Abstract
Background
Studies have shown the laparoscopically harvested omental flap to be a successful method for immediate breast reconstruction. However, data about its usefulness and safety in obese women are limited. This study examined the effectiveness and safety of a pedicled omental flap delivered via a minilaparotomy in women with a body mass index (BMI) higher than 30 kg/m2.
Methods
Women candidates for skin-sparing mastectomy underwent reconstruction with delivery of a pedicled omental flap via a minilaparotomy.
Results
Surgery was performed for 24 women with a mean age of 57.54 years and a mean BMI of 32.54 kg/m2. The operative time was prolonged by about 1 h without excess blood loss or prolongation of their hospital stay. Except for a single case of partial flap necrosis, no single total flap loss was recorded. In three patients (12.5 %), the flap volume was inadequate, and silicone implant was used as an adjunct. Only one patient (4 %) experienced a small incisional hernia. The majority of the patients (67 %) described their cosmetic outcome as excellent.
Conclusion
Delivery of a pedicled omental flap via a minilaparotomy is a safe and reliable method for immediate breast reconstruction after skin-sparing mastectomy in women with a BMI higher than 30 kg/m2.
Level of Evidence V
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Restoration of breast appearance after mastectomy was found to improve patient psychology without affecting overall survival [1, 2]. Studies have shown that immediate breast reconstruction is superior to delayed reconstruction both aesthetically and functionally [3]. The emergence of skin-sparing mastectomy has enabled immediate breast reconstruction and better matching with the normal breast without increasing complications or local recurrence [4, 5].
Immediate breast reconstruction can be achieved effectively with either prosthetic or autologous tissue reconstruction. Pure autologous tissue reconstruction is more desirable because of its durability, better appearance, softness, warmth, ptosis, avoidance of implant-related complications, and resistance to the effect of postoperative irradiation [6, 7].
The latissimus dorsi, an autologous flap, is relatively easy to harvest with a reliable blood supply [8]. However, it may undergo muscle atrophy with subsequent bulk reduction, and its use for a large breast mandates adjunct implant placement [6].
The pedicled and free transverse rectus abdominis muscle (TRAM) and deep inferior epigastric perforator flaps are autologous flaps that can give more bulk, but in many obese and relatively older patients, these are at risk for partial or total loss [9, 10]. In addition to the technical demands, especially in the case of free flaps, both latissimus and TRAM flaps may put the patient at risk for blood transfusion and donor-site morbidity [6]. Of course, all these flaps are still the gold standard, especially when skin-sparing mastectomy cannot be achieved and skin coverage is required. However, in the case of obese women, a delayed procedure may be advised when use of the pedicled TRAM is planned to minimize flap loss [10].
The use of the omental flap for breast cancer was first described by Kiricuta [11] in 1963. More than a decade later, Arnold et al. [12] described a one-stage reconstruction of the breast using a transposed greater omentum.
Saltz et al. [13] were the first to describe the laparoscopic harvest of the omental flap for repair of soft tissue defects in the knee in 1993. A few years later, Costa et al. [14, 15] described the laparoscopically harvested omental flap for breast reconstruction and its use in the treatment of Poland syndrome.
Because the omentum has no skin cover, it is best used with skin-sparing mastectomy. The omental flap has several advantages over the other autologous tissues, namely, its simplicity, safety, reliability, and contour preservation [12, 16]. In the case of laparoscopic harvesting, if the omentum is bulky, it cannot be delivered through a small epigastric incision. Moreover, vascular injury may occur [17]. These difficulties may be more frequent among patients with a body mass index (BMI) higher than 30 kg/m2 [17].
The current study aimed to evaluate the safety and efficacy of the pedicled omental flap delivered via a minilaparotomy for immediate breast reconstruction after skin-sparing and nipple-areola-sparing mastectomy in women with a BMI higher than 30 kg/m2.
Methods
A prospective study was conducted with 24 women between December 2009 and December 2012. All women who were candidates to undergo skin-sparing and nipple-areola-sparing mastectomy for breast cancer were asked to join the study. Written informed consents were obtained from all the patients before their enrollment. The study excluded locally advanced cases, candidates for breast conservation, women with a history of omental resection as in gastrectomy and ovarian cancer, and those with evidence of extensive adhesions in the upper abdomen.
All the eligible patients underwent mastectomy with immediate breast reconstruction using a pedicled omental flap delivered via a minilaparotomy (~7 cm long). Silicone implants of different sizes were available to be placed under the omentum in case of insufficient flap volume. The aforementioned technique was intentionally performed for patients with a BMI higher than 30 kg/m2, whereas those with a lower BMI were offered different reconstructive methods.
The mastectomy was started so as not to expose the abdomen for a long time with a subsequent increase in wound sepsis and to ensure that the mastectomy was performed safely. Next, an upper midline minilaparotomy incision was made for exploration of the abdomen. The omentum then was dissected from the transverse colon.
In all the patients, the right gastroepiploic artery was used as the main vascular pedicle, with division of the left one (Fig. 1). Finally, the omentum was detached from the greater curve of the stomach to be ready for transfer to the mastectomy bed after creation of a tunnel (Fig. 1). The abdominal wound then was closed by mass closure using a suitable nylon loop and leaving a space only for the flap pedicle, whereas the omentum was sutured by a few stitches of Vicryl 2/0 to the pectoral muscle medially.
A case of previously excised mass treated by nipple-sparing mastectomy and pedicled omental flap reconstruction. a Preoperative view showing the scar of the excisional surgery. b Operative bed after mastectomy. c Extraction of the omentum via a minilaparotomy with clamping of the left gastroepiploic vessels. d Delivery of the omentum to the bed through the tunnel. e Front view eight months post-operatively showing the size gain phenomenon and excellent ptosis. f Side view of the same patient
In case of insufficient flap volume, a textured silicone implant (Mentor, Santa Barbara, CA) of suitable volume was wrapped by the omentum, which was sutured over it, making a pocket for the implant. The nipple and areola in the majority of the patients (17/24, 71 %) were free of tumor (by frozen section) and preserved. Skin-sparing mastectomy with free grafting from the contralateral nipple and areola was performed for the remaining patients (7/24, 29 %). Two patients refused further procedures and were satisfied with the cosmetic outcome after healing of the areolar wound.
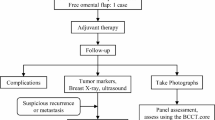
Because a gradual gain in breast size was observed, for relatively small breasts after reconstruction, we decided to wait for about 6 months to assess the final size of the reconstructed breast (Fig. 2). During the follow-up period, we used both subjective and objective methods to assess the aesthetic outcome, allowing a minimum of 6 months for evaluation of the final outcome.
Patient with relatively small volume of the omentum who refused further implant placement. a Intraoperative volume of the omentum. b View 2 months after the operation. c Mammographic view of the reconstructed left breast six months postoperatively. d Postoperative front view with noticeable flap size gain 8 months after the operation
Results
Table 1 shows the demographic characteristics of the studied patients. During the study period, 24 patients underwent mastectomy with immediate breast reconstruction using a pedicled omental flap delivered via a minilaparotomy. The mean age of the women was 57.54 years (range 52–62 years), and their mean BMI was 32.54 kg/m2 (range 31–34 kg/m2). The median follow-up period was 28 months (range 10–36 months). Six patients (25 %) reported a history of lower abdominal operations. Five patients (21 %) had undergone Cesarean section, and one patient (4 %) had undergone an appendectomy.
Table 2 shows the operative characteristics and postoperative outcomes. As shown, 17 patients (71 %) underwent nipple-areola-sparing mastectomy, and 7 patients (29 %) underwent skin-sparing mastectomy. At abdominal exploration, the omental size was insufficient in three patients (13 %), so an implant was used for volume replacement and covered by the omentum.
The mean operative time was 177.92 min (range 160–210 min), and the mean harvest time was 61.5 min (range 50–75 min). The mean blood loss was 170.42 ml (range 80–300 ml), with negligible blood loss during flap retrieval. The mean hospital stay was 3.8 days (range 3–5 days). The flap survival was excellent, with only one case of partial flap loss (4 %).
A single patient (4 %) presented with a small uncomplicated incisional hernia affecting the upper part of the epigastric incision, which was diagnosed during routine follow-up. She was a 59-year-old diabetic patient receiving oral hypoglycemic treatment, and the hernia was managed conservatively.
Mild controllable breast wound hematoma was observed in two patients (8 %). Abdominal wound sepsis was diagnosed in two additional patients (8 %), both of whom were diabetics, and the sepsis was controlled medically. Six patients (25 %) received postoperative radiotherapy without significant changes in the breast contour. These cases were followed up at 2-month intervals for radiation-induced mastitis or contour changes. Five patients (21 %) experienced minor breast deformities that did not affect their outcomes.
The majority of the patients (16/24; 67 %) were highly satisfied with their reconstructed breasts. The remaining patients described their satisfaction as either good (8 %) or fair (25 %).
Discussion
To our knowledge, this is the first study to investigate use of the pedicled omental flap intentionally as a sole breast substitute after mastectomy for patients with a BMI higher than 30 kg/m2. Additionally, the omental flap can be used for immediate breast reconstruction together with an implant when the flap is used to cover it. Several advantages of the omental flap have been described including its easy malleability, adequate vascular reliability, high absorptive power with a size-increase phenomenon unlike any other flap, additional immune function that may protect against infection after reconstruction, simple retrieval with no need for a long learning curve, and minimal donor-site trauma that can reduce donor-site morbidity [18].
In 2010, Zaha and Inamine [17] published a large study examining laparoscopically harvested omental flaps among 96 women. They evaluated a relatively younger group of women (mean age 49 years) with an average BMI (22 kg/m2). In our study, the mean age was 57.5 years, and the mean BMI was 32.5 kg/m2.
Additionally, because Zaha and Inamine [17] excluded obese patients (BMI ≥ 35 kg/m2), they called for further studies to determine whether the omental flap can be safely harvested using laparoscopy in patients with morbid obesity [17]. Moreover, they suggested an appropriate longitudinal incision on the abdominal wall and a free flap for a large omentum or for obese patients [17]. They suggested this because when the omentum is large, it is difficult to withdraw the flap through the small laparotomy incision, and the possibility of vascular injury to the flap increases [17].
In another study, Costa et al. [15] reported an excellent aesthetic outcome using the omental flap in 15 young women (mean age 26 years; range 18–53 years). However, because these patients had Poland syndrome, comparison with the current findings may be irrelevant.
The BMI of the patients in our study did not approach the level of morbid obesity because morbidly obese patients rarely present with breast cancer in our practice. In our study, flap retrieval and fixation prolonged the operative time by about 1 h without any considerable blood loss. The hospital stay in the current study was not longer than the usual stay after mastectomy. Additionally, the flap survival in the current study was excellent, with only a single case of partial necrosis (4 %).
To evaluate the cosmetic outcome, we used both a subjective method depending on patient satisfaction with the reconstructed breast compared with the native one and an objective score as described by Lowery et al. [19]. The majority of our patients were highly satisfied with their reconstructed breast. About two-thirds described their results as excellent, and most of the patients refused further correction of minor deformities.
Several limitations of omental flaps were observed. One of the most important limitations of the omental flap is its frequently unpredictable volume even with preoperative radiology [17]. This limitation may be reversed by the different sizes of silicone implants available at the start of the operation. For patients with volume inadequacy, the implant is wrapped by the omentum as an immediate method of reconstruction.
In our study, volume inadequacy occurred in 3 (13 %) of the 24 patients. Similarly, Zaha et al. [20] in 2006 reported a 12.5 % (5/40) incidence of volume inadequacy among women treated using a laparoscopically harvested omental flap with additional use of a prosthesis. Similar results were obtained from a number of small studies [21, 22].
Another drawback is the volume-gain phenomenon, which may disturb the symmetry. Actually, in most of our patients, the immediate postoperative flap was smaller than the native breast, and with size gain, the symmetry was surprisingly improved. For this reason we waited 6 months to judge the final aesthetic outcome.
Still another possible drawback is the risk of infection associated with abdominal exploration. Actually, we encountered only two cases with mild controllable wound sepsis, and we advise usage of a strong broad-spectrum antibiotic during flap retrieval. Only a single patient (4 %) in the current study experienced the development of a small uncomplicated incisional hernia. This low incidence may have been due to proper patient selection or to the relatively small number of patients.
Nevertheless, the current findings seem to indicate that a minilaparotomy is a quite safe procedure. The current hernia rate closely approximated that reported by Zaha and Inamine [17], who described a 1 % incidence of incisional hernia during laparoscopic retrieval. On the other hand, this rate was much lower than that reported by other researchers. Van Garderen et al. [22] reported hernia in one-fifth (7/35) of the patients who underwent extraabdominal pedicled omentoplasty. Furthermore, Contant et al. [23] reported hernia in one-fourth (9/34) of the patients who underwent a pedicled omental flap for reconstruction of defects in the chest wall.
We can finally conclude that the pedicled omental flap is a safe, easy, and reliable alternative option for breast reconstruction after skin-sparing mastectomy. It is mainly retrieved through a laparoscopic approach, but in cases of large-volume flaps, frequently encountered with obese women, the flap is better extracted via a minilaparotomy.
Conclusion
Despite the relatively small size of this study, the current findings show that delivery of the pedicled omental flap via a minilaparotomy is a safe and reliable method for immediate breast reconstruction after skin-sparing mastectomy in women with a BMI higher than 30 kg/m2 when laparoscopic extraction is difficult.
References
Delgado F, Pedraza MJL, Blasco JA, Aragones EA, Mendez JIS, Miralles GS, Reza MM (2008) Satisfaction with and psychological impact of immediate and deferred breast reconstruction. Ann Oncol 19:1430–1434
Agarwal S, Liu JH, Crisera CA et al (2010) Survival in breast cancer patients undergoing immediate breast reconstruction. Breast J 16:503–509
Elder EE, Brandberg Y, Bjorklund T et al (2005) Quality of life and patient satisfaction in breast cancer patients after immediate breast reconstruction: a prospective study. Breast 14:201
Kroll SS, Khoo A, Singletary SE et al (1999) Local recurrence risk after skin-sparing and conventional mastectomy: a 6-year follow-up. Plast Reconstr Surg 104:421–425
Franco HM, Vasconez LO, Fix RJ, Heslin MJ et al (2002) Factors associated with local recurrence after skin-sparing mastectomy and immediate breast reconstruction for invasive breast cancer. Ann Surg 235:814–819
Jahkola T, Asko-Seljavaara S, Von Smitten K (2003) Immediate breast reconstruction. Scand J Surg 92:249–256
Christensen BO, Overgaard J, Kettner LO, Damsgaard TE (2011) Long-term evaluation of postmastectomy breast reconstruction. Acta Oncol 50:1053–1061
Olivari N (1976) The latissimus flap. Br J Plast Surg 29:126–128
Banic A, Boeckx W, Greulich M, Guelickx P, Marchi A, Rigotti G, Tschopp H (1995) Late results of breast reconstruction with free TRAM flaps: a multicentric study. Plast Reconstr Surg 95:1195–1204
Momoh AO, Colakoglu S, Westvik TS, Curtis MS, Yueh JH, de Blacam C, Tobias AM, Lee BT (2012) Analysis of complications and patient satisfaction in pedicled transverse rectus abdominis myocutaneous and deep inferior epigastric perforator flap breast reconstruction. Ann Plast Surg 69:19–23
Kiricuta I (1963) The use of the great omentum in the surgery of breast cancer. Presse Med 71:5–21
Arnold PG, Hartrampf CR, Jurkiewicz MJ (1976) One-stage reconstruction of the breast using the transposed greater omentum: case report. Plast Reconstr Surg 57:520–522
Saltz R, Stowers R, Smith M, Gadacz TR (1993) Laparoscopically harvested omental free flap to cover a large soft tissue defect. Ann Surg 217:542–546
Costa SS, Pedrini JL, Recamonde A, Penczek F (1998) Tratamento cirúrgico da syndrome de Poland com omento transposto por Videolaparoscopia. Paper presented at the XI Congresso Brasileiro de Mastologia, Foz do Iguaçu-Paraná: XI Congresso Brasileiro de Mastologia, p 186
Costa SS, Blotta RM, Mariano MB et al (2010) Aesthetic improvements in Poland’s syndrome treatment with omentum flap. Aesthetic Plast Surg 34:634–639
Das SK (1976) The size of the human omentum and methods of lengthening it for transplantation. Br J Plast Surg 29:170–174
Zaha H, Inamine S (2010) Laparoscopically harvested omental flap: results for 96 patients. Surg Endosc 24:103–107
Song XY, Guan DD, Lin H, Dai Y, Zheng XY, Zhu YP, Wang XF (2011) Immediate breast reconstruction using laparoscopically harvested omental flap after breast-conserving surgery. Zhonghua Zheng Xing Wai Ke Za Zhi 27:401–405
Lowery JC, Wilkins EG, Kuzon WM (1996) Evaluation of aesthetic results in breast reconstruction: an analysis of reliability. Ann Plast Surg 36:601–607
Zaha H, Inamine S, Naito T, Nomura H (2006) Laparoscopically harvested omental flap for immediate breast reconstruction. Am J Surg 192:556–558
Cothier-Savey I, Tamtawi B, Dohnt F, Raulo Y, Baruch J (2001) Immediate breast reconstruction using a laparoscopically harvested omental flap. Plast Reconstr Surg 107:1156–1163; discussion 1164–1165
Van Garderen, Wiggers TH, Van Geel AN (1991) Complications of the pedicled omentoplasty. Neth J Surg 43:1171–1174
Contant CME, Van Geel AN, Van der Holt B, Wiggers T (1996) The pedicled omentoplasty and split skin graft (POSSG) for reconstruction of large chest wall defect: a validity study of 34 patients. Eur J Surg Oncol 22:532–537
Acknowledgments
We thank Dr. Ayman Elsaed, professor of community medicine, Mansoura University, for his support throughout this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Khater, A. Evaluation of Pedicled Omental Flap Delivered through a Minilaparotomy for Immediate Breast Reconstruction in Obese Patients. Aesth Plast Surg 37, 1140–1145 (2013). https://doi.org/10.1007/s00266-013-0217-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-013-0217-y