Abstract
Keloid scars are common and have a predilection for young, ethnic skin often with a family history. Keloids can be painful and pruritic and cause significant emotional distress when particularly visible or prominent. In this article, we review the evidence underlying the use of laser- and energy-based devices for treatment of keloid scars, either as monotherapy or in conjunction with other therapies such as corticosteroids, surgery and silicone gel in the treatment of keloid scars.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Keloid scars are common with a predilection to younger patients and higher Fitzpatrick skin types, particularly patients of African, Asian or Hispanic origin with an associated family history [1]. They present as raised protuberant nodules or plaques, often asymptomatic but may occasionally be pruritic or painful. Frequently, they cause significant distress to the patients, particularly if they are located on visible areas. Keloids can be caused by a multitude of mechanisms including injury, acne vulgaris, surgical trauma, piercings and burns. The pathogenesis of keloid formation is still not completely understood; however, theories include overproduction of type 1 procollagen in fibroblasts from keloid wounds with raised levels of transforming growth factor and platelet-derived growth factor [2]. Treatments of keloid scarring include topical and injected corticosteroids, silicone-based dressings, cryotherapy, surgical excision, 5-fluorouracil [3] and interferon alfa-2b injections [4]. In recent years, the use of laser- and energy-based devices for treatment of multiple dermatological conditions has become more widespread, with treatment of keloids proving no exception. We have systematically reviewed contemporary evidence supporting the use of light-, laser- and energy-based devices in the treatment of keloid scarring. We performed a systematic literature review using the Pubmed, Medline and Embase databases, employing the search terms ‘keloid’ and ‘laser’. Only articles written in the English language were evaluated. We also scrutinised citation lists from retrieved articles. Lasers can be subcategorized into ablative and non-ablative lasers which can be further subdivided into vascular and non-vascular strata.
Ablative lasers
The most commonly used ablative lasers are the erbium-doped yttrium aluminium garnet (Er: YAG) and carbon dioxide (CO2) lasers. Henderson et al. first reported the use of Argon and CO2 lasers to treat keloids in 1984 [5].To date, there are no published randomised controlled trials (RCTs) on the effectiveness of CO2 laser or Er:YAG lasers to treat keloid scars. We have identified ten studies reviewing the efficacy and safety of CO2 laser in the treatment of keloid scars (Table 1). Overall, 140 patients were included within the ten studies [6,7,8,9,10,11,12,13,14,15], which include retrospective reviews, prospective uncontrolled single studies and case reports with the largest sample size including 30 patients [15].
Ang and Tay carried out the most recent review in 2013, in which they compared the use of CO2 ablation to treat earlobe keloid scars to alternative treatment methods. A total of 16 patients were included within the study, eight of whom were treated with CO2 ablation, six with cold-steel surgery, one with combination treatment and one with triamcinolone (40 mg/ml) alone. The authors found that CO2 ablation and surgery had equally effective outcomes with regards to reducing earlobe keloid size based on the notes of physician assessment, whereas the patient treated with steroid injection only had a partial response. Of note, every patient treated with CO2 ablation or surgery had recurrence within 18 weeks of treatment completion [6].
Another study found that the combination of CO2 ablation with interferon alfa-2b injections given to all 30 patients with either trunk or auricular keloids led to no recurrence in 66% of the patients at 3 years post treatment, with no recurrence found in the auricular area [15].
Only one clinical study specifically reviewing the efficacy of Er:YAG in keloid scars has been published. Combination treatment of Er:YAG laser and twice-daily topical betamethasone under occlusion was carried out until scar flattening or no further improvement of the scar in 70 keloids (found in a total of 23 patients). This study found a median improvement of 50%. Of particular note, recurrences occurred in 22% of the treated lesions [16].
To date, there are no studies reviewing the efficacy of fractional ablative lasers in keloid scars.
Non-ablative vascular laser devices: vascular (PDL and Nd:YAG)
Non-ablative vascular lasers include the potassium titanyl phosphate (KTP), pulsed dye (PDL) and neodymium-doped yttrium garnet (Nd:YAG) lasers. There are no studies using KTP lasers for keloid scars.
The use of PDL lasers in keloid scars has been widely studied, with seven studies [18,19,20,21,22,23,24] conducted between 2000 and 2016, including a comparative randomised split-scar trial [18] and a prospective paired comparison RCT (Table 1) [20].
PDL monotherapy has shown to be effective in treating keloid or hypertrophic sternotomy scars. One study (n = 19) evaluated if the pulse width of a 595-nm flash lamp-pumped PDL held a bearing on outcome and found that the 0.45-ms width was superior to 40-ms width in reducing scar size [20]. Nouri et al. published a study on short- versus long-pulse therapy in scars and found the short pulse to also be more beneficial [37]. The hypothesis is that often, in scars (including keloids), the vessels are of small diameter; hence, according to the theory of photothermolysis, the short pulse width will confine heat within the vessels and thus produce a better outcome.
The largest study reported to date is a retrospective case series of 99 mainly Caucasian patients (85%) with keloid refractory to intralesional triamcinolone (ILT), treated with either PDL alone or rotational PDL combined with ILT. The study reviewed patient notes over a 5-year period and concluded monotherapy with PDL required 12–14 sessions for moderate to excellent outcomes versus only 4–5 sessions with combination treatment [19].
A single-blinded trial reviewed the outcome of a combination of ILT, 5-fluorouracil (5-FU) and PDL for keloid or hypertrophic scars. Sixty-nine patients were selected, of whom 60 completed the trial, and they were randomly distributed into three treatment groups. Group 1 was treated with ILT (10 mg/ml) weekly for 8 weeks, group 2 with ILT 0.1 ml of 40 mg/ml in combination with 5-FU (0.9 ml of 50 mg/ml) weekly for 8 weeks and group 3 was treated as per group 2 but lesions also had 585-nm flash lamp PDL treatment at weeks 1, 4 and 8. The trial demonstrated that all groups showed acceptable improvement but there was evidence of statistically more improvement in groups 2 and 3 (p < 0.05). Group 3 (with additional PDL treatment) was found to have subjectively better results than group 2, according to patients, and a higher percentage of blinded observer outcomes (70% in group 3 versus 40% in group 2) [21]. This indicates a more favourable outcome following combination therapy.
In 1984, Abergel et al. conducted an in vitro and subsequent clinical trial which demonstrated Nd:YAG laser to suppress collagen production and clinically flatten keloids post laser treatment (n = 8) with sustained improvement seen at 3-year follow-up [27]. Two more recent studies have been carried out reviewing the use of 1064-nm Nd:YAG laser to treat keloid and hypertrophic scars in 2013 and 2014. The first study demonstrated improvement in keloid scars with Nd:YAG laser, and the second found that anterior chest keloid scars did not respond as well as the hypertrophic scars to Nd:YAG treatment, with recurrence of keloid scarring being the issue [25, 26] highlighting the molecular differences between hypertrophic and keloid scars.
Koike et al. treated 102 Japanese patients with hypertrophic and keloid scars (n = 38 and n = 64 respectively) with 1064-nm microsecond Nd:YAG laser 3–4 times weekly for 52 weeks, using a spot size of 5 mm and 65–75 J/cm2 with 0.25-ms exposure and 2-Hz repetition rate. The results were evaluated using the Japan scar workshop score. A significant reduction in the score was found 1 year post treatment (p < 0.05). Recurrence, as with all previous methods, was observed at 6 months following treatment in 4% of hypertrophic abdominal scars, 52.9% of anterior chest keloids, 35.7% of upper arm keloids and 25% of scapula keloids. Authors postulated that hypertrophic scars responded better than keloid and keloid recurrence is more likely if any remaining redness or induration persisted following treatment [26].
Non-ablative non-vascular: Q-switched and fractional non-ablative
There have been several RCTs investigating the effects of fractional, non-ablative lasers [31,32,33] upon hypertrophic and surgical scars, but no studies have looked at keloid scarring specifically, and only smaller comparative or case series with regards to Q-switched laser and keloids have been carried out [28, 29].
Cho et al. reviewed the efficacy and safety of 1064-nm Q-switched Nd:YAG laser (low fluence) 5–6 passes at 1–2 weekly intervals in 12 Korean patients. At 3-month follow up, a significant improvement was found with regard to pigmentation, vascularity, pliability and height of the scar, with a 2.7-fold reduction in hospital burn scar assessment score (p < 0.001) in keloid and hypertrophic scarring [28].
Laser-assisted drug delivery
Lasers are increasingly being used to act synergistically with topical drugs, with a hypothesised mechanism of laser pre-treatment facilitating passage of topically applied drugs across the relatively impenetrable stratum corneum; consequently, lower drug doses or concentrations may provide similar therapeutic efficacy as the higher doses without laser pre-treatment, with less risk of adverse events [38]. It is thought that both ablative (fractional and non-fractional) lasers can have this effect. Fractional photothermolysis works by creating microscopic treatment zones (MTZs), thus enabling drug penetration whilst concomitantly enabling neocollagenesis via the preserved skin around the MTZs. Laser-assisted drug delivery has been used successfully for a variety of indications, including actinic keratoses, Bowen’s disease, vitiligo, vaccination and local anaesthetic application [38].
Cavalie et al. carried out a retrospective study using Er:YAG-fractionated laser combined with twice-daily topical betamethasone to treat refractory keloids until the scar had flattened or no further changes were found. They found that nine treatment sessions were required to produce a 50% reduction in the scar profile. Of note, keloid scarring recurred in 22% of the cohort 8 months post treatment [16].
Another prospective case series (n = 15), of mainly hypertrophic burn scars and some acne keloids scars, carried out three to five treatment sessions, at 2–3 monthly intervals, of fractional ablative laser in conjunction with topical triamcinolone (10-20 mg/ml) given immediately post laser. The assessment was evaluated by three blinded observers comparing baseline scar to the scar at 6 months post treatment and found a 2.73/4.0 average improvement [39].
Ethnic skin and laser
Pigmented skin types present particular challenges with regards to laser treatment. Higher Fitzpatrick skin types are associated with more melanin and greater fibroblast responses than fair skin [40] and hence higher risk of not only keloid scar formation but also reactive changes to lasers such as discoloration (notably hyperpigmentation), which remains a daily challenge to a dermatologist. Robust evidence on the treatment of keloid scars with lasers in ethnic skin is lacking.
Discussion
Conventional, longer-standing treatment options for keloid scars include topical and injected corticosteroids, silicone-based dressings, cryotherapy, surgical excision, 5-fluorouracil and interferon alfa-2b injections [4], each of which are often limited by poor outcome or recurrence. CO2 laser and PDL are the most widely used devices trialled for treatment of keloid scars.
Evidence belying the use of ablative lasers (Er:YAG and CO2) is encouraging but premised upon small studies with no RCTS, with the pervasive problem of keloid recurrence yet to be reckoned with [6].
The mechanism underlying laser treatment and improvement in keloid scarring has been analysed at a histological level. A laboratory-based study treated human keloid producing fibroblasts with a combination of CO2 and Er:YAG lasers. The levels of transformation growth factor beta 1 (TGF-β1), known for its role in wound healing, were reduced following treatment, implicating the role of TGF-β1 in the pathogenesis of keloid scarring following ablative laser therapy, similar to fractional lasers [17].
Non-ablative laser techniques, most notably PDL, have yielded encouraging outcomes, particularly when combined with corticosteroid injections, as discussed previously [19].
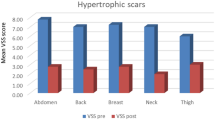
A comparative, randomised, split-scar trial compared 595-nm PDL with long-pulsed 1064-nm Nd:YAG laser in the treatment of hypertrophic and keloid scars after six laser sessions per patient at monthly intervals. One-month follow-up demonstrated the Vancouver scar scale (VSS) scores to be significantly reduced in both treatment arms (p < 0.001) with a higher (but non-significant) improvement in the Nd:YAG versus PDL groups (65.4 versus 55.14%, respectively) [18]. Of note, many practitioners do not use Nd:YAG devices for scars owing to the narrow therapeutic window and higher risk of bulk heating causing subsequent worsening of the scar.
As discussed earlier, it is apparent that the pulse width of a 595-nm flash lamp-pumped PDL has an important effect on outcome, with the 0.45-ms width being found to be superior to 40-ms width in reducing scar size [20].
With respect to monotherapy, there is evidence of benefit of treating keloid scars with CO2 [10, 13], Er YAG [17], PDL [18, 20], Nd:YAG [25,26,27] and Q-switched lasers [28, 29]; however, the evidence presented is from small studies with a paucity of RCTs. To date, there are no studies reviewing the use of fractional non-ablative laser or KTP laser in keloid scarring, with current inferences derived from studies of hypertrophic scarring [31, 32, 34, 41, 42].
Combination laser therapy to treat keloid scarring is much more widely researched. Often, different laser subsets are combined with intralesional steroid injections [7, 11, 19, 21, 24]; however, there is also evidence for laser therapy in combination with other laser modalities [7, 17, 29], cyanoacrylate glue [9], interferon alfa 2b injections [15], topical corticosteroids [16] and 5-fluorouracil [21, 23]. Combination therapy was found to be far more efficient in terms of treatment sessions required [19]. Whilst promising, the aforementioned studies are small and larger RCTs are required.
Koike et al. highlighted the pertinent fact that keloid recurrence is more likely if any remaining redness or induration persisted following treatment [26].
Of interest, Niwa et al. demonstrated that 1550-nm erbium-doped fractional photothermolysis in hypertrophic scars (n = 8) appeared to induce moderate improvement [34] but research specific to keloid scarring is still lacking.
Recurrence rate and follow-up
Whilst a multitude of energy-based devices show promise in treating keloid scars, recurrence of lesions remains an issue [43]. Recurrence of keloids following CO2 laser treatment may present from as short as 2 weeks post treatment [6] and up to 3 years post treatment [11, 15], and Er:YAG has demonstrated a 22% recurrence at 8-month follow up [16]. Nd:YAG showed variable recurrence percentages at 6 months post treatment dependent on the anatomical site of the keloid, with one study reporting recurrence in 52.9% anterior chest keloids, 35.7% upper arm keloids and 25% scapula keloids [26], suggesting that not only treatment modality and mechanism but also anatomical site of keloid determines the likelihood of recurrence. A shortcoming of the majority of the studies is the failure or inability to undertake follow-up beyond 12 months, hampering our capacity to draw inferences about the long-term consequences of treatment.
Future considerations
Whilst the presented data are promising, larger RCTs for each modality of therapy with longer follow-up duration would further enhance our understanding of the role of light-, laser- and energy-based devices in treatment of keloid scars. All of the evidence has been labelled according to the strength of recommendation taxonomy (SORT) criteria to enable clinicians to rate the quality of the evidence presented [44]. In order for a study to be classified as SORT level A, it must meet strict criteria; for example, either be a Cochrane review or show consistent findings from two or more good-quality RCTs. From our entire search, there were only two SORT A studies and the remaining were of SORT B/C criteria. Thus, this demonstrates the need for more robust studies in order to enable clinicians to guide their decision on the treatment of keloids based on high-quality evidence. Some of the reported studies conflate hypertrophic and keloid scars; studies using a stringently defined cohort of exclusively keloid scars would be instructive. In addition to combination therapies, neoteric approaches such as laser-assisted drug delivery and LASH may show future promise. Increased adoption of these nascent techniques and future comparative studies will lead to a more comprehensive understanding of the role of these devices in the treatment of keloid scars.
References
Ud-Din S, Bayat A (2013) Strategic management of keloid disease in ethnic skin: a structured approach supported by the emerging literature. Br J Dermatol 169:71–81
Chike-Obi CJ, Cole PD, Brissett AE (2009) Keloids: pathogenesis, clinical features, and management. Semin Plast Surg 23(3):178–184
Shah VV, Aldahan AS, Mlacker S et al (2016) 5-Fluorouracil in the treatment of keloids and hypertrophic scars: a comprehensive review of the literature. Dermatol Ther 6(2):169–183
Juckett G, Hartman-Adams H (2009) Management of keloids and hypertrophic scars. Am Fam Physician 80(3):253–260
Henderson DL, Cromwell TA, Mes LG (1984) Argon and carbon dioxide laser treatment of hypertrophic and keloid scars. Lasers Surg Med 3(4):271–277
Ang C-C, Tay Y-K, Kwok C (2013) Retrospective analysis of earlobe keloids treated with the carbon dioxide laser ablation or cold steel debulking surgery. J Cosmet Laser 15(5):271–273
Martin MS, Collawn SS (2013) Combination treatment of CO2 fractional laser, pulsed dye laser, and triamcinolone acetonide injection for refractory keloid scars on the upper back. J Cosmet Laser Ther 15(3):166–170
Nicoletti G, De Francesco F, Mele CM et al (2013) Clinical and histologic effects from CO2 laser treatment of keloids. Lasers Med Sci 28(3):957–964
Tenna S, Aveta A, Filoni A et al (2012) A new carbon dioxide laser combined with cyanoacrylate glue to treat earlobe keloids. Plast Reconstr Surg 129(5):843e–844e
Scrimali L, Lomeo G, Tamburino S et al (2012) Laser CO2 versus radiotherapy in treatment of keloid scars. J Cosmet Laser Ther 14(2):94–97
Garg GA, Sao PP, Khopkar US (2011) Effect of carbon dioxide laser ablation followed by intralesional steroids on keloids. J Cutan Aesthetic Surg 4(1):2–6
Scrimali L, Lomeo G, Nolfo C et al (2010) Treatment of hypertrophic scars and keloids with a fractional CO2 laser: a personal experience. J Cosmet Laser Ther 12(5):218–221
Morosolli ARC, De Oliveira Moura Cardoso G et al (2008) Surgical treatment of earlobe keloid with CO2 laser radiation: case report and clinical standpoints. J Cosmet Laser Ther 10(4):226–230
Driscoll B (2001) Treating keloids with carbon dioxide lasers. Arch Otolaryngol Head Neck Surg 127(9):1145
Conejo-Mir JS, Corbi R, Linares M (1998) Carbon dioxide laser ablation associated with interferon alfa-2b injections reduces the recurrence of keloids. J Am Acad Dermatol 39(6):1039–1040
Cavalié M, Sillard L, Montaudié H et al (2015) Treatment of keloids with laser-assisted topical steroid delivery: a retrospective study of 23 cases. Dermatol Ther 28(2):74–78
Cheng ET, Nowak KC, Koch RJ (2001) Effect of blended carbon dioxide and erbium:YAG laser energy on preauricular and ear lobule keloid fibroblast secretion of growth factors: a serum-free study. Arch Facial Plast Surg 3(4):252–257
Al-Mohamady AE-SAE-H, Ibrahim SMA et al (2016) Pulsed dye laser versus microsecond Nd:YAG laser in the treatment of hypertrophic scars and keloid: A comparative randomized split-scar trial. J Cosmet Laser 18(4):208–212
Stephanides S, Rai S, August P et al (2011) Treatment of refractory keloids with pulsed dye laser alone and with rotational pulsed dye laser and intralesional corticosteroids: a retrospective case series. Laser Ther 20(4):279–286
Manuskiatti W, Wanitphakdeedecha R, Fitzpatrick RE (2007) Effect of pulse width of a 595-nm flashlamp-pumped pulsed dye laser on the treatment response of keloidal and hypertrophic sternotomy scars. Dermatol Surg 33(2):152–161
Asilian A, Darougheh A, Shariati F (2006) New combination of triamcinolone, 5-fluorouracil, and pulsed-dye laser for treatment of keloid and hypertrophic scars. Dermatol Surg 32(7):907–915
Bellew SG, Weiss MA, Weiss RA (2005) Comparison of intense pulsed light to 595-nm long-pulsed pulsed dye laser for treatment of hypertrophic surgical scars: a pilot study. J Drugs Dermatol JDD 4(4):448–452
Manuskiatti W, Fitzpatrick RE (2002) Treatment response of keloidal and hypertrophic sternotomy scars: comparison among intralesional corticosteroid, 5-fluorouracil, and 585-nm flashlamp-pumped pulsed-dye laser treatments. Arch Dermatol 138(9):1149–1155
Connell PG, Harland CC (2000) Treatment of keloid scars with pulsed dye laser and intralesional steroid. J Cutan Laser Ther 2(3):147–150
Rossi A, Lu R, Frey MK et al (2013) The use of the 300 microsecond 1064 nm Nd:YAG laser in the treatment of keloids. J Drugs Dermatol JDD 12(11):1256–1262
Koike S, Akaishi S, Nagashima Y et al (2014) Nd:YAG laser treatment for keloids and hypertrophic scars: an analysis of 102 cases. Plast Reconstr Surg Glob Open 2(12):e272
Abergel RP, Dwyer RM, Meeker CA et al (1984) Laser treatment of keloids: a clinical trial and an in vitro study with Nd:YAG laser. Lasers Surg Med 4(3):291–295
Cho S, Lee J, Lee S et al (2010) Efficacy and safety of 1064-nm Q-switched Nd:YAG laser with low fluence for keloids and hypertrophic scars. J Eur Acad Dermatol Venereol 24(9):1070–1074
Bowes LE, Nouri K, Berman B et al (2002) Treatment of pigmented hypertrophic scars with the 585 nm pulsed dye laser and the 532 nm frequency-doubled Nd:YAG laser in the q-switched and variable pulse modes: a comparative study. Dermatol Surg 28(8):714–719
Issa MCA, Kassuga LEBP, Chevrand NS et al (2013) Topical delivery of triamcinolone via skin pretreated with ablative radiofrequency: a new method in hypertrophic scar treatment. Int J Dermatol 52(3):367–370
Verhaeghe E, Ongenae K, Bostoen J et al (2013) Nonablative fractional laser resurfacing for the treatment of hypertrophic scars: a randomized controlled trial. Dermatol Surg 39(3 Pt 1):426–434
Lin JY, Warger WC, Izikson L et al (2011) A prospective, randomized controlled trial on the efficacy of fractional photothermolysis on scar remodeling. Lasers Surg Med 43(4):265–272
Tierney E, Mahmoud BH, Srivastava D et al (2009) Treatment of surgical scars with nonablative fractional laser versus pulsed dye laser: a randomized controlled trial. Dermatol Surg 35(8):1172–1180
Niwa ABM, Mello APF, Torezan LA et al (2009) Fractional photothermolysis for the treatment of hypertrophic scars: clinical experience of eight cases. Dermatol Surg 35(5):773–778
Capon A, Iarmarcovai G, Gonnelli D et al (2010) Scar prevention using laser-assisted skin healing (LASH) in plastic surgery. Aesthet Plast Surg 34(4):438–446
Cassuto DA, Scrimali L, Siragò P (2010) Treatment of hypertrophic scars and keloids with an LBO laser (532 nm) and silicone gel sheeting. J Cosmet Laser 12(1):32–37
Nouri K, Elsaie ML, Vejjabhinanta V et al (2010) Comparison of the effects of short- and long-pulse durations when using a 585-nm pulsed dye laser in the treatment of new surgical scars. Lasers Med Sci 25(1):121–126
Ali FR, Al-Niaimi F (2016) Laser-assisted drug delivery in dermatology: from animal models to clinical practice. Lasers Med Sci 31(2):373–381
Waibel JS, Wulkan AJ, Shumaker PR (2013) Treatment of hypertrophic scars using laser and laser assisted corticosteroid delivery. Lasers Surg Med 45(3):135–140
Alexis AF (2013) Lasers and light-based therapies in ethnic skin: treatment options and recommendations for Fitzpatrick skin types V and VI. Br J Dermatol 169(Suppl 3):91–97
Keaney TC, Tanzi E, Alster T (2016) Comparison of 532 nm potassium titanyl phosphate laser and 595 nm pulsed dye laser in the treatment of erythematous surgical scars: a randomized, controlled, open-label study. Dermatol Surg 42(1):70–76
Yun J-S, Choi Y-J, Kim W-S et al (2011) Prevention of thyroidectomy scars in Asian adults using a 532-nm potassium titanyl phosphate laser. Dermatol Surg 37(12):1747–1753
Park TH, Chang CH (2012) Letter regarding ‘Clinical and histologic effects from CO(2) laser treatment of keloids’. Lasers Med Sci 27(6):1259–1259
Strength of recommendation taxonomy (SORT): a patient-centered approach to grading evidence in the medical literature—American Family Physician. http://www.aafp.org/afp/2004/0201/p548.html. Accessed on 26 April 2017
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Additional information
What’s already known about this topic?
• Keloid scars have a higher predilection for younger, ethnic skin.
• Keloid scars can be caused by a multitude of mechanisms, including injury, acne, surgical trauma, piercings and burns.
• Existing treatments for keloid scars include corticosteroid injections, silicone sheeting, cryotherapy, surgical excision, 5-fluorouracil and interferon alfa-2b injections, radiotherapy.
What does this study add?
• We have comprehensively reviewed and summarised contemporary literature relating to the use of light-, laser- and energy-based devices for treatment of keloid scars and quantified the evidence according to the strength of recommendation taxonomy criteria.
• Although initial findings are promising for multiple subcategories of lasers, lights and fractional radiofrequency, current evidence comprises multiple small studies and with few randomised trials
• The use of lasers in keloids is a relatively new concept, as either monotherapy or an adjunct to medical therapies. Future use of laser-assisted delivery to treat keloid scars has potential.
Rights and permissions
About this article
Cite this article
Forbat, E., Ali, F.R. & Al-Niaimi, F. Treatment of keloid scars using light-, laser- and energy-based devices: a contemporary review of the literature. Lasers Med Sci 32, 2145–2154 (2017). https://doi.org/10.1007/s10103-017-2332-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10103-017-2332-5