Abstract
Purpose
Double level osteotomy (DLO) (femoral and tibial) is a technically demanding procedure for which pre-operative planning accuracy and intraoperative correction are key factors. The aim of this study was to assess the accuracy of the achieved correction using patient-specific cutting guides (PSCGs) compared to the planned correction, its ability to maintain joint line obliquity (JLO), and to evaluate clinical outcomes and level of patient satisfaction at a follow-up of two years.
Methods
A single-centre, prospective observational study including 22 patients who underwent DLO by PSCGs between 2014 and 2018 was performed. Post-operative alignment was evaluated and compared with the target angular values to define the accuracy of the correction for the hip-knee-ankle angle (ΔHKA), medial proximal tibial angle (ΔMPTA), lateral distal femoral angle (ΔLDFA), and posterior proximal tibial angle (ΔPPTA). Pre- and post-operative JLO was also evaluated. At two year follow-up, changes in the KOOS sub-scores and patient satisfaction were recorded. The Mann–Whitney U test with 95% confidence interval (95% CI) was used to evaluate the differences between two variables; the paired Student’s t test was used to estimate evolution of functional outcomes.
Results
The mean ΔHKA was 1.3 ± 0.5°; the mean ΔMPTA was 0.98 ± 0.3°; the mean ΔLDFA was 0.94 ± 0.2°; ΔPPTA was 0.45 ± 0.4°. The orientation of the joint line was preserved with a mean difference in the JLO of 0.4 ± 0.2. At last follow-up, it was recorded a significant improvement in all KOOS scores, and 19 patients were enthusiastic, two satisfied, and one moderately satisfied.
Conclusion
Performing a DLO using PSCGs produces an accurate correction, without modification of the joint line orientation and with good functional outcomes at two year follow-up
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteotomies around the knee represent an ideal joint preserving procedures for the treatment of early tibiofemoral osteoarthritis [1, 2] with extra-articular deformities [3, 4]. When correcting large deformities in a single bone (tibia or femur), surgeons exposed them to the risk of creating abnormal joint line obliquity (JLO), which can compromise post-operative outcomes [5].
Double level osteotomy (DLO) (femoral and tibial) is a technically demanding procedure for which pre-operative planning accuracy and intraoperative correction is a key factor for achieving a corrected lower limb alignment [6, 7]. The accuracy has been improved by the introduction of three-dimensional (3D) pre-operative assessment systems [8], assisted surgery techniques such as computer-assisted surgery [5], and 3D patient-specific cutting guides (PSCGs) [9, 10].
The recent introduction of PSCGs using pre-operative computed tomography (CT) scan templating has raised the possibility of making instrumentation specific to each patient, which in turn could result in a more accurate correction of the bony misalignment with a decrease in operative time compared with conventional techniques during single level osteotomy procedure [11,12,13].
There are, however, potential difficulties when performing a DLO using PSCGs. One example is the inability to adapt the planned correction intraoperatively. The accuracy may also be compromised owing to the fact that the procedure requires a perfect match between the planned correction, the guide for the femoral correction, and the guide for the tibial correction [14, 15] compared to a single level correction which simply requires a single accurate PSCG [16].
To date, little has been published on the results and accuracy of DLO procedure using PSCGs. The aim of our study was to evaluate the accuracy of the achieved correction using PSCGs compared to the planned correction and its ability to maintain JLO in patients who suffered from knee pain, who had never undergone knee surgeries, in a context of important varus alignment with both tibial and femoral deformity. The second objective was to evaluate clinical outcomes and level of patient satisfaction at a follow-up of two years.
The hypothesis was that performing a DLO using PSCGs results in an accurate correction, similar to that seen in single level corrections, without adversely affecting the JLO (with an acceptable increase of JLO < 2°) and achieves satisfactory patient-reported functional outcomes at two year follow-up.
Material and methods
Population
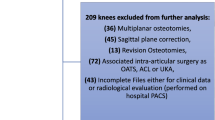
All patients undergoing a DLO using PSCGs between February 2014 and November 2018 were enrolled in this single-centre, prospective continuous cohort, observational study. Indication for DLO included patients aged under 65 years old with important knee pain and isolated medial knee osteoarthritis (Ahlbäck ≤ 3), a preserved status of the patellofemoral and lateral tibiofemoral joints assessed using clinical and radiological examination, a stable knee in the sagittal and coronal planes, a significant varus alignment (hip-knee-ankle angle (HKA) ≤ 170°) with concomitant tibial and femoral varus deformity (medial proximal tibial angle (MPTA) < 85° and lateral distal femoral angle (LDFA) > 90°), and the failure of all non-surgical treatments. The exclusion criteria comprised of previous ipsilateral knee surgery and hardware or bony abnormalities that would interfere with obtaining a high-quality CT scan.
Twenty-three patients met the inclusion and exclusion criteria, 1 patient was lost to follow-up, and finally twenty-two patients (19 men and 3 women) were included in this study. Minimum follow-up was 24 months.
Patient consent was collected pre-operatively after they were informed of the procedure in accordance with the principles of the Declaration of Helsinki. Local Ethical Committee approval was obtained prior to study initiation.
Pre-operative planning
In the pre-operative planning stage, the planned correction was first calculated by the surgeon using conventional radiographs (calibrated weight-bearing long-leg, A/P, and lateral views). Subsequently, all patients underwent a CT scan. The CT scan protocol consisted of acquiring images centered on the femoral head, the knee (allowing the distal femur and 15 cm of the proximal tibia to be captured), and over the ankle. The slice thickness was 0.625 mm for the knee and 2 mm for the hip and ankle (GE Light Speed VCT64). The surgeon took measurements and filled out an order form for the engineer which specified the correction objectives in the frontal and sagittal planes through variations in the HKA, MPTA, LDFA, and posterior proximal tibial angle (PPTA). Pre-operative angles are summarized in the Table 1. Joint orientation was also evaluated by measuring the joint line obliquity (JLO) and joint line convergence angle (JLCA) to assess soft tissue laxity. As there was no sagittal femoral correction planned, the posterior distal femoral angle was not considered.
Tibial and femoral osteotomy models were used to virtually position PSCGs (Fig. 1) and Activmotion plates (Newclip Technics®, Haute-Goulaine, France) both on the tibia and the femur using the protocol defined by the manufacturer. The PSCG design takes into account the resection plane and the position of the screw tunnels relative to the virtual positioning of the plates. The objective behind PSCGs is to define the optimal plate position after osteotomy correction and then to transfer this anatomical position to the pre-osteotomy guide position. When the final plate’s position fits the drill holes using the PSCG, the osteotomy is performed according to the pre-operative plan.
Surgical technique
All surgical procedures followed the same surgical steps, starting off with the distal femoral closing wedge osteotomy [14]. The distal femoral lateral surface was exposed, and the anatomical cutting guide was positioned. When an optimal position was confirmed by fluoroscopy, the guide was secured to the bone by four to seven pins. Additional pins (cutting and hinge pins) were positioned to secure the osteotomy cutting plane. The nine holes required for the plate were pre-drilled prior to performing the osteotomy. The valgus femoral osteotomy was then performed with the PSCG in place; the saw blade was guided utilizing a specific slotted capture. Next, the distal part of the PSCG was removed, and a closing wedge (with a 4–5 mm lateral base) was removed to complete the osteotomy. The plate was secured using nine screws, the sizes of which were pre-determined during the pre-operative planning.
The second stage consisted of performing the opening wedge high tibial osteotomy following a previously published method [15, 17]. The medial aspect of proximal tibia was exposed. The eight holes needed for the plate were pre-drilled prior to performing the osteotomy. The osteotomy was then performed with the PSCG in place, and the proximal portion of the modular cutting guide was removed to finish the osteotomy in a single plane or two planes. This step was dependent on the planned correction and the position of the patellar tendon. The osteotomy was then gradually opened/distracted with a laminar spreader until the pre-drilled screw holes were aligned with the holes in the plate. The bone defect was left empty or filled with a femoral head wedge allograft.
Post-operative management
Weight-bearing was not allowed for the first three weeks. Then, progressive partial weight-bearing with the aid of two crutches was commenced after three weeks to reach a full weight-bearing after six weeks. Range of motion was not restricted during the rehabilitation phase. All patients received thromboprophylaxis with low molecular weight heparin pre- and post-operatively for 45 days.
After surgery, patients were reviewed at one, three, six, 12, and 24 months for regular follow-up with radiographs (long-leg standing (Fig. 2), A/P, and lateral) and KOOS score evaluation. Femoral and tibial bone union were systematically assessed by radiological evaluation at one, three, six, 12, and 24 months: the bone repair process was considered complete when there was continuity in three out of four cortices in anterior and lateral projections (both femoral and tibial) after five months; delayed between five and eight months, and not completed (non-union) after eight months [18]. Post-operative alignment was evaluated and compared with the target angular values, by two independent observers, to define the correction accuracy. We reported an intraclass correlation coefficient (ICC) of 0.79, 0.81, 0.87, and 0.85 for the Δ values (ΔHKA, ΔMPTA, ΔPPTA, ΔLDFA, respectively) and an ICC of 0.80 and 0.82 for JLO and JLCA measurements. For all angular values both in the sagittal and coronal planes, the goal was to obtain a perfect coincidence between the planned and the obtained angular values (delta = 0) with a degree of tolerance of 2°.
Changes in the KOOS sub-scores were recorded, comparing pre-operative to the 24-month assessment: ΔKOOS pain, ΔKOOS symptoms, ΔKOOS ADL, ΔKOOS sport/rec, and ΔKOOS QOL were defined this way. The ability to return to work and sport was also recorded. At 24-month follow-up, patient satisfaction was ranked upon five item questionnaires (disappointed, not-satisfied, moderately satisfied, satisfied, and enthusiastic).
Statistical analysis
Statistical analyses were performed with use of SSPS software (IBM; Armonk, NY). Means and standard deviations (SDs) were determined for each of the measured and desired anatomic parameters. Normal (Gaussian) distributions was verified to determine adequate statistical testing method (either parametric or non-parametric) to estimate difference between pre-operative, planned, and post-operative parameters groups in an univariate analysis. The Mann–Whitney U test for two independent samples with 95% confidence interval (95% CI) was used to evaluate the differences between two variables; the paired Student’s t test was used to estimate evolution of functional outcomes during follow-up. Following the data collection, the statistical power was checked. Using the Δ angular corrections (planned corrections-obtained corrections) as a primary parameter with 80% of power, Alpha 0.05, and a value of Δ < 3.0°, it was estimated that the sample size should be 14. Therefore, the sample size of 22 in the present study is reasonable in terms of statistical power.
Results
Correction accuracy and radiographic results
The mean ΔHKA was 1.3 ± 1.5 (p = 0.12); the mean ΔMPTA was 0.98 ± 1.3 (p = 0.09); the mean ΔLDFA was 0.94 ± 1.2 (p = 0.09); ΔPPTA was 1.05 ± 1.4 (p = 0.2). For all the radiographic parameters, there were no statistically significant differences between the target values and the post-operative values (Table 2). A mean pre-operative JLO of 1.4 ± 1.2° and a mean post-operative JLO of 0.9 ± 1.2° were observed; thus, the orientation of the joint line was preserved with a mean difference in the JLO of 0.5 ± 0.90.
Mean consolidation time at radiographic control was 4.4 ± 1.8 months for the femur and 5.1 ± 1.5 months for the tibia. No case of non-union was reported.
Functional outcomes
At final follow-up assessment, 24 months after surgery, an improvement of 37 ± 16 for the KOOS pain (5–75), 37 ± 25 for the KOOS symptoms (2–82), 37 ± 32 for the KOOS ADL (4–92), 34 ± 37 for the KOOS sport/rec (2–87), and 3625 for the KOOS QOL (7–73) (p < 0.0001) (Table 2) were observed. The mean time to return to work and sports were 4.0 ± 1.6 (3–12) and 4.9 ± 1.2 (2–7) months, respectively. At 24-month follow-up, 19 patients were enthusiastic, two satisfied, and one moderately satisfied.
Complications
One minor complication (post-operative hematoma) and one major complication (deep wound infection) were observed in the cohort. No revisions to total knee arthroplasty or unicompartmental knee arthroplasty were observed at 24-month follow-up.
Discussion
The main finding of this study was that performing a DLO with PSCG is an accurate procedure and preserves pre-operative joint line orientation. The results for achieving desired corrective accuracy are in keeping with those previously published for both single femoral and tibial osteotomies. Good functional outcomes at two year follow-up were observed in this cohort.
Conventional DLOs are highly demanding procedures and require a protracted learning curve. In 1969, Benjamin et al. [19] was the first to report a series of 57 DLO with indications of rheumatoid osteoarthritis and osteoarthritis. In this series, he reported a good level of patient satisfaction despite some complications including limited range of motion and six patients without reduced pain. Analyses of the pre-operative deformity and the post-operative correction (HKA angle or JLO) were not mentioned. Babis et al. [20] reported on 24 patients (29 knees) operated on utilizing a conventional technique. A computer-aided analysis of the mechanical status of the knee was used for pre-operative planning. Their results showed a mean post-operative HKA angle of 176.9° (169.4–184.9°) with a residual varus in two cases (4.6–4.9°) and an over correction of more than 4° in ten cases and more than 6° in five. No information was available concerning the pre-operative and post-operative JLO.
Otherwise, a high level of post-operative alignment accuracy was reached in computer-assisted procedures despite their cost and increased surgical time [21, 22]. Saragaglia [23] reported a case series of 38 patients in which the pre-operative target was reached in 92.7% of patients for HKA and 88.1% for MPTA with 2° of accuracy. No information was reported concerning the pre-operative and post-operative JLO. The results of the present study are comparable with those of Saragaglia. Our study demonstrates that pre-operative targets were reached in all the patients with a slight difference between the planned correction and the post-operative values, which were not statistically significant and always within the gap of 2° of discrepancy. A lower accuracy in the correction was observed for the HKA angle compared to other parameters. This angle is influenced by both the bony and soft tissue status [24]. This is accounted for the joint line convergence angle (JLCA). HKA measurements include JLCA values; therefore, it is important to assess the accuracy of the system by evaluating only direct bone corrections (MPTA, mLDFA, and PPTA).
Previous studies have analyzed the accuracy of the PSCG system but have been restricted to single level knee osteotomy [25]. Nevertheless, a high level of precision has been demonstrated in single level osteotomies. Cerciello et al. in a systematic review analyzed 28 studies which focused on single level osteotomies performed by computer navigation and patient-specific instrumentation. In their conclusions, they stated that it had been observed a reduced rate of post-operative outliers for PSI-instrumented osteotomies compared to conventional techniques [26, 27]. Specific accuracy correction results of open-wedge high tibial osteotomy procedures using PSCGs have been published by Chaouche et al. [15]. They observed that the mean ΔHKA was 1 ± 0.95°, the mean ΔMPTA was 0.54 ± 0.63°, and the mean ΔPPTA was 0.43 ± 0.8°. In all cases, the discrepancy between planned and achieved correction was less than or equal to 2°. Similar results were published in distal femoral osteotomies using PSCGs by Jacquet et al. [14]. The HKA target was also reached in 100% of case with 2° of discrepancy. Finally, the correction accuracy observed in the present study was similar to those previously described for both femoral and tibial single level osteotomies using PSCGs.
Double level osteotomies have been introduced to avoid joint line obliquity [28, 29]. Nakayama et al. reported that a JLO > 5° (medial proximal tibial angle of 95°) determines detrimental stress to the articular cartilage, so they proposed that DLO should be indicated for varus knees with a pre-operatively anticipated MPTA of > 95 [30]. Our study highlights the benefits of this technique [31], with preservation of the joint line orientation in cases where there is extra-articular varus deformity arising from both the tibia and femur. An acceptable difference of 2°, as recommended by most studies, was found in this study [30, 32].
Finally, the second main outcome was to investigate clinical results at 24-month follow-up. A consistent improvement in all sub-categories of the KOOS score was observed, and 86.6% of patients were enthusiastic regarding the results of their surgery. Comparing these clinical results to previously published DLO results, they were comparable [23] or even superior [33].
The present retrospective study has several limitations. Firstly, this is a non-comparative study; even if data exist on the accuracy and recurrence of JLO in conventional techniques, a control group of conventional DLO would have been interesting for doing a direct comparison. Secondly, the surgeons who performed these procedures were familiar with osteotomy surgeries and had already used PSCGs during femoral or tibial single level osteotomies. Their results may not be directly transferrable to other less experienced surgeons. Thirdly, follow-up time was limited to two years following surgery, and so long-term data on functional outcomes, revision rates, and total knee arthroplasty conversion rates were not available.
Conclusion
Performing a DLO using PSCGs produces an accurate correction, without modification of the joint line orientation and with good functional outcomes at two year follow-up. The use of PSCGs in the execution of DLOs guarantees very high levels of precision comparable to those obtained through the use of the same instrumentation for single level osteotomies. Therefore, it represents a useful tool in the hands of surgeons with less experience in this complex surgery, with the assumption of correct planning and adequate indications.
Availability of data and material
Copy of the initial spreadsheet kept available.
References
Conventry MB (2001) Osteotomy of the upper portion of the tibia for degenerative arthritis of the knee. A preliminary report by Mark B. Conventry, MD. From the Section of Orthopedic Surgery, Mayo Clinic and Mayo Foundation, Rochester, Minnesota. 1965. J Bone Joint Surg Am 83:1426
Ferner F, Lutter C, Dickschas J, Strecker W (2019) Medial open wedge vs. lateral closed wedge high tibial osteotomy - indications based on the findings of patellar height, leg length, torsional correction and clinical outcome in one hundred cases. Int Orthop 43:1379–1386. https://doi.org/10.1007/s00264-018-4155-9
Amendola A, Bonasia DE (2010) Results of high tibial osteotomy: review of the literature. Int Orthop 34:155–160. https://doi.org/10.1007/s00264-009-0889-8
Seil R, van Heerwaarden R, Lobenhoffer P, Kohn D (2013) The rapid evolution of knee osteotomies. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 21:1–2. https://doi.org/10.1007/s00167-012-2175-3
Saragaglia D, Chedal-Bornu B, Rouchy RC et al (2016) Role of computer-assisted surgery in osteotomies around the knee. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:3387–3395. https://doi.org/10.1007/s00167-016-4302-z
Sharma L, Song J, Felson DT et al (2001) The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 286:188–195. https://doi.org/10.1001/jama.286.2.188
Dugdale TW, Noyes FR, Styer D (1992) Preoperative planning for high tibial osteotomy. The effect of lateral tibiofemoral separation and tibiofemoral length. Clin Orthop 248–264
Sailhan F, Jacob L, Hamadouche M (2017) Differences in limb alignment and femoral mechanical-anatomical angles using two dimension versus three dimension radiographic imaging. Int Orthop 41:2009–2016. https://doi.org/10.1007/s00264-017-3428-z
Donnez M, Ollivier M, Munier M et al (2018) Are three-dimensional patient-specific cutting guides for open wedge high tibial osteotomy accurate? An in vitro study. J Orthop Surg 13:171. https://doi.org/10.1186/s13018-018-0872-4
Ke S, Ran T, He Y et al (2020) Does patient-specific instrumentation increase the risk of notching in the anterior femoral cortex in total knee arthroplasty? A comparative prospective trial. Int Orthop 44:2603–2611. https://doi.org/10.1007/s00264-020-04779-4
Thienpont E, Schwab PE, Fennema P (2014) A systematic review and meta-analysis of patient-specific instrumentation for improving alignment of the components in total knee replacement. Bone Jt J 96-B:1052–1061. https://doi.org/10.1302/0301-620X.96B8.33747
Haglin JM, Eltorai AEM, Gil JA et al (2016) Patient-specific orthopaedic implants. Orthop Surg 8:417–424. https://doi.org/10.1111/os.12282
Jacquet C, Sharma A, Fabre M et al (2019) Patient-specific high-tibial osteotomy’s “cutting-guides” decrease operating time and the number of fluoroscopic images taken after a Brief Learning Curve. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. https://doi.org/10.1007/s00167-019-05637-6
Jacquet C, Chan-Yu-Kin J, Sharma A et al (2019) "More accurate correction using “patient-specific” cutting guides in opening wedge distal femur varization osteotomies. Int Orthop 43:2285–2291. https://doi.org/10.1007/s00264-018-4207-1
Chaouche S, Jacquet C, Fabre-Aubrespy M et al (2019) Patient-specific cutting guides for open-wedge high tibial osteotomy: safety and accuracy analysis of a hundred patients continuous cohort. Int Orthop 43:2757–2765. https://doi.org/10.1007/s00264-019-04372-4
Gómez-Palomo JM, Meschian-Coretti S, Esteban-Castillo JL et al (2020) Double level osteotomy assisted by 3D printing technology in a patient with blount disease: a case report. JBJS Case Connect 10:e0477. https://doi.org/10.2106/JBJS.CC.19.00477
Munier M, Donnez M, Ollivier M et al (2017) Can three-dimensional patient-specific cutting guides be used to achieve optimal correction for high tibial osteotomy? Pilot study. Orthop Traumatol Surg Res OTSR 103:245–250. https://doi.org/10.1016/j.otsr.2016.11.020
Dijkman BG, Sprague S, Schemitsch EH, Bhandari M (2010) When is a fracture healed? Radiographic and clinical criteria revisited. J Orthop Trauma 24(Suppl 1):S76-80. https://doi.org/10.1097/BOT.0b013e3181ca3f97
Benjamin A (1969) Double osteotomy for the painful knee in rheumatoid arthritis and osteoarthritis. J Bone Joint Surg Br 51:694–699
Babis GC, An K-N, Chao EYS et al (2002) Double level osteotomy of the knee: a method to retain joint-line obliquity. Clinical results. J Bone Joint Surg Am 84:1380–1388. https://doi.org/10.2106/00004623-200208000-00013
Saragaglia D, Roberts J (2005) Navigated osteotomies around the knee in 170 patients with osteoarthritis secondary to genu varum. Orthopedics 28:s1269-1274
Maurer F, Wassmer G (2006) High tibial osteotomy: does navigation improve results? Orthopedics 29:S130-132
Saragaglia D, Blaysat M, Mercier N, Grimaldi M (2012) Results of forty two computer-assisted double level osteotomies for severe genu varum deformity. Int Orthop 36:999–1003. https://doi.org/10.1007/s00264-011-1363-y
Lee D-H, Park S-C, Park H-J, Han S-B (2016) Effect of soft tissue laxity of the knee joint on limb alignment correction in open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 24:3704–3712. https://doi.org/10.1007/s00167-015-3682-9
Predescu V, Grosu A-M, Gherman I et al (2021) Early experience using patient-specific instrumentation in opening wedge high tibial osteotomy. Int Orthop. https://doi.org/10.1007/s00264-021-04964-z
Pérez-Mañanes R, Burró JA, Manaute JR et al (2016) 3D surgical printing cutting guides for open-wedge high tibial osteotomy: do it yourself. J Knee Surg 29:690–695. https://doi.org/10.1055/s-0036-1572412
Cerciello S, Ollivier M, Corona K et al (2020) CAS and PSI increase coronal alignment accuracy and reduce outliers when compared to traditional technique of medial open wedge high tibial osteotomy: a meta-analysis. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. https://doi.org/10.1007/s00167-020-06253-5
Schröter S, Nakayama H, Yoshiya S et al (2019) Development of the double level osteotomy in severe varus osteoarthritis showed good outcome by preventing oblique joint line. Arch Orthop Trauma Surg 139:519–527. https://doi.org/10.1007/s00402-018-3068-9
Micicoi G, Grasso F, Kley K, et al (2021) Osteotomy around the knee is planned toward an anatomical bone correction in less than half of patients. Orthop Traumatol Surg Res OTSR 102897. https://doi.org/10.1016/j.otsr.2021.102897
Nakayama H, Schröter S, Yamamoto C et al (2018) Large correction in opening wedge high tibial osteotomy with resultant joint-line obliquity induces excessive shear stress on the articular cartilage. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 26:1873–1878. https://doi.org/10.1007/s00167-017-4680-x
Akamatsu Y, Nejima S, Tsuji M et al (2021) Joint line obliquity was maintained after double-level osteotomy, but was increased after open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. https://doi.org/10.1007/s00167-020-06430-6
Song J-H, Bin S-I, Kim J-M, Lee B-S (2020) What is an acceptable limit of joint-line obliquity after medial open wedge high tibial osteotomy? Analysis based on midterm results. Am J Sports Med 48:3028–3035. https://doi.org/10.1177/0363546520949552
Nakayama H, Iseki T, Kanto R et al (2020) Physiologic knee joint alignment and orientation can be restored by the minimally invasive double level osteotomy for osteoarthritic knees with severe varus deformity. Knee Surg Sports Traumatol Arthrosc Off J ESSKA 28:742–750. https://doi.org/10.1007/s00167-018-5103-3
Author information
Authors and Affiliations
Contributions
MO, LH, and CJ designed the protocol. MO, LH, and KK gathered the patients’ data anonymously. FG, KK, and RK performed database analysis. CJ, MO, and FG wrote the initial draft. MO, CJ, FG, KK, RK, GM, and PM edited the different version of the draft. MO, CJ, FG, KK, RK, LH, GM, and PM approved the submitted and final versions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate and to publish
Patient consent was collected pre-operatively after they were informed of the procedure in accordance with the principles of the Declaration of Helsinki. Local Ethical Committee approval was obtained prior to study’s initiation (Comité Informatique et Liberté (CIL)/Assistance Publique des Hopitaux de Marseille (AP-HM)/Registration Number 2019–127)).
Conflict of interest
MO is educational consultant for New-Clip, Stryker, and Arthrex. KK is educational consultant for New-Clip. CJ, RK, FG, PM, GM, and LH have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Grasso, F., Martz, P., Micicoi, G. et al. Double level knee osteotomy using patient-specific cutting guides is accurate and provides satisfactory clinical results: a prospective analysis of a cohort of twenty-two continuous patients. International Orthopaedics (SICOT) 46, 473–479 (2022). https://doi.org/10.1007/s00264-021-05194-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-021-05194-z