Abstract
Background
Keloids and hypertrophic scars are extremely disturbing to patients, both physically and psychologically. This study prospectively assessed the safety and efficacy of intense pulsed light (IPL) on scars originating from burns, trauma, surgery, and acne.
Methods
Hypertrophic scars in 109 patients, originating from surgical incisions (n = 55), traumatic cuts (traffic accidents) (n = 24), acne scars (n = 6), keloids (n = 5), and burns (n = 19), were treated using an IPL® Quantum™ device. Treatment was administered at 2–4-week intervals, and patients received an average of 8 treatments (range = 6–24). Using digital photographs, Changes in scar appearance were assessed by two physicians who were blinded to the study patients and treatments. The photographs were graded on a scale of 0 to 4 (none, minimal, moderate, good, excellent) for improvement in overall clinical appearance and reduction in height, erythema, and hardness.
Results
An overall clinical improvement in the appearance of scars and reductions in height, erythema, and hardness were seen in the majority of the patients (92.5%). Improvement was excellent in 31.2% of the patients, good in 25.7%, moderate in 34%, and minimal in 9.1%. Over half the patients had good or excellent improvement. In the preventive IPL treatment group, 65% had good to excellent improvement in clinical appearance. Patient satisfaction was very high.
Conclusion
This study suggests that IPL is effective not only in improving the appearance of hypertrophic scars and keloids regardless of their origin, but also in reducing the height, redness, and hardness of scars.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The appearance of keloids and hypertrophic scars, whatever their origins (traumatic scarring and/or burn scars), are extremely disturbing to patients, both physically and psychologically, and are challenging for physicians. Hypertrophic scars and keloids occur as a result of excessive healing reactions to damage to the deep skin tissues after traumatic or surgical wounds that have a prolonged phase of inflammation and fibroplasias. This healing reaction leads to excessive fibroblast proliferation and collagen synthesis that result in benign fibrous outgrowths for both keloids and hypertrophic scars. Both have a similar clinical appearance; however, the growth reaction remains within the margins of the scar in hypertrophic scars, while in keloids the reaction has the ability to extend the boundaries of the initial scar and is likely to recur after treatment [1].
Despite increasing knowledge of wound healing and metabolism, hypertrophic scars are difficult to prevent and eradicate. The exact pathogenesis of keloids and hypertrophic scar formation still remains unknown which makes treatment even more complicated [2]. Various treatment options are available, including intralesional and topical corticosteroids, surgery, cryosurgery, laser treatment, silicone gel or sheet application, radiotherapy, application of pressure, intralesional injection of noncorticosteroid agents (e.g., interferon), and 5-fluorouracil [2, 3]. These treatments can achieve flattening in some cases, but complete removal is never obtained. Furthermore, multiple treatments are usually required and adverse effects, including infections, hypoesthesia, necrosis, and loss of pigmentation, may occur [3–6].
Because of the limitations of currently available treatments, other options such as short-pulsed pulsed dye laser (PDL) and long-pulsed pulsed dye laser (LPDL) have been used with reported improvement in the long-term appearance of hypertrophic scars [7–10]. More recently, intense pulsed light (IPL) applied following suture removal was found in a pilot study to be effective on surgically induced scars [11], and on various types of scars in another study [12]. The mechanism of IPL is not fully understood, but it probably targets the vascular proliferation essential to the collagen overgrowth and its effect on the pigmentation (both melanin and artificial pigments) that results in scar development (hyperpigmented, erythematous, and proliferative scars) [11–13].
IPL treatment has been extensively researched and used for photorejuvenation [13], sun-damaged skin, and pigmented lesions [11–16], but there are few studies of its effects on hypertrophic scars [12, 17, 18]. This study prospectively assessed the safety and efficacy of IPL on scars originating from burns, trauma, surgery, and acne. A secondary goal was to determine the role of IPL in the prevention of hypertrophic scarring after surgery.
Materials and Methods
The efficacy of IPL was assessed in 109 adult patients who underwent IPL treatment (IPL® Quantum™, Lumenis Inc., Santa Clara, CA) for hypertrophic scars or keloids between November 2003 and July 2006. In most cases hypertrophic scar tissues formed as a result of surgical incisions, traumatic cuts (e.g., traffic accidents), acne, keloids, or burns (Table 1). Scars were located on the face in 29 patients, on the extremities in 33 patients, and on the trunk in 47 patients. Thirty patients had undergone previous scar treatments such as skin grafts, scar tissue excision, or intralesional corticosteroids without satisfactory results prior to IPL treatment (Table 2). Patients who had postsurgical hypertrophied scar tissue development were not treated for at least 3 months after their surgery in order to determine that the scar tissue was indeed persistent.
The role of IPL treatment in the prevention of hypertrophic scarring after surgery was assessed in 17 patients who were known to have a predisposition for hypertrophic scarring. These patients were treated within 3–8 weeks after aesthetic surgery (abdominoplasty and breast reduction) while the postsurgical scars were still in their active growth phase.
Treatment
Each patient was treated with the IPL Quantum device. All patients received treatment at 2–4-week intervals; the number of treatments ranged from 1 to 24. Energy density varied from 30 to 40 J/cm2; cutoff filters of 550–590 nm, pulse durations of 2.1–10 ms, and pulse delays of 10–40 ms were used on all patients. The number of treatments administered was determined by the treating physicians based on the severity of the scarring. The treatments for each patient were completed through a minimum of six sessions.
Evaluation
Evaluations were done by grading the digital photographs of the scars taken during patient clinic visits. All photographs were taken with the same camera (Nikon D100 digital camera with a Nikon microdigital 100 mm SLR lens), magnification, lighting, angle, and film exposure. Patients with missing pre- and posttreatment photographs were excluded from ratings.
Two physicians who were unfamiliar with the patients and treatments conducted the clinical assessments. Pretreatment and posttreatment photographs of the patients were evaluated separately. The scars were rated for improvement in overall clinical appearance and in the reduction of scar height and erythema using the following scale: 0 = no visible improvement, 1 = minimal improvement, 2 = moderate improvement, 3 = good improvement, 4 = excellent improvement.
During the patient visits, possible side effects (e.g., posttreatment purpura) and discomfort due to pain or other sources, as well as any changes that had occurred (i.e., smoothness, change in color and hardness of the scars, and decrease in pruritus), were documented in the patients’ medical records by their treating doctors.
A phone survey about patient satisfaction with IPL treatment was performed. We were able to contact 86 (78.9%) patients. They were asked to grade their satisfaction using the following scale: 0 = no satisfaction, 1 = minimal, 2 = moderate, 3 = good, 4 = excellent (Table 3).
Results
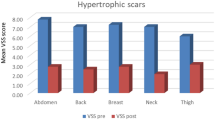
Overall, 144 patients (24 males and 120 females, age range = 2–55 years) who had IPL for hypertrophic scars or keloids were assessed. There were 35 patients with missing photographs and insufficient treatment who were excluded from the ratings. The remaining 109 patients were rated by two physicians and the average of the scores was used. The results of 109 patients who completed all treatments (6–24 sessions) are shown in Table 3 (posttreatment group). Midtreatment (1–5 sessions) results were available for 109 patients (Table 4).
There was an overall visible clinical improvement in the appearance of scars in all patients (100%) within the posttreatment group; improvement was excellent in 31.2%, good in 25.7%, moderate in 34%, and minimal in 9.1% (Table 5). A total of 56.9% were rated higher than 2 (moderate improvement), showing good or excellent improvement.
The coloring of the scars was rated according to a visible improvement of the erythema or darkness of the scar; improvement was excellent in 23.7%, good in 34.9%, moderate in 24.8%, and minimal in 9.1%. Overall, 59.7% of patients had good or excellent improvement (scores 3 and 4).
The texture of the scar, described as the height, showed improvement in 98.2%, with 69.8% scoring higher than 2 (good or excellent). Only 1.8% of the patients showed no improvement in scar texture.
The results of patients in the midtreatment group are given in Table 4. Good or excellent improvements were seen in 63.4% for clinical appearance, 54.1% for color, and 60.6% for scar height. Only 1.8% of patients in the midtreatment group showed no improvement.
Overall, 35 patients (32.1%) in the posttreatment group and 25 in the midtreatment group (22.9%) were rated excellent (average of 4 points) in all categories by both assessors, showing immense improvement in clinical appearance, coloring, and scar height (Figs. 1–4).
The results of the group of patients who underwent “preventive” IPL treatment are summarized in Table 6. Only four patients had completed their treatments. Despite the fact that the rest of the patients (13 in total) had not yet completed their treatment at the time of the assessment, the improvement was clearly visible. Sixty-five percent had good to excellent improvement in clinical appearance and 58.9% had scored 3 or 4 in the total average, showing good to vast improvement. Two patients had the full score in the prevention phase, showing immense scar healing.
In the medical notes of the treating doctors, an improvement of scar tissue with more pliability was noted for the majority of scars, most significantly for patients with burn scars, which enabled further surgical treatment by scar tissue excision. Staged surgical excisions were done in three patients (Fig. 5, two were done on the face of this patient).
The results of the phone survey about patient satisfaction with IPL treatment is summarized in Table 3. Seventy-sixty percent were satisfied with their treatment at good to excellent degrees. Only one patient was dissatisfied with it.
Complications
A lightening of skin color around the scar tissue was seen after the IPL treatment in four patients (we did not use tapes to close around the lesion). In three patients posttreatment purpura appeared but it was not persistent and disappeared within 2–3 weeks after treatment according to the medical records and photographs that were taken during follow-up. One patient experienced darkening of the scar, which made it more noticeable (Fig. 6).
Discussion
Hypertrophic scarring can be extremely frustrating for patients and physicians, eventually overshadowing the success of an aesthetic operation. This study demonstrates that intense pulsed light can induce significant overall clinical improvement in hypertrophic and keloid scars, particularly in terms of textural smoothing of scars, because of its use of near-infrared wavelengths. Among our patients who completed treatment, all experienced some clinical improvement in the appearance of the scars (100%), with 59.7% experiencing good or excellent improvement.
Current treatment options for hypertrophic scars and keloids, such as intralesional and topical corticosteroids, surgery, cryosurgery, CO2 laser treatment, silicone gel or sheet application, radiotherapy, application of pressure, and intralesional injection of triamcinolone, interferon, and 5-fluorouracil, have been shown to achieve flattening in some cases, but complete removal is never obtained [2, 3]. These methods vary in efficacy and their use is limited by high recurrence rates and side effects including atrophy and pigmentary changes [2, 3]. Many of these treatments are painful and time-consuming and some have side effects; in contrast, IPL treatment is noninvasive, i.e., it requires no injections, and therefore has few side effects. Two disadvantages of IPL treatment are the cost of the device and slight pain during administration, which can be made tolerable with cold and topical anesthetic cream (we used only cold to relieve pain following IPL treatment).
Because of the limitations of currently available treatments, other options such as short-pulsed PDL and LPDL have been previously used and reported to improve the appearance of hypertrophic scars [4–10, 12, 13, 18]. More recently, the flash lamp-pumped pulsed dye laser has emerged as a treatment of choice to affect long-term improvement in the appearance of hypertrophic scars [9, 10].
IPL treatment has been extensively researched and used for photorejuvenation, to treat vascular lesions, sun-damaged skin, a variety of pigmented lesions and rhytids, and to reduce the incidence of purpura [11, 12, 14–16]. It is also frequently used for hair removal [17, 18]. However, its use on hypertrophic or keloid scars has been reported in only a few studies [11, 12].
Bellew et al. [11] showed that IPL was as effective as 595-nm LPDL for scar treatment and that it had an additional significant effect on pliability of the scar. IPL, performed two times at 2-month intervals following suture removal, was found to be effective on surgically induced scars (abdominoplasty and breast reduction) [11]. Both LPDL and IPL significantly improved hypertrophic surgical scars (IPL 45% at first and 65% at second application and LPDL 55% and 80%, respectively). In that study, only surgically induced scars were treated and IPL and LPDL were applied following suture removal. It is not clear whether these scars would have been persistent because they were treated before complete wound healing [11]. The authors hypothesized that IPL treatment might affect the neovascularization that plays a vital role in wound healing and scar formation [11].
Kontoes et al. [12] reported a more than 75% improvement in pigmentation in hyperpigmented scars, more than 50% improvement in patients with tarmac tattooing scars, no significant improvement in the traumatic tattooing scars, more than 75% improvement in erythematous scars, more than 50% reduction in the scar’s size and bulk in patients with proliferative scars, and no significant improvement in atrophic scars. They also reported, as side effects, erythema and/or edema in the treated areas lasting usually 6 h, but up to 48 h in a few cases. No pigmentary changes (hyper- or hypopigmentation) on normal surrounding skin was observed because it was properly masked during treatment [12]. The authors hypothesized that IPL treatment might be applicable to and effective in almost all types of scars and could easily be combined with other treatment methods [12]. Their results are in accordance with ours. We agree with them that IPL is very effective for hyperpigmented, traumatic, erythematous, and proliferative scars. In addition, we propose that IPL can be used as a preventive in patients with a tendency to hypertrophic scarring and keloids. Also, it may be used to make excisional scar revisions easy in burn scars.
Our study included a large population of patients (n = 109) who underwent IPL treatment and it demonstrated a significant visible improvement of hypertrophic scars in the majority of patients. Many types of hypertrophic scars were evaluated, including surgical incisions, traumatic cuts (e.g., traffic accidents), acne scars, keloids, and burns (Table 1). The patients who had postsurgical hypertrophic scar tissue development were not treated until at least 3 months after their surgery in order to determine that the scar tissue indeed persisted.
Only photographs were used; there were with no measurements of scar color using spectrometry or thickness measurement via biopsies. Although we did not perform such measurements in our patients, these and additional tests such as ultrasound assessment of scar thickness, cutometer evaluation of scar firmness, and spectrophotometer measurement of erythema and pigmentation could be done to achieve a better assessment [1, 11–13]. Improved follow-up and assessment of prior treatments might also have an effect on the outcome.
Early studies utilizing the PDL demonstrated improvement in the erythema, thickness, texture, and pliability of hypertrophic scars [4–6, 9, 10, 12]. However, further studies have yielded conflicting data, with some more recent investigations finding no difference in PDL-irradiated scars over untreated controls [19–22], while others have confirmed the initial reports of improvement [7, 8, 12, 13]. Alster et al. [8] reported significant clinical and histologic improvement in hypertrophic inframammary scars after two treatments with LPDL. The results of Bellew et al. [11] confirm this reduction in erythema and scar height with the use of LPDL and IPL on both inframammary and lower abdominal surgically induced hypertrophic scars. Kontoes et al. [12] reported more than 50% improvement in hyperpigmented scars, tarmac tattooing, erythematous scars, and proliferative scars with the use of IPL. Overall, IPL treatments were rated as more painful than LPDL treatments but were still well tolerated. Although overall global improvement in scar appearance was assessed in Kontoes’ studies [11, 12], Bellew et al. [11] postulated that IPL may offer greater improvement in the textural smoothing component of scars than PDL due to its inclusion of near-infrared wavelengths, and Kontoes et al. [12] hypothesized that IPL treatment might be applicable to and effective in almost all types of scars and could easily be combined with other treatment methods. In our study we used IPL for all kinds of hypertrophic scars and keloids and observed significant clinical improvement in both, with especially greater improvement in the textural smoothing component of scars. The PDL device, however, is less painful due to air cooling. The addition of a topical anesthetic cream before IPL treatment would help reduce pain, making IPL tolerability comparable to that of LPDL [11]. However, the use of cold and local anesthetic creams before treatment causes vasoconstriction and decreases the effect of IPL so we used only cold for the relief of pain following treatment so as not to decrease the effect of IPL by vasoconstriction.
In a few patients we used IPL treatment in preparation for staged surgical excision of the scar tissues. Results from the midtreatment group demonstrated that even a few sessions can improve the scar quality overall. In the midtreatment group, 63.4% of patients had more than moderate improvement in clinical appearance, and only 1.9% of patients showed no improvement.
The use of IPL for the prevention of surgical scars has not been adequately assessed. As the complex interplay of molecules and cells involved in wound healing is becoming better understood, the ideal window of time in which to treat and even prevent hypertrophic scars is being further elucidated. PDL treatment of surgical and traumatic scars within the first few weeks has been shown to decrease the frequency of hypertrophic scarring [11, 19]. Nouri et al. [20] found that PDL treatment starting on the day of suture removal improved both the quality and cosmetic appearance of surgical scars. In addition, PDL has also been used to prevent hypertrophic scarring following deep dermal burns [11, 19, 22]. Because the Bellew et al. study administered IPL upon suture removal, this more closely approximates a prevention rather than a treatment study. They found significant improvement of 65% in hypertrophic surgical scars treated with two IPL applications [11]. In our study, there was a good to excellent improvement in 65% of patients who underwent preventive IPL treatment. Future avenues of investigation should include analyzing the early use of IPL to improve the final appearance of scars and to help prevent hypertrophic scarring [21].
Conclusion
Although knowledge of wound healing and metabolism is increasing, hypertrophic scars remain a challenge. IPL induced significant overall clinical improvement in hypertrophic and keloid scars, particularly in textural smoothing, likely because of its inclusion of near-infrared wavelengths. In addition, IPL was found to prevent hypertrophic scar formation when applied early after aesthetic surgery. There were minimal complications, which were transient and disappeared within a few weeks after treatment. A clear improvement in pliability of the scars was observed, which has enabled further surgical treatment for the reduction of the scar tissue. Further studies using more quantitative evaluations should be conducted.
References
Alster TS, Tanzi EL (2003) Hypertrophic scars and keloids: etiology and management. Am J Clin Dermatol 4:235–243
Alster TS, West TB (1997) Treatment of scars: a review. Ann Plast Surg 39:418–432
Chen MA, Davidson TM (2005) Scar management: prevention and treatment strategies. Curr Opin Otolaryngol Head Neck Surg 13:242–247
Bayat A, McGrouther DA (2005) Clinical management of skin scarring. Skinmed 4:165–173
Boutli-Kasapidou F, Tsakiri A, Anagnostou E, Mourellou O (2005) Hypertrophic and keloidal scars: an approach to polytherapy. Int J Dermatol 44:324–327
Smith FR (2005) Causes of and treatment options for abnormal scar tissue. J Wound Care 14:49–52
Alster TS (1997) Laser treatment of hypertrophic scars, keloids, and striae. Dermatol Clin 15:419–429
Alster TS, Lewis AB, Rosenbach A (1998) Laser scar revision: comparison of CO2 laser vaporization with and without simultaneous pulsed dye laser treatment. Dermatol Surg 24:1299–1302
Alster TS, Tanzi EL (2005) Re: the use of pulsed dye laser for the prevention and treatment of hypertrophic scars in Chinese persons. Dermatol Surg 31:252–253; author reply 253
Lupton JR, Alster TS (2002) Laser scar revision. Dermatol Clin 20:55–65
Bellew SG, Weiss MA, Weiss RA (2005) Comparison of intense pulsed light to 595-nm long-pulsed pulsed dye laser for treatment of hypertrophic surgical scars: a pilot study. J Drugs Dermatol 4:448–452
Kontoes PP, Marayiannis KV, Vlachos SP (2003) The use of intense pulsed light in the treatment of scars. Eur J Plast Surg 25:374–377
Hedelund L, Due E, Bjerring P, Wulf HC, Haedersdal M (2006) Skin rejuvenation using intense pulsed light: a randomized controlled split-face trial with blinded response evaluation. Arch Dermatol 142:985–990
Clementoni MT, Gilardino P, Muti GF, Signorini M, Pistorale A, Morselli PG, Cavina C (2006) Intense pulsed light treatment of 1,000 consecutive patients with facial vascular marks. Aesthetic Plast Surg 30:226–232
Lemperle G, Rullan PP, Gauthier-Hazan N (2006) Avoiding and treating dermal filler complications. Plast Reconstr Surg 118:92S–107S
Yamashita T, Negishi K, Hariya T, Kunizawa N, Ikuta K, Yanai M, Wakamatsu S (2006) Intense pulsed light therapy for superficial pigmented lesions evaluated by reflectance-mode confocal microscopy and optical coherence tomography. J Invest Dermatol 126:2281–2286
Butterwick KJ, Butterwick LS, Han A (2006) Laser and light therapies for acne rosacea. J Drugs Dermatol 5:35–39
Hurwitz DJ, Holland SW (2006) The L brachioplasty: an innovative approach to correct excess tissue of the upper arm, axilla, and lateral chest. Plast Reconstr Surg 117:403–411; discussion 412–403
Allison KP, Kiernan MN, Waters RA, Clement RM (2003) Pulsed dye laser treatment of burn scars. Alleviation or irritation? Burns 29:207–213
McCraw JB, McCraw JA, McMellin A, Bettencourt N (1999) Prevention of unfavorable scars using early pulse dye laser treatments: a preliminary report. Ann Plast Surg 42:7–14
Meshkinpour A, Ghasri P, Pope K, Lyubovitsky JG, Risteli J, Krasieva TB, Kelly KM (2005) Treatment of hypertrophic scars and keloids with a radiofrequency device: a study of collagen effects. Lasers Surg Med 37:343–349
Nouri K, Jimenez GP, Harrison-Balestra C, Elgart GW (2003) 585-nm pulsed dye laser in the treatment of surgical scars starting on the suture removal day. Dermatol Surg 29:65–73; discussion 73
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erol, O.O., Gurlek, A., Agaoglu, G. et al. Treatment of Hypertrophic Scars and Keloids Using Intense Pulsed Light (IPL). Aesth Plast Surg 32, 902–909 (2008). https://doi.org/10.1007/s00266-008-9161-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-008-9161-7