Abstract
Purpose
This systematic review aimed to compare radiographic correction, clinical outcomes, complications, and re-operations between lateral column lengthening (LCL) and arthroereisis (AR) for treating symptomatic flatfoot in children.
Methods
We conducted a comprehensive search on MEDLINE, EMBASE, and Cochrane Library databases. Literature search, data extraction, and quality assessment were conducted by two independent reviewers. The outcomes analyzed included radiographic parameters, clinical scores, satisfaction, complications, and re-operations.
Results
Twenty-one and 13 studies were included in the LCL and AR groups, respectively. The change in anteroposterior talo-first metatarsal angle was greater in the LCL (9.5° to 21.7°) than in the AR group (10.6° to 12.8°). The change in calcaneal pitch was greater in the LCL (2.1° to 26.53°) than in the AR group (− 1.3° to 3.23°). Improvements in the American Orthopedic Foot and Ankle Society (AOFAS) ankle–hindfoot score were greater in the LCL (27.7 to 39.1) than in the AR group (17 to 22). The percentage of satisfaction was similar between the LCL (68% to 89%) and AR (78.5% to 96.4%) groups. The complication rate was higher in the LCL (0% to 86.9%) than in the AR group (3.5% to 45%). The most common complications were calcaneocuboid subluxation and persistent pain in the LCL and AR groups, respectively. The re-operation rate was similar between the LCL (0% to 27.3%) and AR (0% to 36.4%) groups.
Conclusions
The LCL group has achieved more radiographic corrections and more improvements in the AOFAS score than the AR group. Complications were more common in the LCL group than in the AR group, and the re-operation rates were similar between the two groups.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Flatfoot deformity is a common reason for referral of children to an orthopaedic surgeon, with a prevalence of 15–45% in children [1]. Most children with flatfoot deformity will undergo spontaneous correction or become asymptomatic [2, 3]. Most symptoms if present resolve with conservative treatment [4]. Surgery is indicated if pain is persistent despite conservative treatment. Multiple surgical options to treat symptomatic flatfoot have been described [5].
Evans [6] first introduced the concept of lateral column lengthening (LCL) in 1975, and Mosca [7] had modified and further popularized it. LCL has been reported to produce good results, and it has become the mainstay of surgical options to treat symptomatic flexible flatfoot deformity. However, disadvantages, such as insufficient corrections, overcorrections, loss of correction due to inadequate graft size, graft migration, or malposition, have been reported [8, 9].
Subtalar arthroereisis (AR), which is performed by placing an implant within the sinus tarsi to restrict excessive subtalar eversion, is also a common surgical procedure to treat symptomatic flexible flatfoot deformities. This procedure became popular because it is minimally invasive and allows early weight-bearing capacity and a relatively rapid return to play and sports [10]. However, outcomes of the procedure have been poorly studied, and the indications of the procedure have not been established because of insufficient evidence [1]. The complication rate has been reported to be up to 40%, and common complications include overcorrection and undercorrection, inflammatory synovitis, sinus tarsi pain, cortical erosion, talar avascular necrosis, and calcaneus fractures [11,12,13].
Although both LCL and AR are popular surgical options to treat symptomatic flexible flatfoot deformity, high-quality evidence-based studies, such as level 1 or 2 studies, that compare these two procedures are lacking. We could find only one study, a prospective comparative study [4], directly comparing the two procedures, and it showed no difference in the outcomes.
The present study aimed to perform a systematic review to compare radiographic correction, clinical scores, patient satisfaction, complications, and reoperations between LCL and AR as treatment for symptomatic flatfoot in children.
Materials and methods
Data and literature sources
Multiple comprehensive databases, including PubMed/MEDLINE, EMBASE, and Cochrane Library databases, were searched to identify studies that pertain to LCL and AR as treatment for paediatric flatfoot deformity. This study was based on the Preferred Reporting Items for Systematic Reviews and Meta-analyses guidelines [14]. The following keywords and MeSH terms were included in our searches: flatfoot, planovalgus, calcaneal lengthening osteotomy, LCL, AR, pediatric, and child. After the initial electronic search, additional manual searches were conducted using the bibliographies of all selected full-text articles.
Study selection
Two authors independently decided the inclusion of all studies in accordance with the selection criteria. For study selection, the titles and abstracts of the identified studies were screened first, and then the selected studies were scanned by full text. Studies were eligible for inclusion if they met the following criteria: (1) levels I to IV clinical studies of pediatric flatfoot; (2) either LCL or AR; (3) studies including clinical and/or radiological outcome; (4) English language. The exclusion criteria were as follows: (1) studies including adult flatfoot; (2) nonclinical (e.g., cadaver or biomechanical) studies; (3) studies not reporting clinical or radiological outcomes; (4) LCL combined with medial displacement calcaneal osteotomy or triple arthrodesis; (5) LCL combined with AR; (6) review or meta-analysis articles, case reports, technique articles, and letters to the editor; and (7) non-English language.
Literature search
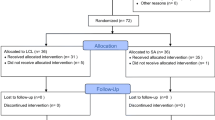
Database searches yielded 410 articles. After removing duplicate entries, 267 articles were identified, of which 61 were potentially eligible based on their title and abstract. After we assessed the eligibility based on the full manuscript, 28 articles were excluded. Finally, 33 studies were included in our systematic review (Fig. 1), including 1, 1, 8, and 23 level I, II, III, and IV studies, respectively (Tables 1 and 2). Among comparative studies, only one level II study [4] directly compared the LCL group with the AR group.
Data extraction
Data extraction was conducted by two independent reviewers using a predefined data extraction form. Any discrepancies were arbitrated by consensus with a third reviewer. The included studies were divided into the LCL and AR groups. The LCL or AR cohort data were extracted from the comparative studies. Finally, 21 and 13 studies were included in the LCL and AR groups, respectively (Tables 1 and 2). Information extracted from each study included authors, publication date, number of patients, underlying diagnosis, age, sex, follow-up period, radiographic measurements, clinical scores, complications, and re-operations. Various radiographic parameters were used for evaluating radiographic correction in the included studies; hence, radiographic parameters were selected if they were reported in more than two studies in each group. The following six radiographic parameters were analyzed: anteroposterior talo-first metatarsal, lateral talo-first metatarsal, calcaneal pitch, anteroposterior talocalcaneal, lateral talocalcaneal, and talar declination angles. Satisfaction with surgery was assessed in the included studies based on the Mosca clinical criteria [7], a scoring system described by Yoo et al. [30], patients’ report, or authors’ own criteria. The percentage of cases with satisfactory outcome was calculated. Six kinds of clinical scores were used in ten studies. The American Orthopedic Foot and Ankle Society (AOFAS) ankle–hindfoot score [43] and the Oxford Ankle Foot Questionnaire for Children (OxAFQ) scores [44] were used in more than two studies in each group, whereas other scores were used only once in one study regardless of the groups. Complications included calcaneocuboid subluxation, implant migration, nonunion, delayed union, infection, wound problem, persistent pain, overcorrection and undercorrection, recurrence of planovalgus deformity, nerve injury, hardware prominence, graft failure, and iliac bone graft donor site problem. Re-operation was defined as any surgery performed after the index surgery.
Assessment of methodological quality
The Methodological Index for Nonrandomized Studies (MINORS) scale quantified the quality of the literature [45]. The global ideal MINORS scores for non-comparative and comparative studies are 16 and 24, respectively. Two independent reviewers scored each study, and any discrepancy between the reviewers was resolved by consensus with a third reviewer. The mean MINORS score and levels of evidence in both groups are presented in Table 3, and the quality of included studies was similar between the LCL and AR groups.
Statistical analysis
Most of the included studies were nonrandomized case series without a control group, and some studies were comparative studies. Therefore, a meta-analysis was considered inappropriate because the included studies had considerable heterogeneity. Thus, a qualitative synthesis without quantitative comparison between the LCL and AR groups was performed.
Results
Study demographics
Demographic data are presented in Table 1. In the LCL group, eight studies included patients with and without underlying neuromuscular diseases, five studies excluded patients with neuromuscular diseases, and eight studies included only a patient with cerebral palsy. In the AR group, three studies excluded patients with neuromuscular diseases, two studies included only patients with cerebral palsy, two studies included only patients with neuromuscular diseases, and six studies did not report underlying diagnoses.
We analyzed 1144 and 818 feet in 729 and 565 patients in the LCL and AR groups, respectively. The mean age ranged from 8.6 to 13.6 years and from 7.7 to 12.1 years in all included studies of the LCL group and in eight studies of the AR group, respectively. The remaining five studies in the AR group reported the age range (2–15 years) without the mean age. The mean follow-up period ranged from six months to 10.9 years in all included studies of the LCL group and 18.4 months to six years in 11 studies of the AR group. The remaining two studies of the AR group reported the range of the follow-up period (1–15 years) without the mean follow-up period.
Surgical procedures
In the LCL group, intra-calcaneal lengthening was performed in 17 studies [8, 15,16,17,18,19,20,21,22,23,24, 26,27,28,29,30, 46], and intra-calcaneal lengthening or calcaneocuboid distraction arthrodesis was conducted in four studies [4, 5, 25, 31]. The modified Evans osteotomy technique [6] was used for intra-calcaneal lengthening in most of the included studies. Bone graft was performed in 20 studies, and one study [26] did not state whether bone graft was performed. Only autograft and allograft were used in six [19,20,21,22,23, 27] and seven studies [4, 5, 16, 17, 24, 25, 28], respectively. Autograft or allograft, allograft or xenograft, and autograft or hydroxyapatite–tricalcium phosphate graft were used in five studies [8, 29,30,31, 46], one study [18], and one study [15], respectively. The graft was not fixed in five studies [4, 15,16,17, 19, 24], fixed in all patients in eight studies [20,21,22, 25, 27, 29, 30, 46], and fixed in some patients in seven studies [4, 5, 8, 18, 23, 28, 31]. One study [26] did not describe about graft fixation.
The devices for AR in the AR group were categorized as titanium, bioresorbable, stainless steel, silicone, polyethylene, or staple implants, which were used in five studies [4, 10, 33, 34, 36], one study [32], one study [37], four studies [35, 38, 39, 41], one study [40], and one study [42], respectively. Other simultaneous procedures were performed in most studies of both groups, except for one study [4, 15] in each group, and one study [28] in the LCL group did not describe about the simultaneous procedures. Additional procedures are presented in Table 4. The most common additional procedures were Achilles tendon lengthening or gastrocnemius recession; the next most common procedures were peroneus brevis or longus tendon lengthening which were performed in both groups.
Radiographic outcomes
Six radiographic parameters were analyzed, and the range of mean values is summarized in Table 5. All radiographic parameters improved after surgery in most of the included studies in both groups. However, one study [5] in the LCL group reported that the mean lateral talocalcaneal angle increased from 19° pre-operatively to 24° at follow-up, and four (25%) of the 16 feet had poor results because of recurrence of planovalgus foot deformity. In one study [4] in the AR group, the mean calcaneal pitch decreased from 13° pre-operatively to 11.7° at follow-up.
The LCL group had more improvements in the anteroposterior talo-first metatarsal angle. The change in the anteroposterior talo-first metatarsal angle ranged from 9.5° to 21.7° and from 10.6° to 12.8° in the LCL and AR groups, respectively. The change in the anteroposterior talo-first metatarsal angle in the LCL group was > 15° in 9 [17, 19, 21, 22, 24, 26, 28, 30, 46] of 16 included studies. The LCL group also had more improvements in the calcaneal pitch. The change in the calcaneal pitch ranged from 2.1° to 26.53° and from − 1.3° to 3.23° in the LCL and AR groups, respectively. As previously mentioned, one study [4] in the AR group reported that the calcaneal pitch decreased post-operatively.
Clinical outcomes
The AOFAS score and satisfaction are shown in Table 6. Eight and six studies in the LCL and AR groups, respectively, reported satisfaction with outcome. The percentage of satisfaction ranged from 68 to 89% and from 78.5 to 96.4% in the LCL and AR groups, respectively. Three and three studies in the LCL and AR groups reported AOFAS score, respectively. Improvements of the mean AOFAS score ranged from 27.7 to 39.1 and from 17 to 22 in the LCL and AR groups, respectively.
Three studies reported OxAFQ scores. First, the only available prospective comparative study [4] reported that both the LCL and AR groups showed improvements in their OxAFQ scores, but only the AR group achieved statistical significance. Two patients in the LCL group did not fill out preoperative Oxford questionnaires, which may be why the LCL group was unable to achieve statistical significance. The pre- and post-operative OxAFQ scores were not compared between the two groups. Second, Martinkevich et al. [15] compared structural hydroxyapatite–tricalcium phosphate graft to autologous iliac crest bone graft in calcaneal lengthening osteotomy. In this study, both groups showed comparable changes towards higher OxAFQ scores (improvement) in the physical function and footwear item at 6-month follow-up. Finally, one study [47] in the AR group noted a significant improvement in the mean OxAFQ scores in the “Emotional” and “Footwear” items for the children scale and in the “School and Play” and “Footwear” items for the parent scale.
Complications
Eighteen and 11 studies in the LCL and AR groups, respectively, contributed to the analysis of the complication rate (Table 7). The complication rates ranged from 0 to 86.9% and from 3.5 to 45% in the LCL and AR groups, respectively. The complication rates in the LCL group were > 50% in six studies [8, 15, 19, 25, 28, 46]. The most common complication in the LCL group was calcaneocuboid subluxation, followed by nonunion. The calcaneocuboid subluxation rate ranged from 0.8 to 86.9% in seven studies [8, 19, 20, 26, 28, 29, 46] and > 50% in four [8, 19, 28, 46] of seven studies. However, calcaneocuboid subluxation did not have an effect on the clinical score and did not lead to symptoms and osteoarthritic changes in the calcaneocuboid joint [8, 20, 46]. The nonunion rate in the LCL group was noted in four studies [5, 8, 16, 18], ranging from 3 to 13%. However, the nonunion rate ranged from 3 to 4.7% after excluding Andreacchio et al.’s study [5]. The nonunion rate was 13% in Andreacchio et al.’s study [5], and LCL was performed through intra-calcaneal lengthening or calcaneocuboid distraction arthrodesis. Nonunions developed only in patients with calcaneocuboid distraction arthrodesis, and all nonunions were asymptomatic with maintenance of the surgical correction.
Persistent pain and implant migration were the most frequently reported complications in the AR group. Eight studies [4, 10, 32, 33, 35, 36, 39, 40] in the AR group reported persistent pain, ranging from 0.7 to 36.4%, whereas only one study [25] in the LCL group reported persistent foot pain. Three studies [34, 35, 41] contributed to the analysis of the implant migration rate, and the implant was used differently in each study. The migration rate was 3.7%, 19.3%, and 2.6% in the studies using Kalix II (Integra LifeSciences, Plainsboro, NJ, USA) [34], Silastic plug [35], and Viladot implant [41], respectively. The complication rate based on the implant type ranged from 3.5 to 45% and from 3.7 to 15.4% in the old-type [35, 38,39,40,41] (silicone, polyethylene, and staple implants) and recent-type implants [4, 10, 32,33,34, 36] (titanium, bioresorbable, and stainless steel implants), respectively. Infection, wound problem, overcorrection, and undercorrection were reported in only the old-type implants.
Re-operation
Fifteen [4, 5, 8, 15,16,17,18,19,20, 23,24,25, 27, 29, 30] and twelve studies [4, 10, 32,33,34,35,36, 38,39,40,41,42] in the LCL and AR groups, respectively, reported re-operations. The re-operation rates ranged from 0 to 27.3% and from 0 to 36.4% in the LCL and AR groups, respectively (Table 8). Four studies [5, 24, 29, 30] in the LCL group reported that revision surgeries were performed for loss of correction, and one study [15] reported that revision surgeries were performed for deep infection. Hardware removals were performed in two studies [4, 25] because of hardware prominence or extrusion of the graft and staple. Implant removal in the AR group was performed in nine studies [4, 10, 33, 35, 36, 38,39,40,41] because of implant migration, persistent pain, deep infection, or overcorrection. Implant change was performed for implant migration, overcorrection, or undercorrection in four studies [33, 34, 41, 42]. The re-operation rate based on the implant type ranged from 0.9 to 36.4% and from 0 to 15.4% in the old-type [35, 38,39,40,41,42] and recent-type implants [4, 10, 32,33,34, 36], respectively.
Subgroup analysis
The studies included in our current analysis were divided into those investigating idiopathic flatfoot and neuromuscular flatfoot in order to analyze the influence of the specific origin of flatfoot (Table 9). However, studies featuring both idiopathic and neuromuscular flatfoot could not be included in this particular subgroup analysis because patients with idiopathic flatfoot had been mixed with patients with neuromuscular flatfoot. Consequently, radiographic parameters could not be compared between LCL and AR because most studies in the AR groups rarely reported radiographic results. In the LCL group, the correction of radiographic parameters was comparable between idiopathic and neuromuscular flatfoot, even though idiopathic flatfoot had a tendency towards slightly greater correction than neuromuscular flatfoot. In both idiopathic and neuromuscular flatfoot, the complication rates were higher in the LCL group than in the AR group, and the complication rates were comparable between idiopathic and neuromuscular flatfoot in both the LCL and AR groups. However, there were limitations in this particular subgroup analysis because of the small number of studies included and due to the heterogeneity of the parameters reported.
In 21 studies incorporated into the LCL group, 13 studies included only ambulatory children, two studies included ambulatory and non-ambulatory children, and six studies did not report the ambulatory status of the patients involved. In 13 studies incorporated into the AR group, five studies included only ambulatory children and eight studies did not report the ambulatory status of the patients involved. In two studies included in the LCL group, which included ambulatory and non-ambulatory children, one study [24] reported that the ambulatory status was not associated with the Goldberg score for calcaneal bone graft and does not necessarily correlate with graft failure. The other study [27] reported that there was a significant correlation between ambulatory status of the children and both clinical outcome and radiological result according to Mosca’s criteria. It is well known that a non-ambulatory status is associated with poor outcomes after LCL with respect to deformity correction [9, 21].
Discussion
For the surgical treatment of paediatric flexible flatfoot deformity, LCL has been the mainstay of surgical options. AR has also gained popularity because of its advantages, such as minimal invasive procedure and an early weight-bearing capacity. Although both procedures are popular surgical options to treat pediatric flexible flatfoot deformity, studies comparing these two procedures are limited. Therefore, we performed a systematic review to compare radiographic correction, clinical outcomes, complications, and reoperations between the two procedures for pediatric flexible flatfoot deformity.
In this systematic review, six radiographic parameters, which were reported in more than two studies in each group, were analyzed to compare radiographic corrections between both groups. The LCL group had more improvements in the anteroposterior talo-first metatarsal angle and calcaneal pitch. LCL is typically reserved for severe forefoot abduction deformity and has better correction power for midfoot transverse plane deformities than AR [4, 48]. This is supported by the result of our systematic review that the LCL group had a greater decrease in the anteroposterior talo-first metatarsal angle. Metcalfe et al. [49] reported that the calcaneal pitch among nine radiographic parameters demonstrated the least change with only small increases following AR, and Morris et al. [44] noted that AR does not change the calcaneal pitch. This is consistent with the result of our systematic review that an increase in the calcaneal pitch post-operatively in the LCL group was greater than that in the AR group. A prospective comparative study of LCL and AR for paediatric flatfoot reported that the calcaneal pitch increased significantly post-operatively only in the LCL group [4], whereas a study using AR for adult flatfoot deformity reported that the calcaneal pitch improved significantly [50].
Ten studies [4, 8, 10, 15, 17, 19, 27, 32, 34, 36] reported clinical scores using six kinds of scores. Other scores, except the AOFAS and OxAFQ scores, were used only once in one study regardless of the groups. The AOFAS scores were reported in six studies [17, 19, 27, 32, 34, 36] (three studies in each group). In the ranges of increases of the mean AOFAS score, the minimum value in the LCL group (range, 27.76–39.1) was greater than the maximum value in the AR group (range, 17–22), which meant that the LCL group has more improved AOFAS scores. The OxAFQ scores were reported in three studies [4, 10, 15], and both groups showed improvement in the OxAFQ scores. However, comparing the OxAFQ scores between both groups was difficult because studies reporting these scores were limited.
The complication rates in the LCL group were higher overall than those in the AR group, whereas the re-operation rates were similar in the two groups. The most common complication in the LCL group was calcaneocuboid subluxation, which was reported in seven studies [8, 19, 20, 26, 28, 29, 46]. Its incidence was > 50% in four [8, 19, 28, 46] of seven studies. The high incidence rate of calcaneocuboid subluxation might be the reason for the higher complication rate in the LCL group. Although the incidence of calcaneocuboid subluxation was high, this complication could gradually resolve over time and have little effect on the clinical outcome and symptoms [8, 20, 46]. That is why the re-operation rates were similar to the two groups, although the LCL group had a higher complication rate. The most common cause for re-operation in the LCL group was loss of correction. In the literature, the most common post-operative complications of AR were tarsal sinus pain, insufficient or excessive correction caused by inappropriate implant size, excessive intrusion or protrusion of the implants, and related synovitis [51, 52]. In this systematic review, persistent pain was the most common complication in the AR group, followed by implant migration. Residual pain after AR was the most common reason for dissatisfaction [10]. Overcorrection was an important cause of tarsal sinus pain after AR, and the solution was also implant removal [53]. In our systematic review, the highest incidence of persistent pain was 36.4% in Black et al.’s study [39], and the highest rate of implant migration was 19.3% in Smith et al.’s study [35]. Old-type implants were used in these two studies. In addition, both complication and re-operation rates in the old-type implant group were higher than those in the recent-type implant group. Therefore, the advance in AR design has improved the outcomes. The unsatisfactory or poor results in the LCL group were due to a recurrence of planovalgus deformity, overcorrection, medial foot collapse, subluxation of the calcaneocuboidal joint, and resorption of the allograft [5, 21, 25, 29, 30]. In the AR group, unsatisfactory or poor results were due to implant dislocations, implant fractures, overcorrection of hindfoot deformity, and the recurrence of deformity [34, 37, 40, 41].
Even though both LCL and AR are currently used worldwide for the treatment of symptomatic flexible flatfeet in children, the precise indications for the application of these procedures have not been established. In addition, AR is still a debated procedure because of the poor-quality evidence (level IV or V studies) reported in the current literature [54]. LCL is a more ideal procedure for flatfoot with severe forefoot abduction because forefoot abduction is better corrected with LCL than with AR [4, 48]. LCL is considered to be more applicable for severe forefoot abduction with 40% to 50% of talonavicular uncoverage [48]. One goal of AR is to relocate the talus in an appropriate manner over the calcaneus to allow remodeling of the subtalar joint. Thus, there may not be sufficient time for the remodeling of hindfoot bones and ligaments in patients older than 12 years of age. Prior to eight years of age, many children with flatfoot may experience spontaneous correction. Therefore, AR is recommended in children between eight and 12 years of age [2]. We also prefer LCL in cases of flatfoot with severe forefoot abduction, and prefer to use AR in pre-adolescent patients with moderate forefoot abduction as an isolated or complementary surgical procedure.
This systematic review has several limitations. First, the underlying diagnosis and the inclusion criteria were heterogeneous among the included studies based on accompanying neuromuscular disease and whether or not include non-ambulatory. Hence, the heterogeneity of the underlying diagnosis and the inclusion criteria may be a potential source of bias. Second, the diversity of LCL methods, implant type for AR, and simultaneous procedures may have had an influence on the treatment outcomes. LCL methods were diverse based on lengthening site (intra-calcaneal lengthening versus calcaneocuboid joint lengthening), whether bone graft fixation was performed, methods of bone graft fixation, and kinds of bone graft. The data could not be separated by lengthening site or implant type because of the insufficient number of studies. Third, the limited number of the studies contributed to the analysis of radiographic outcomes because substantial variation was observed in the radiographic parameters reported between studies. We selected only six radiographic parameters, which were reported in more than two studies in each group, for evaluating radiographic outcome. In addition, the time frame of the final radiographic assessment varied between studies or was not clarified. Fourth, few studies reported the clinical scores, and various clinical scores were used in the included studies. Although the results of the AOFAS score in this systematic review showed that the LCL group achieved more improvement than the AR group, more studies reporting the clinical scores are necessary to strengthen this result. Finally, only one included study [4] directly compared LCL with AR. Most included studies were case series. Although nine studies [8, 15, 18, 20, 23, 24, 26, 28, 36] were comparative studies, they did not directly compare LCL with AR. Therefore, we were unable to perform a meta-analysis for statistical comparison because of the design heterogeneity of the included studies.
In conclusion, the LCL group achieved more radiographic corrections and more improvements in the AOFAS score than the AR group. Complications were more common in the LCL group than in the AR group, and the re-operation rates were similar between the two groups. Calcaneocuboid subluxation and nonunion were the major complications in the LCL group, but revision surgery was unnecessary in most of them. Loss of correction was the main cause of revision surgery in the LCL group. Persistent pain and implant migration were the main complications in the AR group, and implant removal as a revision surgery was mainly performed for these complications.
References
Bouchard M, Mosca VS (2014) Flatfoot deformity in children and adolescents: surgical indications and management. J Am Acad Orthop Surg 22:623–632. https://doi.org/10.5435/JAAOS-22-10-623
Fernandez de Retana P, Alvarez F, Viladot R (2010) Subtalar arthroereisis in pediatric flatfoot reconstruction. Foot Ankle Clin 15:323–335. https://doi.org/10.1016/j.fcl.2010.01.001
Mourkus H, Prem H (2018) Double calcaneal osteotomy with minimally invasive surgery for the treatment of severe flexible flatfeet. Int Orthop 42:2123–2129. https://doi.org/10.1007/s00264-018-3910-2
Chong DY, Macwilliams BA, Hennessey TA, Teske N, Stevens PM (2015) Prospective comparison of subtalar arthroereisis with lateral column lengthening for painful flatfeet. J Pediatr Orthop B 24:345–353. https://doi.org/10.1097/BPB.0000000000000179
Andreacchio A, Orellana CA, Miller F, Bowen TR (2000) Lateral column lengthening as treatment for planovalgus foot deformity in ambulatory children with spastic cerebral palsy. J Pediatr Orthop 20:501–505
Evans D (1975) Calcaneo-valgus deformity. J Bone Joint Surg Br 57:270–278
Mosca VS (1995) Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am 77:500–512
Moraleda L, Salcedo M, Bastrom TP, Wenger DR, Albinana J, Mubarak SJ (2012) Comparison of the calcaneo-cuboid-cuneiform osteotomies and the calcaneal lengthening osteotomy in the surgical treatment of symptomatic flexible flatfoot. J Pediatr Orthop 32:821–829. https://doi.org/10.1097/BPO.0b013e3182648c74
Zeifang F, Breusch SJ, Doderlein L (2006) Evans calcaneal lengthening procedure for spastic flexible flatfoot in 32 patients (46 feet) with a followup of 3 to 9 years. Foot Ankle Int 27:500–507
Martinelli N, Bianchi A, Martinkevich P, Sartorelli E, Romeo G, Bonifacini C, Malerba F (2017) Return to sport activities after subtalar arthroereisis for correction of pediatric flexible flatfoot. J Pediatr Orthop B 27:82–87. https://doi.org/10.1097/BPB.0000000000000449
Mosca VS (2010) Flexible flatfoot in children and adolescents. J Child Orthop 4:107–121. https://doi.org/10.1097/BPB.0000000000000449
Schon LC (2007) Subtalar arthroereisis: a new exploration of an old concept. Foot Ankle Clin 12:329–339
Needleman RL (2006) A surgical approach for flexible flatfeet in adults including a subtalar arthroereisis with the MBA sinus tarsi implant. Foot Ankle Int 27:9–18
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 339:b2535. https://doi.org/10.1136/bmj.b2535
Martinkevich P, Rahbek O, Stilling M, Pedersen LK, Gottliebsen M, Soballe K, Moller-Madsen B (2016) Is structural hydroxyapatite tricalcium-phosphate graft or tricortical iliac crest autograft better for calcaneal lengthening osteotomy in childhood? Interim results from a randomised, controlled non-inferiority study. Bone Joint J 98-B:1554–1562
Westberry DE, Davids JR, Anderson JP, Pugh LI, Davis RB, Hardin JW (2013) The operative correction of symptomatic flat foot deformities in children: the relationship between static alignment and dynamic loading. Bone Joint J 95-B:706–713. https://doi.org/10.1302/0301-620X.95B5.30594
Viegas GV (2003) Reconstruction of the pediatric flexible planovalgus foot by using an Evans calcaneal osteotomy and augmentative medial split tibialis anterior tendon transfer. J Foot Ankle Surg 42:199–207
Rhodes J, Mansour A, Frickman A, Pritchard B, Flynn K, Pan Z, Chang F, Miller N (2017) Comparison of allograft and bovine xenograft in calcaneal lengthening osteotomy for flatfoot deformity in cerebral palsy. J Pediatr Orthop B 37:e202–e208. https://doi.org/10.1097/BPO.0000000000000822
Marengo L, Canavese F, Mansour M, Dimeglio A, Bonnel F (2017) Clinical and radiological outcome of calcaneal lengthening osteotomy for flatfoot deformity in skeletally immature patients. Eur J Orthop Surg Traumatol 27:989–996. https://doi.org/10.1007/s00590-017-1909-9
Kim JR, Shin SJ, Wang SI, Kang SM (2013) Comparison of lateral opening wedge calcaneal osteotomy and medial calcaneal sliding-opening wedge cuboid-closing wedge cuneiform osteotomy for correction of planovalgus foot deformity in children. J Foot Ankle Surg 52:162–166. https://doi.org/10.1053/j.jfas.2012.12.007
Noritake K, Yoshihashi Y, Miyata T (2005) Calcaneal lengthening for planovalgus foot deformity in children with spastic cerebral palsy. J Pediatr Orthop B 14:274–279
Oeffinger DJ, Pectol RW Jr, Tylkowski CM (2000) Foot pressure and radiographic outcome measures of lateral column lengthening for pes planovalgus deformity. Gait Posture 12:189–195
Luo CA, Kao HK, Lee WC, Yang WE, Chang CH (2017) Limits of calcaneal lengthening for treating planovalgus foot deformity in children with cerebral palsy. Foot Ankle Int 38:863–869. https://doi.org/10.1177/1071100717702596
Lee IH, Chung CY, Lee KM, Kwon SS, Moon SY, Jung KJ, Chung MK, Park MS (2015) Incidence and risk factors of allograft bone failure after calcaneal lengthening. Clin Orthop Relat Res 473:1765–1774. https://doi.org/10.1007/s11999-014-4052-5
Kadhim M, Holmes L Jr, Miller F (2013) Long-term outcome of planovalgus foot surgical correction in children with cerebral palsy. J Foot Ankle Surg 52:697–703. https://doi.org/10.1053/j.jfas.2013.06.010
Dogan A, Zorer G, Mumcuoglu EI, Akman EY (2009) A comparison of two different techniques in the surgical treatment of flexible pes planovalgus: calcaneal lengthening and extra-articular subtalar arthrodesis. J Pediatr Orthop B 18:167–175. https://doi.org/10.1097/BPB.0b013e32832c2f32
Ettl V, Wollmerstedt N, Kirschner S, Morrison R, Pasold E, Raab P (2009) Calcaneal lengthening for planovalgus deformity in children with cerebral palsy. Foot Ankle Int 30:398–404. https://doi.org/10.3113/FAI.2009.0398
Adams SB Jr, Simpson AW, Pugh LI, Stasikelis PJ (2009) Calcaneocuboid joint subluxation after calcaneal lengthening for planovalgus foot deformity in children with cerebral palsy. J Pediatr Orthop 29:170–174. https://doi.org/10.1097/BPO.0b013e3181982c33
Kwak YH, Park KB, Park HW, Kim HW (2008) Use of allograft in skeletally immature patients for calcaneal neck lengthening osteotomy. Yonsei Med J 49:79–83. https://doi.org/10.3349/ymj.2008.49.1.79
Yoo WJ, Chung CY, Choi IH, Cho TJ, Kim DH (2005) Calcaneal lengthening for the planovalgus foot deformity in children with cerebral palsy. J Pediatr Orthop 25:781–785
Danko AM, Allen B Jr, Pugh L, Stasikelis P (2004) Early graft failure in lateral column lengthening. J Pediatr Orthop 24:716–720
Jay RM, Din N (2013) Correcting pediatric flatfoot with subtalar arthroereisis and gastrocnemius recession: a retrospective study. Foot ankle Spec 6:101–107. https://doi.org/10.1177/1938640012470714
Scharer BM, Black BE, Sockrider N (2010) Treatment of painful pediatric flatfoot with Maxwell-Brancheau subtalar arthroereisis implant a retrospective radiographic review. Foot Ankle Spec 3:67–72. https://doi.org/10.1177/1938640010362262
Cao L, Miao XD, Wu YP, Zhang XF, Zhang Q (2017) Therapeutic outcomes of Kalix II in treating juvenile flexible flatfoot. Orthop Surg 9:20–27. https://doi.org/10.1111/os.12309
Smith RD, Rappaport MJ (1983) Subtalar arthroereisis. A four-year follow-up study. J Am Podiatry Assoc 73:356–361
Wen J, Liu H, Xiao S, Li X, Fang K, Zeng M, Tang Z, Cao S, Li F (2017) Comparison of mid-term efficacy of spastic flatfoot in ambulant children with cerebral palsy by 2 different methods. Medicine (Baltimore) 96:e7044. https://doi.org/10.1097/MD.0000000000010690
Molayem I, Persiani P, Marcovici LL, Rosi S, Calistri A, Villani C (2009) Complications following correction of the planovalgus foot in cerebral palsy by arthroereisis. Acta Orthop Belg 75:374–379
Viladot A (1992) Surgical treatment of the child’s flatfoot. Clin Orthop Relat Res:34–38
Black PR, Betts RP, Duckworth T, Smith TW (2000) The Viladot implant in flatfooted children. Foot Ankle Int 21:478–481
Vedantam R, Capelli AM, Schoenecker PL (1998) Subtalar arthroereisis for the correction of planovalgus foot in children with neuromuscular disorders. J Pediatr Orthop 18:294–298
Carranza-Bencano A, Zamora-Navas P, Fernandez-Velazquez JR (1997) Viladot's operation in the treatment of the child’s flatfoot. Foot Ankle Int 18:544–549
Crawford AH, Kucharzyk D, Roy DR, Bilbo J (1990) Subtalar stabilization of the planovalgus foot by staple arthroereisis in young children who have neuromuscular problems. J Bone Joint Surg Am A 72:840–845
Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int 15:349–353
Morris C, Liabo K, Wright P, Fitzpatrick R (2007) Development of the Oxford ankle foot questionnaire: finding out how children are affected by foot and ankle problems. Child Care Health Dev 33:559–568
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Ahn JY, Lee HS, Kim CH, Yang JP, Park SS (2014) Calcaneocuboid joint subluxation after the calcaneal lengthening procedure in children. Foot Ankle Int 35:677–682. https://doi.org/10.1177/1071100714528494
Martinelli N, Romeo G, Bonifacini C, Vigano M, Bianchi A, Malerba F (2016) Validation of the Italian version of the Oxford Ankle Foot Questionnaire for children. Qual Life Res 25:117–123. https://doi.org/10.1007/s11136-015-1064-x
Stein BE, Schon LC (2015) Posterior tibial tendon dysfunction in the adult: current concepts. Instr Course Lect 64:441–450
Metcalfe SA, Bowling FL, Reeves ND (2011) Subtalar joint arthroereisis in the management of pediatric flexible flatfoot: a critical review of the literature. Foot Ankle Int 32:1127–1139. https://doi.org/10.3113/FAI.2011.1127
Yasui Y, Tonogai I, Rosenbaum AJ, Moore DM, Takao M, Kawano H, Kennedy JG (2017) Use of the arthroereisis screw with tendoscopic delivered platelet-rich plasma for early stage adult acquired flatfoot deformity. Int Orthop 41:315–321. https://doi.org/10.1007/s00264-016-3349-2
Needleman RL (2005) Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int 26:336–346
Bourlez J, Joly-Monrigal P, Alkar F, Laborde A, Cottalorda J, Louahem D, Delpont M (2018) Does arthroscopic resection of a too-long anterior process improve static disorders of the foot in children and adolescents? Int Orthop 42:1307–1312. https://doi.org/10.1007/s00264-017-3740-7
Soomekh DJ, Baravarian B (2006) Pediatric and adult flatfoot reconstruction: subtalar arthroereisis versus realignment osteotomy surgical options. Clin Podiatr Med Surg 23:695–708
Bernasconi A, Lintz F, Sadile F (2017) The role of arthroereisis of the subtalar joint for flatfoot in children and adults. EFORT Open Rev 2:438–446. https://doi.org/10.1302/2058-5241.2.170009
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Suh, D.H., Park, J.H., Lee, S.H. et al. Lateral column lengthening versus subtalar arthroereisis for paediatric flatfeet: a systematic review. International Orthopaedics (SICOT) 43, 1179–1192 (2019). https://doi.org/10.1007/s00264-019-04303-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-019-04303-3