Abstract
Background
Mandibular angle ostectomy (MAO) is commonly used to correct prominent mandibular angles through an intraoral approach. However, limited vision in the operative site may lead to difficulties or complications during surgery. Therefore, it is necessary to develop an effective method for helping surgeons to perform MAO more precisely and safely.
Methods
In this study, we report a novel method of a computer image-guided surgical template for navigation of MAO, and evaluate its accuracy and clinical outcomes. Nine patients with a prominent mandibular angle were enrolled in this study. A pair of stereolithographic templates was fabricated by computer-aided image design and 3D printing. In all cases, bilateral MAO was performed under the guide of these templates. Post-operative effects were evaluated by 3D curve functions and maximal shell-to-shell deviations.
Results
All patients were satisfied with their cosmetic outcomes. The mean and SD of ICC between R-Sim and R-Post were 0.958 ± 0.011; between L-Sim and L-Post, 0.965 ± 0.014; and between R-Post and L-Post, 0.964 ± 0.013. The maximal shell-to-shell deviations between the simulated mandibular contour and post-operative mandibular contour on the right and left sides were 2.02 ± 0.32 and 1.97 ± 0.41 mm, respectively.
Conclusion
The results of this study suggest that this new technique could assist surgeons in making better pre-surgical plans and ensure more accurate and safer manipulation for completion of this procedure.
Level of Evidence V
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
In the Orient, women with a prominent mandibular angle are regarded as unattractive, whereas in Westerners this condition is seldom regarded as requiring treatment [1, 2]. Mandibular angle ostectomy (MAO) through an intraoral approach has many advantages, such as the absence of visible scars and much less risk of facial nerve injury. However, limited vision in the operative site may lead to complications or unfavorable results, including condylar fracture, inferior alveolar nerve injury, overcorrection/undercorrection, facial asymmetry, and formation of a second mandibular angle [3–5]. Most plastic surgeons perform the MAO according to their own clinical experience. However, it is not easy to resect a prominent mandibular angle precisely based on pre-surgical planning.
With the development of computer-aided design and rapid prototyping (3D-Print) technology, computer-aided surgical simulation and virtual templates/splints have gained increasing prevalence in today’s maxillofacial surgery [6–8]. For mandibular angle ostectomy, plastic surgeons may also need an effective way of transferring pre-surgical planning from computer-assisted design to the actual operation. In this study, we report a novel method whereby a computer-generated surgical template is used for guiding MAO, and also evaluate its accuracy and clinical outcomes.
Patients and Methods
From July of 2013 to February of 2014, nine patients with prominent mandibular angles were enrolled in this study. The patients included eight women and one man ranging from 20 to 33 years old, with an average age of 26 years. All patients underwent MAO. In three patients, MAO was combined with genioplasty, and in one patient, MAO was combined with reduction malarplasty. This study was approved by the local IRB and all participants signed an informed consent agreement.
Step 1: Obtain the 3D Models
All patients received pre-surgical CT scans. The scanning data were exported as digital imaging and communication in medicine (DICOM) format files and were imported into Mimics software (version 10.01; Materialise, Leuven, Belgium) for segmentation. 3D models of jaws, including inferior alveolar nerves and facial soft tissues, were exported in STL format and imported into Freeform software (version 12.0; Geomagic, Morrisville, NC, USA) for surgical simulation and template design.
Step 2: Surgical Simulation and Template Creation
The 3D models of mandibles and facial soft tissues were set as 70 % and 10 % transparent, respectively, which showed the inferior alveolar nerve and jaws clearly.
The osteotomy line of the MAO was planned according to the following criteria (Fig. 1):
Determination of the osteotomy line of MAO by computer-aided design. The new gonion (Go′) should be located in the red region and on the angle bisector of the MP–RP simultaneously. The green region indicates the bone to be removed from the mandible. FHP Frankfurt horizontal plane, RP ramus plane, MP mandibular plane, Go original gonion, Go′ new gonion
-
(1)
The new gonion (Go′) should be 2.5 ± 0.5 cm below the auricular lobule; it would be located in the normal range of the mandibular plane (MP) angle (FH–MP = 31.1° ± 5.6°) and should be on the angle bisecting the MP–RP (ramus plane).
-
(2)
The planned osteotomy line should be below the mandibular canal, the posterior end of this line should not be higher than the occlusion plane, and its anterior end might reach the mental region. Thus, a natural and smooth curved osteotomy line would be determined.
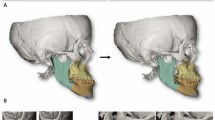
The mandibular angle on one side was removed in the software according to the osteotomy line. The osteotomy line on the other side was marked in reference to the mirror image of the cut side, with the facial midline as the axis of symmetry. Then, 2.5-mm-thick templates were formed on the surface of the resected mandibular angle on both sides. To position the guides on the mandibular angle accurately and prevent slippage during surgery, the template was somewhat extended to the lingual surface of the ramus and inferior border, which formed a “hook” for mechanical fixation of the template (Fig. 2). A pair of stereolithographic templates and mandibular model was fabricated by rapid prototyping. The components of the template were polypropylene (Fig. 3). The templates were immersed in povidone-iodine solution for 45 min before the surgery.
Step 3: Surgical Procedures
Through an intraoral approach, bilateral MAO was performed by routine methods. The masseter was then stripped from the mandibular ramus to the body, and the inferior border was freed from the attached muscle [2]. After exposure of the mandibular angle, the surgical templates were positioned on the outer surface of the mandibular angle (Fig. 4). Ostectomy with an oscillating or reciprocating saw was easily performed along the upper edge of the surgical template (Fig. 4).
Step 4: Post-operative Evaluation
All patients received CT scans post-surgery. Three-dimensional curve functions [z = f(x, y)] regarding simulated mandibular margins of each case were obtained through curve-fitting with Sigmaplot software (version 12.0, Systat Software, Chicago, IL, USA). The post-operative three-dimensional coordinate values (x, y, z) regarding mandibular margins were obtained in Freeform software. We chose at least ten points on the mandibular margins of one side in the lateral view. The goodness of fit between simulation and post-operation was then calculated through the intraclass correlation coefficient (ICC) via SPSS 17.0 (SPSS, Chicago, IL, USA).
For the analysis of post-operative symmetry, the three-dimensional values (x, y, z) from the left side were fitted against three-dimensional curve functions [z = f(x, y)] obtained from the right side.
The post-operative image of the mandible was overlapped with the simulation model, and the maximal shell-to-shell deviations between the simulated mandibular angle and post-operative mandibular angle were calculated on both sides, shown by color-mapping methods [9] (Fig. 5).
Results
The mean and SD of ICC between the right simulated mandibular angle (R-Sim) and the right post-operative mandibular angle (R-Post) was 0.958 ± 0.011. The mean and SD of ICC between the left simulated mandibular angle (L-Sim) and the left post-operative mandibular angle (L-Post) was 0.965 ± 0.014. The mean and SD of ICC between the right post-operative mandibular angle (R-Post) and the left post-operative mandibular angle (L-Post) was 0.964 ± 0.013. The maximal shell-to-shell deviations between the simulated mandibular angle and post-operative mandibular angle on the right and left sides were 2.02 ± 0.32 mm and 1.97 ± 0.41 mm, respectively (Table 1).
The outline of the excised mandibular angle was almost the same as that of the templates (Fig. 6). No patients showed signs of injury to the inferior alveolar nerve, and all were satisfied with their facial contour and cosmetic outcomes (Figs. 7, 8).
Discussion
Differences in cultural backgrounds and esthetic views exist between Orientals and Westerners. Oriental women prefer an ovoid and slender facial contour, which is thought to be a feminine feature. Since Adams [10] (1949) first reported a linear osteotomy for the treatment of prominent mandibular angles, many authors have improved or modified the operative techniques for better correction [11–14]. However, it is not easy to perform these surgical procedures precisely, according to the pre-surgical plan. Because of limitations to the visibility of the intraoral site, locating the osteotomy line during surgery often depends on the surgeons’ experience, and overcorrection, undercorrection, or even facial asymmetry may occasionally occur due to the lack of guidance during the performance of surgery. The development of computer and 3D-print technology provides a possible solution to this problem.
In the current study, we designed osteotomy lines and fabricated surgical templates based on 3D-reconstructed images of the patients’ lower jaw. We performed surgical simulations on these images and designed optimal osteotomy lines in terms of the desired esthetics. Subsequently, we fabricated a surgical template based on the planned osteotomy lines through rapid prototyping (3D-Print). By means of these surgical templates, the surgeon can easily determine the cut line at the surgical site and perform MAO with precision. Our results showed that the ICCs between simulated and post-operative mandibular angles were almost consistent on both sides, and that the maximal shell-to-shell deviations between simulated and post-operative mandibular angles were acceptable, indicating that, with the templates, it can be guaranteed that ostectomy will be performed well along the pre-determined osteotomy line. Moreover, the mandibular canal can be visualized in 3D images of the patient before surgery, which is helpful in the design of an osteotomy line that avoids injury to the inferior alveolar nerve.
From a lateral view, the gonion (the lowest and the most lateral point of the mandibular angle) and the mandibular lower border play important roles in facial contour. If the mandibular angle is resected by straight-line cutting, the natural contour of the lower jaw may be destroyed. An ideal surgical correction allows the gonion to move upward and forward while maintaining the normal shape of the angle. Although “V-line” ostectomy can change the incline of the mandibular plane, it leads to a posterior displacement of the gonion [15]. In this study, we have established a new method to determine the new gonion by computer-aided design. According to the normal position of the gonion and normal value of the mandibular plane angle, a new gonion can be found easily. Moreover, it is necessary to expand the osteotomy line to the mental region, which can avoid the formation of “a secondary mandibular angle”. Using this method, we can design a well-curved osteotomy line and obtain a natural and smooth mandibular profile.
In the frontal view, symmetry is another important esthetic criterion following MAO. On one hand, the surgeon must remove the prominent mandibular angle on both sides equally to guarantee facial symmetry. On the other hand, some patients have asymmetric prominent mandibular angles before surgery, so the angles must be resected differently on both sides of the mandible to achieve new facial symmetry. Initially, we designed the osteotomy line on one side and removed the excised bone. We then designed a new cutting line on the other side by reference to the mirror image on the contralateral mandible. This method may guarantee the symmetry of bilateral mandibular angles. Our results revealed that the ICC between left and right mandibular angles was 0.964 ± 0.013, indicating good symmetry of the lower jaw following MAO.
Digital technology is often used in plastic and esthetic surgery for better correction. We believe that this technique may also provide a visual method for patients to easily understand the operation, and an effective way for training young plastic surgeons.
Conclusions
By means of computer and 3D-print technology, we have developed a novel method for better design of MAO and prepared a surgical template to guide the performance of this surgical procedure. This digital technique can not only assist surgeons in optimal pre-surgical planning but also help MAO to be performed more precisely and safely.
References
Liu D, Huang J, Shan L, Wang J (2011) Intraoral curved ostectomy for prominent mandibular angle by grinding, contiguous drilling, and chiseling. J Craniofac Surg 22:2109–2113
Satoh K (1998) Mandibular contouring surgery by angular contouring combined with genioplasty in orientals. Plast Reconstr Surg 101:461–472
Oh YW, Han KT, Ahn ST (1990) The complication of mandibular angle reduction. J Korean Soc Plast Reconstr Surg 17:645–652
Hwang K, Han JY, Kil MS, Lee SI (2002) Treatment of condyle fracture caused by mandibular angle ostectomy. J Craniofac Surg 13:709–712
Kane AA, Lo LJ, Chen YR, Hsu KH, Noordhoff MS (2000) The course of the inferior alveolar nerve in the normal human mandibular ramus and in patients presenting for cosmetic reduction of the mandibular angles. Plast Reconstr Surg 106:1162–1174; discussion 1175–1166
Zinser MJ, Mischkowski RA, Sailer HF, Zoller JE (2012) Computer-assisted orthognathic surgery: feasibility study using multiple CAD/CAM surgical splints. Oral Surg Oral Med Oral Pathol Oral Radiol 113:673–687
Choi JY, Song KG, Baek SH (2009) Virtual model surgery and wafer fabrication for orthognathic surgery. Int J Oral Maxillofac Surg 38:1306–1310
Xia J, Ip HH, Samman N, Wang D, Kot CS, Yeung RW, Tideman H (2000) Computer-assisted three-dimensional surgical planning and simulation: 3D virtual osteotomy. Int J Oral Maxillofac Surg 29:11–17
Ye N, Long H, Xue J, Wang S, Yang X, Lai W (2014) Integration accuracy of laser-scanned dental models into maxillofacial cone beam computed tomography images of different voxel sizes with different segmentation threshold settings. Oral Surg Oral Med Oral Pathol Oral Radiol 117:780–786
Adams WM (1949) Bilateral hypertrophy of the masseter muscle; an operation for correction; case report. Br J Plast Surg 2:78–81
Gui L, Yu D, Zhang Z, Changsheng LV, Tang X, Zheng Z (2005) Intraoral one-stage curved osteotomy for the prominent mandibular angle: a clinical study of 407 cases. Aesthet Plast Surg 29:552–557
Kim Y, Park B (2003) Resection of the prominent mandible angle with intraoral and external approach. Aesthetic Plast Surg 27:38–42; discussion 43
Yang DB, Park CG (1991) Mandibular contouring surgery for purely aesthetic reasons. Aesthet Plast Surg 15:53–60
Ying B, Wu S, Yan S, Hu J (2011) Intraoral multistage mandibular angle ostectomy: 10 years’ experience in mandibular contouring in Asians. J Craniofac Surg 22:230–232
Hsu YC, Li J, Hu J, Luo E, Hsu MS, Zhu S (2010) Correction of square jaw with low angles using mandibular “V-line” ostectomy combined with outer cortex ostectomy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:197–202
Acknowledgments
This work was supported by a Grant from Foundation of Ministry of Education of China (No. 20130181130004). We also thank 3D Orthodontics & Craniofacial Laboratory, Shanghai TiTOK Medical Technology Co., Ltd.
Conflicts of interest
The authors declare that they have no conflicts of interest to disclose.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ye, N., Long, H., Zhu, S. et al. The Accuracy of Computer Image-Guided Template for Mandibular Angle Ostectomy. Aesth Plast Surg 39, 117–123 (2015). https://doi.org/10.1007/s00266-014-0424-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-014-0424-1