Abstract
Purpose
Higher patient’s expectations and dissatisfaction following total knee arthroplasty are well-documented phenomena. Despite the implications of different patients’ related factors both modifiable and nonmodifiable, in the last decade a lot of emphasis has been focused on surgical technique, implant alignment and stability both as a cause and a potential solution of several problems.
Methods
Different alignment and balancing techniques have been recently described and the introduction of new technologies such as computer and robotic-assisted surgery have been the basis for their optimization. In this paper, the surgical technique of the ROSA Knee System will be described focusing on the potential alignment options and the ligament balancing technique. The current literature available about the system will also be analyzed.
Results
The ROSA® robotic system have been recently introduced in the market and presents specific and peculiar features to optimize ligament balancing and an individualized alignment of the implant in a three dimensional prospective.
Discussion
The system is showing a favourable gap balancing technique and the possibility to create an individualized alignment. Preliminary results have now been shown in the literature both on the accuracy of the system and on clinical outcomes.
Conclusions
Preliminary results are promising both in terms of accuracy of the system and of clinical outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent years, robots are gaining popularity in the field of orthopaedics and particularly in total knee arthroplasty (TKA), for different reasons such as improved accuracy of implant positioning and reduced outliers in limb alignment comparing to conventional jig-based TKA [1,2,3,4].
Following the introduction of computer and robotic-assisted surgery, different techniques and alignment options have evolved. From one side, mechanically aligned knees may be more respectful for the design of the implant, but less of the soft tissue envelope while kinematic or anatomic alignments may be able to recreate the original joint line, respecting the soft tissues while ignoring a mechanical concept, which is the base of the kinematic design of the current implants. Different so called “functional alignment” options have also been presented as hybrid techniques to obtain on side a mechanically functional and on the other a soft tissue-friendly alignment targets to be identified and achieved [5, 6].
Different robotic systems are available on the market, and they all differ substantially in terms of software features and surgical activity, although all based on a Navigation System that can be either image based or image-less [7].
In the world of robotics different tools are available: from fully active to semi-active systems [8]. On one side, fully active robots work autonomously to perform the planned bone resections while on the other with semi-active systems the surgeon keeps the overall control over resections and implant positioning, but receives from the robot live intra-operative feedbacks (haptic or not) and the robotic arm constrain deviation from the pre- and intra-operative surgical plan particularly avoiding soft tissue impingement or bony over-resections [8, 9]. The ROSA® (Zimmer-Biomet Warsaw IN) robotic-arm system was designed to couple a robotic placement of the cutting jigs with ligament balancing evaluation performed in a dynamic fashion [10, 11]. It can be considered as a “collaborative robotic” system. The robot’s task is to help in placing the cutting jigs, while it’s the surgeon performs the sawing through them. This features differentiates it from other systems available on the market such as haptic arm robots, keeping the surgeons in defined boundaries, or milling robotic systems either based on a passive mode where the surgeon is actively involved in the milling process with the device retracting when reaching the boundaries, either working on an active fashion doing itself the milling process without the direct involvement of the surgeon [12, 13]. Differently from other Robotic Systems available, the ROSA can work both on an image-based or image-less basis. The image-based option utilizes a 3D virtual model derived from 2D full-length pre-operative plain radiographs, while the image-less mode is exclusively based on intra-operative landmarks acquisition [14].
Aim of this paper is to describe the surgical technique of the ROSA Knee System focusing on the potential alignment options and ligament balancing technique and to analyze the current literature available about the system.
Methods
Robotic procedure
The patient is placed on the surgical table in supine position. The robot’s position close to the patient’s hip. Two trackers are placed on the patient’s femur and tibia as a reference for leg movements and a third is located on the robotic unit, to track it relatively to the patient’s leg during the surgery. After the approach and the arthrotomy, the surgeon performs the knee state evaluation, starting with the registration of the femoral and tibial landmarks. In this phase, accuracy is important both in the imageless (where bone morphology and resections are based only on the correct quality of the acquisition) as well as in the image-based procedure, where the surgeon can proceed only if the landmark points show a correspondence with the pre-op radiographic planning. After the definition of the bone morphology the surgeon performs the evaluation of the ligament status and competence with a varus-valgus stress test at different degrees of flexion (0°, 30°, 45°, 60°, 90°, 120°). This provides quantitative information about the operated knee range of motion (in degrees), overall alignment of the limb, as well as varus/valgus deformity (in degrees) and ligament laxity (in mm) at different angles. Following these steps, intra-operative planning is performed by the surgeon, using the dedicated software, to determine the ideal resection thickness and angle to obtain a balanced and well-aligned TKA.
During this planning, several parameters are determined: the femoral (and tibial in the image-based procedure) component size, the orientations of the bone cuts (femoral distal, posterior and anterior, tibial) and their thickness based on the bony and ligaments references. Predictive values of the final gaps and alignment are provided, live and with real time modifications, by the system.
After the planning phase, the robot places the jig according to the surgical plan for the tibial and the distal femoral cuts and determines the position of the 4-in-1 resection guide. The robotic arm has three modes of action: automatic, collaborative, and static. In the automatic mode, when the robotic arm is far from the knee, the robot moves in the space autonomously. The robot switches to a so-called collaborative mode when approaching the knee and the surgeon can drive the robotic arm by applying a gentle force on the guide and place it on the bone surface within the cutting plane. At this step, the robotic arm movement is limited to the planned cutting surface but follows the knee in any of its movement adapting its positioning relative to the joint in order to perform the correct cut. The correct positioning of the jig is verified and optimized by looking at live cut values on the screen; then robotic arm is then fixed to the joint by switching to a static mode which allows the surgeon to perform the different cuts with the robotic arm stably fixed and pinned to the bone.
Different surgical strategies can be performed with the ROSA knee, according to the surgeon’s preferences. All the classic and the newer techniques can be performed: measured resection, gap balancing, functional alignment, kinematic alignment. The software navigates the procedure between the different surgical steps according to the surgeon’s preference for alignment, implants positioning, but also for the correct ligament balancing in flexion and extension.
Results
The concept of individualized alignment
The concept individualized alignment is based on the possibility to evaluate and assess in real time resection thickness, joint gaps, and limb alignment and their interactions during surgery. The additional precision offered by the robotic techniques means that any target in limb alignment can be achieved more reproducibly, with higher accuracy reducing the risk of significant alignment outliers and balancing the knee in all three spaces in a harmonic way.
Both principles of measured resection and gap-balancing techniques are used.
The limb alignment can be assessed intra-operatively before and after osteophytes removal, the coronal correction can be evaluated at different degrees of flexion and applying varus or valgus stresses to correct the deformity and evaluate the ligament competence throughout the whole range of motion.
This allows the software to generate the size of the potential gaps, both in extension and at 90° of flexion, as well as to assess the laxity throughout different degrees of flexion.
In this phase, the surgeon has a direct visualization of the effects that any modification of bone cuts alignment and potential ligament release may have on the balancing of the gaps.
With the concept of individualized alignment, the gaps can be balanced by changing the implant targets in all three planes. The surgeon can decide to give the best alignment option for each patient and compensate any gap imbalance with adjustments on bone cuts, minimizing any ligament release. With the ROSA system, once the extension gap has been correctly balanced a dedicated “rotational tool”, allows to balance the flexion with the extension gap using of the Fuzion® (Zimmer-Biomet Warsaw IN) system.
These targets are individualized to the patient’s knee and gaps.
With the use of the robotic technology, gap balancing and limb alignment can be kept within safe limits and the overall limb alignment can be kept within a safe and controlled zone of coronal alignment.
These limits may evolve with further studies and become broader. With an individualized alignment a valgus correction can be applied to the distal femoral resection and varus correction to the tibial resection aiming for the obliquity of the joint line if and when needed.
The height of the joint line can be preserved avoiding under or over-resection of the distal femur reducing the risk of mid-range instability associated with raising of the joint line or flexion instability due to attempts to compensate for a tight extension gap with a thinner polyethylene insert.
The concept of individualized alignment is not limited to the coronal plane, and its goal is to implant the components in the position that is better conforming to the soft tissue envelope of the knee. The target is to restore the correct plane and obliquity of the joint line and to balance the gaps correctly according to the ligaments tension and competence.
In severe deformities, some ligament releases may be required to balance the gaps and the medial and lateral collateral ligaments. The extent and frequency of such releases can be performed under a live and continuous feedback to evaluate the entity which is smaller when compared with a standard mechanical alignment technique.
Balancing procedure
Once bony landmarks and ligaments tension have been registered the system presents a planning to be assessed by the surgeon.
-
The surgeon has first the possibility to choose or change the implant and the referencing method (Persona, Nex Gen System or Vanguard system, PS or CR; anterior or posterior referencing) and the system automatically adapts the planning and the dimensions of the gaps according to the chosen implant and chosen anterior or posterior referencing.
-
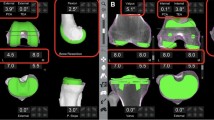
The system provides two Navigating pages on the same screen, one referring to the bone cuts and one for the gap balancing (Fig. 1):
-
On the first one it is possible to modify the planned cuts of the flexion and varus/valgus angle of the distal femur and of the tibial slope and varus valgus cut.
-
The second one shows the gap obtained merging the planned cuts with the ligament tensions registered and reports the gap obtained on the medial and lateral side both in flexion and in extension; any adjustment performed on the planning of the cuts is in real time reported on the planning showing the modifications of the gaps.
-
The system also provides a planning of the final alignment obtained.
-
The surgeon can decide to give the best coronal alignment option for each patient and compensate any gap imbalance with adjustments on bone cuts, minimizing any ligament release.
-
A direct visualization of the effects that any modification of bone cuts alignment and potential ligament release may have on balancing of the gaps is available
-
The procedure can start with a definitive planning of the extension gap and only a provisional planning of the flexion gap as once the cuts for the extension gap are reported, the flexion gap can be adjusted with the “rotational tool” to be balanced with the extension.
-
The procedure can start both with the distal femoral or with the proximal tibial cut; on the surgical plan is set the robotic arm moves and position an universal cutting jig on the bone. The cutting jig is then firmly pinned to the bone and the surgeon can perform the cuts through it. In these phases, the operator have a direct live cut visualization and can check the proper positioning of the robotic arm in real time.
-
After each resection, the surgeon can verify and validate the cuts with a specific validation tool (Fig. 2). The validated measures if different from the original plan, can be reported on the plan at each step, modifying it accordingly.
-
As well, after each resection it is possible to reassess the ligament tension (manually or using the Fuzion tensioner) and modify the planning according to the new registered tensions.
-
Modified ligament laxity should also be assessed and planning reassessed if any release is performed.
-
When the first two cuts are performed and the extension gap obtained, an evaluation of the extension gap is performed and verified either with a static spacer or with a balancing tool (Zimmer Fuzion® spacer block or tensioner).
-
The added value of the system is now the Femoral Rotation Tool, which drives the 4-in-1 cutting block balancing the flexion gap on the previously performed and measured extension gap. The systems utilizes a tool called Fuzion® and a technique designed to merge the measured resection and the gap balancing techniques [15]. Once the femoral distal and the proximal tibial cuts are performed, a distraction test is performed and the ROSA will register quantitative information on the medial and lateral ligaments tension and laxity. This test can be performed both with a 10- or 12-mm spacer, or with the Fuzion system (both tensioner or spacer block, which, during this step, has a 9-mm shim in place). The ROSA measures and register these values on the extension gap and show the frontal alignment obtained. The knee is then positioned at 90° of flexion and the Fuzion instrument is positioned again in the flexion space without the 9 mm shim. If the FuZion tensioner instrument is used, this is tensioned to equally tension the medial and lateral compartments in flexion. The system will now register the flexion gap values and assess the 4 in 1 cutting jig position (and so the femoral component rotation) to equally match the extension gap. The ROSA will then drive the drilling for the two holes of the 4-in-1 femoral resection bloc to obtain the ideal femoral rotation with a correct balance between the two gaps (Fig. 3).
-
With the robotic arm in place, the surgeon will be driven in drilling the holes for the dedicated classic 4-in-1 posterior (or anterior according to the chosen technique) referenced cutting jig that setting the anterior–posterior position and rotation of the femoral component. The remaining femoral cuts are then performed with the conventional cutting jig in place.
-
With the trial components on, it is possible to evaluate the ligament balance and the degree of residual deformity of the knee (Fig. 4).
-
At this point, any imbalance can be evaluated and addressed with different potential solutions such as, use of a thicker liner, recuts or ligament releases.
-
The preparation of the tibial metaphysis and the patella are performed with standard instrumentation.
-
-
Use of ROSA in a classic feature
The system can be also used in a conventional way aiming to achieve a neutral limb alignment (with 0 ± 3), by implanting the femoral and tibial components perpendicular to the mechanical axis. The main advantage is to be able to register and plan the cuts on that fashion having direct feedback on ligaments and gaps tensions and on the effects of any potential release. The cuts can be either independent (and starting either from the tibia or from the femur) or reciprocally dependent, as the distal and posterior femoral cuts are performed parallel to the tibial cut. Ligament balancing can be achieved using soft tissues releases to create the same tension between the medial and lateral compartment, both in the flexion and extension gap. The stability of the joint is then obtained by the design and the kinematic of the implant that fills the flexion and extension gap in the same manner with its conformity.
Discussion
The ROSA Knee System have been recently introduced on the market and is considered as a collaborative robotic system. It allows to obtain an individualized alignment based on the surgeon’s preference and the patients characteristics. The operator can decide his surgical strategy and perform his preferred workflow in terms of implant positioning and limb alignment, sequence of bone cuts and ligament balancing. No bone morphing is needed, and the landmark’s acquisition is straight forward as well as the surgical planning that can be visualized, with all the required data, on a few screens. The system has been conceived to help the surgeon to improve his accuracy for bone resections and the ligament balancing and to achieve an individualized alignment for each patient based on the feedback information that the system gives to the surgeon as described by the group of Scuderi [14].
Regarding the versatility and simplicity of the system Vanlommel et al. [16] in their retrospective cohort study showed a very quick learning curve on a series of 90 patients undergoing robotic-TKA (rTKA) using the ROSA Total Knee System versus 90 operated with a traditional manual TKA (mTKA) by a high-volume orthopaedic surgeon. The initial learning curve was achieved in six to 11 cases for operative time with similar 90-day complication rates and improved implant alignment.
Similar results have been shown by Bolam et al. [17] comparing 83 consecutive conventional jig-based TKAs with 53 robotic TKAs performed with the same robotic system by three high-volume surgeons. Operative times did not differ significantly (p = 0.92) and the authors did not register a discernible learning curve for the components planning accuracy. No significant difference (p > 0.99) was shown in post-operative complication rates. The authors concluded that the introduction of the system did not imply major risks and accounted for a learning curve of 8.7 cases regarding only operative time.
Analogue advantages have been shown by Batailler et al. [10] in their publication focused on describing the concept and the surgical technique of the ROSA Knee System for TKA, its advantages and potential limits and reporting the early experience with the system. In their study, the authors stress on the versatility and the adaptability of the system underlining the possibility of applying different technique and alignment options.
From a behavioural point of view, Haffar et al. [18] showed that rTKA with the ROSA system resulted in less surgeon physiologic stress, energy expenditure per minute, and postural strain compared to conventional TKA and that robotic assistance may help to increase surgical efficiency and reduce physician workload. The authors suggest these benefits may reduce musculoskeletal pain and injury among surgeons.
The ROSA system have shown increased accuracy both on a cadaveric as in an in vivo studies.
Charette et al. [19] showed on a cadaveric setting that the registration of anatomic landmarks and the gap assessment was highly repeatable with low variability among observers using both image-based and image-less software of the ROSA robotic system.
Parratte et al. [11] in a cadaveric setting used the ROSA Knee System with three different implants demonstrating high accuracy of the system; standard deviation for alignment on the coronal and sagittal plane for both tibia and femur was less than one. A standard deviation of less than one was also shown for planned and measured bone resections. Mean hip-knee-ankle axis difference between the measured and the planned axis was 0.03 ± 0.87, with a rate of malalignment > 3° of 0%.
Rossi et al. [20] reproduced a similar study in vivo demonstrating a high level of accuracy of cuts, angular values and post-op limb alignment; Standard deviation was inferior to one between planned, validated and measured cuts and angles. The robot was also reliable in reproducing the planned HKA with a mean difference between planned and measured axis of 1.2 ± 1.1. with no statistically significant difference.
Differently, Shin et al. [21] did not show the same satisfactory results in terms of accuracy in a smaller cohort of 37 patients where The ROSA system but was inaccurate in calculating both γ and δ angles while accurately calculated the HKA, α, and β angles.
Concerning clinical outcomes Mancino et al. [22] compared the functional outcomes and PROMs of 50 imageless ROSA TKA with 47 imageless Navigated TKA at one year follow-up. They demonstrated significant differences for the “pain” subsection of the KOOS score. In addition, robotic TKA showed higher maximum range of motion and a better mean improvement of the arc of motion. The authors concluded that the robotic group was associated with longer surgical time, better pain perception, and improved ROM at 12-month follow-up.
Batailler et al. [23] in a recent study compared sequential robotic versus traditional bilateral TKA. The study confirmed that despite a longer operative time, results between the two groups were comparable in terms of post-op complications and that the new technique is at least as safe as a the conventional one, without additional risk of complications.
Parratte et al. [24] introduced and showed promising clinical outcomes with the concept of an anatomo-functional implant positioning (AFIP) technique using the ROSA Robotic system. The authors showed a faster recovery at 6 months compared to an adjusted mechanical alignment concluding that this robotic technique may allow the restoration of the native knee alignment and with a more natural and functional ligament balance.
Kenanidis et al. [25] in a prospective matched cohort study compared two groups of 30 patients undergoing mechanical or ROSA robotic assisted. Patients undergoing robotic TKA showed less pain, better patient satisfaction, and PROMs at 6-month with the same complication rate.
Finally, Vermue et al. [12] in a recent systematic review analyze the different robotic systems concluding and underlying the difficulties for a comparison between different systems as the current evidence regarding each one differs both in quantitative and in qualitative measures and outcomes. Each system has specific features and a specific workflow and it becomes complicated to assess comparisons with other systems working in a different manner.
Conclusions
The ROSA Knee System is showing a favorable gap balancing technique and the possibility to create individualized alignment. Preliminary results are promising both in terms of accuracy of the system and of clinical outcomes.
References
Hampp E, Chughtai M, Scholl L et al (2019) Robotic-arm assisted total knee arthroplasty demonstrated greater accuracy and precision to plan compared with manual techniques. J Knee Surg 32:239–250. https://doi.org/10.1055/s-0038-1641729
Vaidya NV, Deshpande AN, Panjwani T et al (2022) Robotic-assisted TKA leads to a better prosthesis alignment and a better joint line restoration as compared to conventional TKA: a prospective randomized controlled trial. Knee Surg Sports Traumatol Arthrosc 30:621–626. https://doi.org/10.1007/s00167-020-06353-2
Zhang J, Ndou WS, Ng N et al (2022) Robotic-arm assisted total knee arthroplasty is associated with improved accuracy and patient reported outcomes: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 30:2677–2695. https://doi.org/10.1007/s00167-021-06464-4
Kort N, Stirling P, Pilot P, Müller JH (2022) Robot-assisted knee arthroplasty improves component positioning and alignment, but results are inconclusive on whether it improves clinical scores or reduces complications and revisions: a systematic overview of meta-analyses. Knee Surg Sports Traumatol Arthrosc 30:2639–2653. https://doi.org/10.1007/s00167-021-06472-4
Oussedik S, Abdel MP, Victor J, Pagnano MW, Haddad FS (2020) Alignment in total knee arthroplasty. Bone Joint J 102-B(3):276–279. https://doi.org/10.1302/0301-620X.102B3.BJJ-2019-1729
Mercuri JJ, Pepper AM, Werner JA, Vigdorchik JM (2019) Gap balancing, measured resection, and kinematic alignment: how, when, and why? JBJS Rev 7:e2–e2. https://doi.org/10.2106/JBJS.RVW.18.00026
Agarwal N, To K, McDonnell S, Khan W (2020) Clinical and radiological outcomes in robotic-assisted total knee arthroplasty: a systematic review and meta-analysis. J Arthroplasty 35:3393-3409.e2. https://doi.org/10.1016/j.arth.2020.03.005
Chen AF, Kazarian GS, Jessop GW, Makhdom A (2018) Robotic technology in orthopaedic surgery. J Bone Joint Surg 100:1984–1992. https://doi.org/10.2106/JBJS.17.01397
Kayani B, Konan S, Ayuob A et al (2019) Robotic technology in total knee arthroplasty: a systematic review. EFORT Open Reviews 4:611–617. https://doi.org/10.1302/2058-5241.4.190022
Batailler C, Hannouche D, Benazzo F, Parratte S (2021) Concepts and techniques of a new robotically assisted technique for total knee arthroplasty: the ROSA knee system. Arch Orthop Trauma Surg 141:2049–2058. https://doi.org/10.1007/s00402-021-04048-y
Parratte S, Price AJ, Jeys LM et al (2019) Accuracy of a new robotically assisted technique for total knee arthroplasty: a cadaveric study. J Arthroplasty 34:2799–2803. https://doi.org/10.1016/j.arth.2019.06.040
Vermue H, Batailler C, Monk P et al (2022) The evolution of robotic systems for total knee arthroplasty, each system must be assessed for its own value: a systematic review of clinical evidence and meta-analysis. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04632-w
Collins K, Agius PA, Fraval A, Petterwood J (2022) Initial experience with the NAVIO robotic-assisted total knee replacement—coronal alignment accuracy and the learning curve. J Knee Surg 35:1295–1300. https://doi.org/10.1055/s-0040-1722693
Knapp PW, Nett MP, Scuderi GR (2022) Optimizing total knee arthroplasty with ROSA® robotic technology. Surg Technol Int 40:289–296. https://doi.org/10.52198/22.STI.40.OS1522
Rossi SMP, Ivone A, Ghiara M et al (2021) A ligament tensor-guided extramedullary alignment technique for distal femoral cut in total knee replacement: results at a minimum 3 years follow-up. Arch Orthop Trauma Surg 141:2295–2302. https://doi.org/10.1007/s00402-021-04115-4
Vanlommel L, Neven E, Anderson MB et al (2021) The initial learning curve for the ROSA® Knee System can be achieved in 6–11 cases for operative time and has similar 90-day complication rates with improved implant alignment compared to manual instrumentation in total knee arthroplasty. J Exp Ortop 8:119. https://doi.org/10.1186/s40634-021-00438-8
Bolam SM, Tay ML, Zaidi F et al (2022) Introduction of ROSA robotic-arm system for total knee arthroplasty is associated with a minimal learning curve for operative time. J Exp Ortop 9:86. https://doi.org/10.1186/s40634-022-00524-5
Haffar A, Krueger CA (2022) Goh, Lonner GS Total knee arthroplasty with robotic surgical assistance results in less physician stress and strain than conventional methods. J Arthroplasty 37(6S):S193–S200. https://doi.org/10.1016/j.arth.2021.11.021. (Epub 2022 Feb 17)
Charette RS, Sarpong NO, Weiner TR, Shah RP, Cooper HJ (2022) Registration of bony landmarks and soft tissue laxity during robotic total knee arthroplasty is highly reproducible. Surg Technol Int 41:sti41/1633. https://doi.org/10.52198/22.STI.41.OS1633
Rossi SMP, Sangaletti R, Perticarini L et al (2022) High accuracy of a new robotically assisted technique for total knee arthroplasty: an in vivo study. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06800-8
Shin C, Crovetti C, Huo E, Lionberger D (2022) Unsatisfactory accuracy of recent robotic assisting system ROSA for total knee arthroplasty. J EXP ORTOP 9:82. https://doi.org/10.1186/s40634-022-00522-7
Mancino F, Rossi SMP, Sangaletti R et al (2022) A new robotically assisted technique can improve outcomes of total knee arthroplasty comparing to an imageless navigation system. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04560-9
Batailler C, Anderson MB, Flecher X, Ollivier M, Parratte S (2022) Is sequential bilateral robotic total knee arthroplasty a safe procedure? A matched comparative pilot study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04455-9
Parratte S, Van Overschelde P, Bandi M et al (2022) An anatomo-functional implant positioning technique with robotic assistance for primary TKA allows the restoration of the native knee alignment and a natural functional ligament pattern, with a faster recovery at 6 months compared to an adjusted mechanical technique. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-022-06995-4
Kenanidis E, Paparoidamis G, Milonakis N et al (2022) Comparative outcomes between a new robotically assisted and a manual technique for total knee arthroplasty in patients with osteoarthritis: a prospective matched comparative cohort study. Eur J Orthop Surg Traumatol. https://doi.org/10.1007/s00590-022-03274-3
Acknowledgements
None
Funding
None.
Author information
Authors and Affiliations
Contributions
SMPR and FB designed and were responsible for the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
None.
Consent to participate
None. No need for IRB approval for the current study.
Conflict of interest
Francesco Benazzo is Consultant for Zimmer Biomet and Limacorporate. Grants from Limacorporate; Royalties from Zimmer Biomet and Limacorporate. Stefano Marco Paolo Rossi have no disclosures. Prof. Francesco Benazzo declares a teaching contract with the manufacturer (Zimmer Biomet). No other conflict of interest to be declared by any of the authors for the current study.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rossi, S.M.P., Benazzo, F. Individualized alignment and ligament balancing technique with the ROSA® robotic system for total knee arthroplasty. International Orthopaedics (SICOT) 47, 755–762 (2023). https://doi.org/10.1007/s00264-022-05671-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-022-05671-z