusion criteria for patients. In our study, we focused on patients who were young to middle aged and with isolated platysmal bands previously classified for non-surgical treatment by Rohrich et al. [1]. Having some patients with platysmal bands that appeared after neck liposuction proving the value of the recommendation to properly assess platysma before liposuction of the neck as liposuction only may expose hidden platysmal bands [1, 3].
We did not have scar-related complains or even scars in this study. There is a risk of scarring when using stainless steel wires and threads to saw the bands as the skin ports usually widen [7]. Using mini-incisions [6] will have even a higher risk of undesired scarring as scars in the neck are not easy to hide.
Regarding the raw material costs, the cost of our technique is negligible if compared to using a special device [7], special stainless steel wires [5] or even Vicryl® surgical thread [8]. Regarding the fact that treatment of platysmal bands by botulinum toxin is expensive due to the relatively large doses needed [4] also adding the fact that treatment has to be repeated every few months, one can safely conclude that on the long-term botulinum toxin treatment is the most expensive treatment option [4].
It is worth mentioning that botulinum toxin treatment is not an absolutely safe treatment. There are reported platysma botulinum toxin injection-specific complications like dysphagia and dysarthria due to the spread of the toxin to deeper neck muscles [4].
In this work, cutting of any visible platysmal band was done below the hyoid level to the suprasternal notch for most medial bands and below the danger zone for marginal mandibular and cervical facial nerve branches and the great auricular nerve, other series only focused on medial bands. We believe that our attitude gives a better cervicomental angle due to a compensatory increase in platysmal muscle tone in its part above the hyoid. This statement is supported by the fact that putting a part of any muscle out of action, e.g., by botulinum toxin will stimulate a compensatory increase in the tone of other parts of the same muscle [4] also, the cuts along the most medial bands lengthen the medial edge of the muscle allowing better draping of the platysma and skin over the deeper structures.
We consider that platysmotomy in general is cosmetically safe as it is well known that the lower part of the platysma is completely cut in other surgeries, e.g., thyroidectomy with no reported negative impact on the support of the submental and submandibular area.
The safety of our technique regarding major neurovascular structures at risk in the neck was achieved by respecting the danger zones of these nerves and vessels and their surface anatomy. The danger zone of the cervical and mandibular branches was proposed between two lines parallel to the lower border of the mandible; one line above it by 1 cm and the other below it by 2 cm below it. Both lines extend forward from the level of the angle of the mandible to a vertical level in line with the premolar teeth nearly at the level of the commissure of the mouth [11,12,13]. The danger zone of the great auricular nerve branches was proposed in a triangle of which the apex is at the lower external auditory meatus, its base at the level between the upper third and lower two-thirds of the sternomastoid muscle, its front limb being vertical to a Frankfort horizontal line extending downward, and its hind limb forms a 30º angle with the front limb at the apex while the nerve itself is represented by a line over the upper third of the anterior border of sternomastoid muscle [14, 15].
The external jugular vein is about 0.5 cm in front of the great auricular nerve trunk. However, in thin necks of this group of patients, any superficial vein in these thin necks whether the external jugular vein, anterior jugular vein, or even unnamed venous tributaries are usually easy to see.
Safety of neurovascular structures was furthermore enhanced by keeping just close to the bands while cutting, having the artery forceps fixed needle as a deep limit of cutting.
The combination of low cost, effectiveness, outpatient nature, safety and self-limiting minor complications along with ease to manage recurrent cases explains the high patient satisfaction rate and the perfect (patients/objective assessment) agreement on Kappa analysis [16] we had in this series.
The need for a cooperative conscious patient is essential to control these active bands by our method and gives more esthetic outcomes in our opinion but limits its use if the patient is under anesthesia if platysmotomy is planned in combination with other surgeries under general anesthesia, e.g., face lift.
Conclusion
Regarding the results of our work, we can conclude that with proper patient selection, the percutaneous needle closed platysmotomy is a valuable technique in management of platysmal bands as an office procedure.
Recommendations
The status of the platysma should be assessed before liposuction of excess submental fat. If platysmal bands are detected, a management plan for them should be added.
References
Rohrich RJ, RiosJL Smith PD, Gutowski KA (2006) Neck rejuvenation revisited. PlastReconstrSurg 118(5):1251–1263
Watson D (2005) Submentoplasty. Facial PlastSurgClin North Am 13(3):459–467
Dayan SH, Benjamin B, Rayan MG, Amit BP (2009) Ch.6: Neck rejuvenation. In: Hirsch R, Sadick N, Cohen JL (eds) Aesthetic rejuvenation a regional approach. McGraw Hill Medical, pp 123–149
De Maio M, Rzany B (2007) Chap. 5: The most common indications. In: De Maio M, Rzany B (eds) Botulinum toxin in aesthetic medicine. Springer Verlag, Berlin Heidelberg, pp 27–92
Sulamanidze MA, Salti G, Mascetti M, Sulamanidze GM (2000) Wire scalpel for surgical correction of soft tissue contour defects by subcutaneous dissection. DermatolSurg 26(2):146–150
Saylan Z (2001) Serial notching of the platysmal bands. AesthetSurg J 21(5):412–417
Daher C (2011) Closed platysmotomy: a new procedure for the treatment of platysma bands without skin dissection. Aesthetic PlastSurg 35(5):866–877
Gonzalez R (2013) Closed platysmotomy: a new procedure to treat platysmal bands. Aesthetic PlastSurg 37(3):636–637
De Castro CC (1980) The anatomy of the platysma muscle. PlastReconstrSurg 5:680–683
Vistnes LM, Souther SG (1983) The platysma muscle: anatomic considerations for aesthetic surgery of the anterior neck. Clin Plast Surg 10(3):441–448
Davies JC, Agur AMR, Fattah AY (2013) Anatomic landmarks for localization of the branches of the facial nerve. OA Anatomy 1(4):33
Owsley JQ, Argwal CA (2008) Safely navigating around facial nerve in three dimensions. Clin Plast Surg 35(4):467–477
Roostaeian J, Rohrich RM, Stuzin JM (2015) Anatomical considerations to prevent facial nerve injury. Plast Reconstr Surg 135(5):1318–1327
Ozturk CN, Ozturk C, Huettner F, Drake RL, Zins JE (2014) A fail safe method to avoid injury to the great auricular nerve. Aesthet Surg J 34(1):16–21
Lefkowitz T, Hazani R, Chowdhry S, Elston J, Yaremchuk MJ, Wilhelmi BJ (2013) Anatomical landmarks to avoid injury to the great auricular nerve during rhytidectomy. Aesthet Surg J 33(1):19–23
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37:360–363
Fogli AL (2008) Skin and platysma muscle anchoring. Aesthetic Plast Surg 32(3):531–541
Guyron B, Sadek EY, Ahmadian R (2010) A 26-Year experience with vest-over-pants technique platysmarrhaphy. Plast Reconstr Surg 126(3):1027–1034
Fledman JJ (2014) Neck lift my way: an update. Plast Reconstr Surg 134(6):1173–1183
Acknowledgements
The authors would like to acknowledge the efforts of professor Dr. Ashraf Abdel Kader Ahmed Aly (plastic and Reconstructive Surgery Department, Al Azhar University, Cairo, Egypt) for giving his valuable objective opinion in the assessment of the results of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose. There were no conflict of interests of any kind stated by the International Committee of Medical Journal Editors Regulations.
Ethical commitments
All the procedures performed in this study that involved human participants were in accordance of the institutional, national research committee and compliant with the 1964 Declaration of Helsinki and its later amendments and comparable ethical standards. Informed consent was obtained from all individual participants in this study including scientific publications of their clinical photography, videos, etc.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (MOV 60272 kb)
Supplementary material 2 (MP4 313069 kb)
Rights and permissions
About this article
Cite this article
Hegazy, A.M., Farouk, M. A Simplified Method for Management of Platysmal Bands: Platysmotomy as an Office Procedure. Aesth Plast Surg 41, 1351–1359 (2017). https://doi.org/10.1007/s00266-017-0934-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-017-0934-8