Abstract
Purpose
The purpose of the study is to determine the effectiveness of semi-active and active robotic hip and knee arthroplasty on post-operative patient-reported outcomes of function, pain, quality of life and satisfaction with surgery.
Methods
PubMed, Medline, Embase and CENTRAL were searched. Included were comparative studies investigating the effectiveness of semi-active or active robotic hip or knee arthroplasty compared to any other surgical intervention on function, pain, quality of life and satisfaction with surgery. Risk of bias and the strength of the evidence were assessed using the Downs and Black tool and the GRADE system, respectively. Relative risks, mean differences and 95% CI were calculated using random-effects models.
Results
Fourteen studies involving 1342 patients were included. All studies compared robotic to conventional surgery, with active robotic surgery evaluated in total hip or knee arthroplasty and semi-active robotic surgery in total hip or unicompartmental knee arthroplasty. Most studies presented some risk of bias, and the strength of evidence was rated as low to very low quality. Random-effects meta-analyses showed that post-operative functional outcomes were comparable between active robotic and conventional total hip and knee arthroplasty at the short-, medium- and long-term follow-up. No significant difference in pain, quality of life and satisfaction with surgery were reported in individual studies.
Conclusions
This systematic and meta-analyses indicates that functional outcomes for patients undergoing active robotic total hip and knee arthroplasty were comparable to conventional surgery. Whether semi-active or active robotic hip or knee arthroplasty is effective in improving post-operative pain, quality of life and satisfaction with surgery is unclear.
PROSPERO Registration Number: CRD42017059932.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conventional hip and knee arthroplasty are common procedures effectively employed to manage advanced degenerative and inflammatory joint disease [1], providing acceptable survivorship and significantly improving quality of life (QOL) by reducing pain and restoring function [1, 2]. Previous studies have demonstrated that hip and knee arthroplasty survivorship are correlated with intra-operative factors such as leg alignment, component alignment, component fixation, joint line maintenance and soft tissue balancing [3, 4]. To improve surgical accuracy and precision and ultimately QOL and survivorship, several robotic-assisted arthroplasty surgery systems have been developed in the last two decades [5]. While there is evidence suggesting that robotic surgery improves the accuracy of prosthesis implantation when compared to conventional hip and knee arthroplasty [3, 4], at present, it is unclear if robotic-assisted surgery results in improved functional outcomes, pain, QOL and satisfaction with surgery.
Robotic surgery may be classified as a passive, semi-active or active robotic system, depending on how independently the system performs the manoeuvres [6]. Passive robotic systems assist the surgeon by displaying the surgical plan to be followed, while semi-active and active robotic systems directly influence the surgeon’s operative technique by respectively providing feedback or carrying out a pre-programmed surgical plan under the supervision of the surgeon. A large proportion of the existing evidence investigating the effectiveness of robotic surgery has focussed on clinical outcomes [4, 5, 7,8,9]. Recent systematic reviews comparing semi-active and active robotic hip and knee arthroplasty versus conventional surgery reported that robotic surgery was associated with better control of prosthesis positioning, fixation and alignment [4, 8].
Controlling intra-operative clinical factors has been reported to improve the success of hip and knee arthroplasty [4, 5]; however, whether these advantages translate into improved patients’ function, pain and QOL outcomes at the short-, medium- and long- term is currently unknown. While meta-analyses of these factors have previously investigated passive robotics compared to conventional surgery, this has not been performed for semi-active or active robotic systems [4]. Previous systematic reviews have attempted to provide an overview and describe the scope of semi-active and active robotic surgery in this area, but have not attempted to pool results for patient-reported outcomes [4, 8]. Therefore, the effect of robotic surgery, as compared to conventional surgery, from a patient’s perspective has not been elicited.
Patient-reported outcomes inform clinicians of the impact the treatment has on the patient and therefore has a significant role in guiding decision making for treatment [10]. As a result, knowledge of the effectiveness of robotic surgery for hip or knee arthroplasty on functional, pain and QOL outcomes will provide invaluable information to clinicians, patients and policy makers. Therefore, the aim of this systematic review was to evaluate the effectiveness of semi-active and active robotic hip and knee arthroplasty on patient-reported outcomes. Primary outcomes of interest were function, pain, QOL and patient satisfaction with these surgeries at short-, medium- and long- term.
Materials and methods
The protocol of this systematic review and meta-analysis was registered on PROSPERO (https://www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42017059932; registration number CRD42017059932) prior to the start of the study and was written in accordance with PRISMA-P [11]. The review followed the methods recommended by the Cochrane Handbook for Systematic Reviews of Interventions [12], and was written in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [13]. The PRISMA checklist in reported in Online Resource 1.
Search strategy
The electronic databases of PubMed, Medline, Embase and Cochrane Central Register of Controlled Trials (CENTRAL) were searched (via Ovid) from inception till 20 March 2017. In addition to the electronic database searches, Google Scholar was searched and pearling of reference lists of studies was conducted for additional relevant articles. We also contacted an expert in the field, not involved in the review, to check if any published report was missed.
The search strategy was based on key terms for “arthroplasty”, “robotic surgery”, “hip” and “knee” (Online Resource 2). For each potentially eligible study, the full-text article was obtained and assessed against the inclusion criteria. Studies were screened by two independent review authors (SK and MD), and conflicts regarding included studies were resolved by discussion with a third review author (DS).
Inclusion criteria
This review included comparative studies (e.g. randomised controlled trials [RCTs], cohort studies) reporting the effectiveness of semi-active and/or active robotic arthroplasty compared to any other surgical intervention (e.g. conventional, passive robot). Semi-active robots were defined as any device that provided feedback or constrained the surgical plan within a pre-determined area greater than a conventional cutting guide (e.g. Mako, Acrobot, Navio Precision Freehand Sculptor). Active robots were defined as any device that performed surgical procedures without the direct intervention of a surgeon (e.g. ROBODOC, CASPAR).
Eligible studies met the following criteria: (1) reported on adults (≥ 18 years old) of any gender; (2) investigated any type of hip or knee arthroplasty (e.g. total hip [THA] or knee [TKA] arthroplasty, partial hip arthroplasty [PHA], unicompartmental knee arthroplasty [UKA], bi-unicompartmental knee arthroplasty [Bi-UKA]); and (3) presented at least one patient reported outcome measure of function, pain, QOL or overall patient satisfaction with the surgery at any follow-up time. Follow-up periods were categorised into short (≤ 3 months), medium (3–12 months) or long term (≥ 12 months). If studies reported multiple time points within each follow-up interval, the time point closest to two months was considered as the shortest time point, the medium time point was considered as the closest to six months and the longest time point was considered as the closest to 12 months. No language or publication restrictions were employed, with translations attempted for all non-English published studies.
Data extraction process
A standardised piloted data extraction form was employed to collate study information, participants’ baseline characteristics, intervention, control characteristics and outcome data. Two reviewers (SK and MD) independently extracted data from the included studies, and disagreements were resolved by discussion and consensus. If consensus could not be reached, a third reviewer (DS or MH) was consulted. Studies that were published in duplicate were only included once, but all versions were considered for maximal data extraction. If missing data were found, we made attempts to contact authors.
Assessment of studies
Risk of bias of the included studies was assessed by two independent reviewers (SK and MD) using the Downs and Black Quality Checklist for Health Care Intervention Studies [14]. This tool evaluates the study’s reporting quality (10 items), external validity (3 items), bias (7 items), confounding and selection bias (6 items) and power of studies (1 item) (Online Resource 3). Scores using this tool range from 0 (high risk of bias) to 32 (low risk of bias).
The strength of the evidence of the included studies was assessed from high to very low quality for each outcome using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system [11]. In brief, the quality of evidence was downgraded from high quality by one level according to the following criteria: (1) risk of bias (> 25% of patients from studies with high risk of bias [Downs and Black score < 26]); (2) inconsistency (statistically significant heterogeneity [I2 > 50% or ≤ 75% of studies with findings in the same direction]); and (3) imprecision (only 1 study or > 1 study with < 300 patients for each outcome). Two reviewers (SK and MD) independently rated the overall quality of evidence and consensus between these reviewers for all evaluations was used to resolve any disagreement.
Statistical analysis
For dichotomous outcomes, an estimate of the relative risk (RR) and its 95% confidence interval (CI) was calculated, where a RR value < 1 favoured robotic surgery. Continuous outcomes were analysed by calculation of the mean difference (MD) and 95% CI, where a negative MD value favoured robotic surgery.
Results from included studies were converted to a score out of 100, where a higher score indicated a better outcome, for ease of comparison across all outcomes (e.g. Oxford Knee Score of 48/60 was converted to 75/100) [15]. Homogeneous outcome measures from individual studies were combined through a meta-analysis using a random-effects model and correlated outcomes combined [16,17,18,19,20], where appropriate (r value > 0.5). If a meta-analysis was not possible, the results were qualitatively reported. Statistical heterogeneity was assessed visually and using the I2 statistic.
Results
Search results
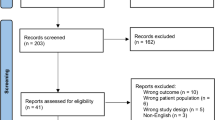
The search yielded 2957 articles across all databases after duplicates were removed. Following elimination of clearly irrelevant references, 118 full-text articles were screened for eligibility. After screening of the full-text articles, 100 articles were excluded based on being of ineligible study design (n = 60), not reporting outcomes of interest (n = 28) and not evaluating an intervention of interest (n = 12) (Online Resource 4). Therefore, 18 articles were included of which 14 reported on a unique sample (Fig. 1).
Study design and characteristics
Included studies investigated the effectiveness of active robotic versus conventional THA (n = 7; reported by four RCTs and three prospective cohorts) [21,22,23,24,25,26,27], semi-active robotic versus conventional THA (n = 1; reported by one retrospective cohort) [28], active robotic versus conventional TKA (n = 4; all reported by RCTs) [29,30,31,32] and semi-active robotic versus conventional UKA (n = 2; reported by one RCT and one prospective cohort) [33, 34] (Table 1).
Sample sizes ranged from 28 [33] to 200 [28], with a total of 955 hip arthroplasties (mean age ± SD = 60.54 ± 11.94 years) and 387 knee arthroplasties (mean age ± SD = 66.59 ± 6.80 years) reported. Functional outcomes were reported by all included studies, with follow-up times ranging from six weeks [33] to 13 years [21]. Six studies reported on the difference of pain scores [22, 25, 26, 29, 33, 34].
Osteoarthritis was the predominant diagnosis in the included robotic hip arthroplasty studies [21,22,23, 25,26,27,28], with one study mostly reporting on osteonecrosis patients [24]. Additionally, four of these studies included patients treated for pathologies other than osteoarthritis [24,25,26,27]. Studies investigating knee robotic surgery examined patients presenting with osteoarthritis [29,30,31,32,33], although one study did not specify the diagnoses of their participants [34]. Table 1 presents the characteristics of the included studies.
Risk of bias assessment
Table 2 summarises the risk of bias for individual studies. All studies had at least one domain considered to be high risk of bias, and five studies (36%) were judged with more than two domains. The most common methodological flaw was found in the confounding domain, which investigated biases in the selection of study subjects (n = 11; 79%). This was followed by power (n = 9; 64%), where no study evaluating knee arthroplasty was considered to meet the criteria. The least methodological flaws were found to be in the domains of external validity (n = 12; 86%) and reporting quality (n = 11; 79%).
Summary of findings and strength of evidence
THA active robotic versus conventional surgery
The outcomes of active robotic compared to conventional THA surgery were investigated by seven studies [21,22,23,24,25,26,27], including 755 hip arthroplasties (Table 3). Short-term results for function reported no significant differences between groups when results were pooled for the Merle d’Aubigne Score (MD − 0.41; 95% CI − 5.31 to 4.48) (Fig. 2). This was also found when short-term function was evaluated by the modified Harris Hip Score (mHHS) (MD 0.40; p > 0.05; 95% CI not reported) [21], Harris Hip Score (HHS) (MD − 0.90; 95% CI − 4.84 to 3.04) and Mayo Clinical Hip Score (MD 4.75; 95% CI − 0.48 to 9.98) [23], providing low to very low quality of evidence. A single study evaluated function in the medium term using the Merle d’Aubigne Score (MD − 2.22; 95% CI − 8.40 to 3.95) and HHS (MD − 6.10; 95% CI − 12.34 to 0.14), providing low-quality evidence of no difference between groups [23]. Though, this study also presented very-low-quality evidence of a difference between groups favouring active robotic surgery using the Mayo Clinical Hip Score (MD − 9.50; 95% CI − 16.55 to − 2.45). At long term, pooled estimates of function using the Merle d’Aubigne Score (MD − 1.25; 95% CI − 3.90 to 1.41) and combined mHHS and HHS (MD − 2.90; 95% CI − 9.04 to 3.24) provided low-quality evidence of no difference between groups (Fig. 2). We also performed a sensitivity analysis including only RCTs (i.e. removing non-randomised comparative studies) and found similar pooled estimates for the Merle d’Aubigne Score (MD − 3.96; 95% CI − 9.32 to 1.40) or combined mHHS and HHS (MD − 4.62; 95% CI − 13.32 to 4.09) (Online Resource 5). Lim et al. assessed function using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and reported no difference between groups (MD − 1.0; 95% CI − 2.47 to 0.47). However, low quality of evidence of an increase in function, favouring active robotic surgery, was reported when assessed by the Mayo Clinical Hip Score (MD − 12.88; 95% CI − 18.27 to − 7.48) [23] and Japanese Orthopaedic Association (JOA) Score (MD − 2.00; 95% CI − 3.89 to − 0.11) [25].
Mean difference for functional outcomes in trials comparing active robotic versus conventional total hip arthroplasty. Studies are ordered chronologically within functional outcomes. Short-term indicates follow-up periods < 3 months. Long-term indicates follow-up periods > 12 months. Negative values favour active robotic surgery. MD mean difference.*modified Harris Hip Score
Pain was assessed in three studies [22, 25, 26], including 344 hip arthroplasties (Table 3). Low-quality evidence was found in one study (n = 156) that reported no significant difference between groups when patients reported if they experienced thigh pain at short term (RR 2.75; 95% CI 0.91 to 8.27) [26] and at medium term (RR 1.50; 95% CI 0.26 to 8.73) [26]. The pain domain of the Merle d’Aubigne Score was reported in one study (n = 58) at long term with no difference between groups (MD 0.00; p > 0.05; 95% CI not reported) [22]. Nakamura et al. (n = 130) investigated if patients presented pain in their thigh (RR 4.23; 95% CI 0.48 to 36.9) or knee (only two patients in the robotic group reported knee pain) and found no differences between robotic and conventional surgery at long term [25].
Bargar et al. (n = 103) evaluated QOL using the Short Form 36 Health Survey (SF-36) overall scaled score in the short (MD 2.60; p > 0.05; 95% CI not reported), medium (MD 3.20; p > 0.05; 95% CI not reported) and long term (MD − 2.40; p > 0.05; 95% CI not reported), and provided very low quality of evidence of no difference between groups [21] (Table 3).
THA semi-active robotic versus conventional surgery
One study (n = 200) compared long-term outcomes of semi-active robotic versus passive robotic THA surgery and provided low-quality evidence for all outcomes [28] (Table 3). No difference between groups was found when function was evaluated by the mHHS (MD − 6.00; 95% CI − 9.78 to 2.22) and WOMAC (MD − 1.30; 95% CI − 5.51 to 2.91).
In terms of QOL (Short Form 12 Health Survey), there was no difference between groups in both the physical component summary (PCS) (MD − 1.60; 95% CI − 4.58 to 1.38) and the mental component summary (MCS) (MD − 1.60; 95% CI − 4.28 to 1.08) at long term.
TKA active robotic versus conventional surgery
Four studies reported data from 282 TKAs comparing active robotic to conventional surgery (Table 3) [29,30,31,32]. In the short term, one study (n = 60) provided very-low-quality evidence of no significant difference between group when evaluating function using the Hospital for Special Surgery (HSS) Score (MD − 0.60; 95% CI − 3.97 to 2.77) and WOMAC (MD 0.40; 95% CI − 5.77 to 6.57) [31]. Low quality of evidence of no difference between groups in the medium term was reported when estimates of the Knee Society Function Score (KSS-F) and HSS function scores were pooled (MD 0.04; 95% CI − 2.94 to 3.01) (Fig. 3). No difference between groups was reported in the medium term when function was assessed by the WOMAC (MD 0.20; 95% CI − 5.14 to 5.54) [31] and Oxford Knee Score (OKS) (MD 0.63; 95% CI − 1.17 to 2.42) [29]. In the long term, all four studies reported low quality of evidence of no difference between groups when estimates of function were pooled using the KSS-F and HSS (MD − 0.51; 95% CI − 1.83 to 0.82) or KSS-F and WOMAC (MD − 0.51; 95% CI − 1.95 to 0.94) (Fig. 3). No difference between groups was also found when function was evaluated by the OKS (MD 1.25; 95% CI − 0.16 to 2.66) [29], providing very low quality of evidence.
Mean difference for functional outcomes in trials comparing active robotic versus conventional total knee arthroplasty. Studies are ordered chronologically within functional outcomes. Medium term indicates follow-up periods between 3 and 12 months. Long term indicates follow-up periods > 12 months. Negative values favour active robotic surgery. MD mean difference, WOMAC Western Ontario and McMaster Universities Osteoarthritis Index. *Knee Society Score-Function
Patient response to pain was reported by one study (n = 60) which found no significant differences between groups at medium (MD 4.80; 95% CI − 8.90 to 18.50) and long term (MD − 3.90; 95% CI − 16.48 to 8.68) when responding to the SF-36 Bodily Pain Score [29].
QOL was evaluated by one study (n = 60) that reported the PCS and MCS scores of the SF-36, providing very low quality of evidence [29]. In the medium term, no differences between groups was found in the PCS (MD 0.50; 95% CI − 4.76 to 5.76) and MCS (MD − 4.40; 95% CI − 9.08 to 0.28). This was also reported in the long term with the PCS (MD − 4.10; 95% CI − 9.61 to 1.41) and MCS (MD − 4.60; 95% CI − 9.69 to 0.49) (Table 3).
Patient’s satisfaction with the outcome of surgery was investigated by one study (n = 60) which reported no significant difference between groups at medium (RR 0.99; 95% CI 0.83 to 1.17) and long term (RR 0.96; 95% CI 0.82 to 1.12) [29].
UKA semi-active robotic versus conventional surgery
Two studies compared semi-active robotic to conventional surgery in patients undergoing UKA (n = 105) (Table 3) [33, 34]. Coon et al. evaluated function in the short term using the combined Clinical and Function Knee Society Score (cKSS) and reported no difference between groups (MD not reported; p > 0.05; 95% CI not reported) [34]. The cKSS was assessed by two studies, evaluating function in the medium term. Cobb et al. (n = 28) found a difference between groups favouring semi-active robotic surgery (MD not reported; p = 0.004; 95% CI not reported) [33], whereas Coon et al. (n = 77) found no difference between groups (MD not reported; p > 0.05; 95% CI not reported) [34], with both studies providing very low quality of evidence. Cobb et al. also reported no differences between groups when function was measured by the WOMAC (MD not reported; p = 0.06; 95% CI not reported) [33].
Pain was assessed in both studies (n = 105), and no significant difference between groups at medium term using the pain component of the cKSS (MD not reported; p > 0.05; 95% CI not reported) [34] and WOMAC (MD not reported; p > 0.05; 95% CI not reported) [33] was found.
Discussion
Statement of principal findings
This systematic review and meta-analysis demonstrates that comparable patient-reported outcomes are achieved at short, middle and long term in hip or knee arthroplasty when performed by a semi-active or active robotic system compared to conventional surgery. No study reported outcomes favouring conventional surgery over robotic, with reports from two individual studies showing active robotic total hip arthroplasty provides significantly better function outcomes at medium- and long-term follow-up, and one study reporting semi-active robotic unicompartmental knee arthroplasty provided better functional outcomes at medium-term follow-up. No significant difference in pain, QOL and satisfaction with surgery was reported in individual studies.
Strengths and weaknesses of the study
The strengths of this review include the adherence to a pre-specified protocol registered on PROSPERO, inclusion of all comparative papers and following of the PRISMA recommendations including the use of the GRADE system to appraise the quality of evidence. We also assessed study’s risk of bias with the Downs and Black Quality Checklist for Health Care Intervention Studies, which has been shown to have acceptable validity and reliability [14]. To facilitate the interpretation of our meta-analysis, we provided precise estimates and clinically interpretable scores on a 0–100 scale. Furthermore, the review applied no restrictions on the publication language, date of publication and patient-reported outcome measure employed, and we have contacted an expert in the field to ensure relevant studies were not missed.
We, however, were only able to identify a small number of studies (n = 14), half of which were published over a decade ago. As a result, we encountered difficulty in obtaining full data sets and raised the possibility that advances in technology may have an influence over reported results [35]. This, combined with the assessed quality of included studies, meant that the level of evidence across all studies was somewhat low. Furthermore, the inclusion of non-randomised comparative studies, and the heterogeneity of the surgical approaches regarding the instrumentation, manual rasping technique and prostheses implanted, may have also influenced the results presented. In addition, heterogeneity of outcomes employed meant that scores could not always be pooled in our meta-analysis. It was also identified that while pain was explicitly reported by six studies, only two studies provided quantifiable results to explore pain intensity.
Strengths and weaknesses in relation to other studies
To our knowledge, this is the first systematic review and meta-analysis to rigorously evaluate the effectiveness of semi-active or active robotic hip and knee arthroplasty compared to conventional surgery on patient-reported outcomes. Previous systematic and narrative reviews in this area have commonly provided general overviews or summaries, with few employing a systematic approach. Many of these articles have focussed on knee arthroplasty in terms of the clinical outcomes associated with this technology, with secondary reference to patient-reported outcome measures [4, 5, 7,8,9]. Additionally, results from three new studies, of which two are RCTS, have also been included in our review [24, 28, 29].
Meta-analysis of results from these studies through collaboration of individual study results, namely those from consistent or correlated measures, had not been attempted previously. However, Karthik et al. [8] and Jacofsky et al. [5] presented tables descriptively summarising the overall results from multiple studies, and based on their individual study summaries, the pattern of no difference between groups was somewhat consistent with the results of this review.
When collaborating these results, semi-active and active robotic systems were evaluated separately. While the differences between semi-active and active robotic systems are well established in the literature [5, 6], previous reviews have commonly grouped the two in an attempt to provide an overall interpretation of robotic surgery. Jacofsky et al. [5] attempted to distinguish between semi-active and active robotic systems and then evaluated the individual robotic devices within each group. Similarly in our review, we grouped studies accordingly to robotic system (i.e. semi-active or active), surgery performed (i.e. THA, TKA or UKA) and patient-reported outcomes (i.e. function, pain, QOL or patient satisfaction).
Unanswered questions and future research
This systematic review found a paucity of studies investigating the effectiveness between robotic surgery and conventional surgery in terms of patient-reported outcomes. A lack of consistency of outcome measures in these studies further compounded the difficulty in pooling the data for meta-analysis and establishing recommendations. This is a well-documented phenomenon in arthroplasty, with governing bodies [36, 37] and international experts [38, 39] supporting the establishment of standardised questionnaire sets to be collected.
Additionally, pain was only reported in six studies [22, 25, 26, 29, 33, 34]; however, comparable outcomes were not employed. While many outcome measures employed by the included studies evaluated pain as a component of their overall score (e.g. HHS, Merle d’Aubigne, WOMAC, OKS), explicit discussion of this was lacking. With pain being one of the primary reasons for consideration of arthroplasty [40,41,42], future studies should aim to comprehensively assess pain using standardised measures. Furthermore, a proper sample size calculation should be employed.
While the results of this review indicate that robotic and conventional surgery are comparable in terms of patient-reported measures of function, pain, QOL and satisfaction, it remains uncertain as to the effect robotic surgery truly has on these outcomes. Due to the low or very low quality of evidence presented across the included studies, further high-quality research may change the results of this review and caution should be taken when interpreting our results. Whenever possible, future studies should investigate the effect of different surgical approaches on patient-reported outcomes and further evaluate the influence of robotic surgeries on clinical outcomes such as length of stay and complications intra-operatively and post-operatively [43]. Key study design components to address in future include consistency in outcome measures employed as suggested by governing bodies [36, 37] and experts [38, 39], and increased power via improved samples sizes, particularly in knee arthroplasty studies.
Conclusion
In conclusion, this review’s findings indicate that post-operative functional outcomes for patients undergoing robotic or conventional total hip and knee arthroplasty are comparable. Although, evidence of significant improvements in function have been reported in single studies following robotic surgery at medium- and long-term follow up. Whether these results translate to improvements in post-operative pain, quality of life and satisfaction with surgery remains unclear.
References
Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) (2017) Hip, knee & shoulder arthroplasty: 2017 annual report. https://aoanjrr.sahmri.com/documents/10180/397736/Hip%2C%20Knee%20%26%20Shoulder%20Arthroplasty. Accessed 16 Apr 2018
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster J (2004) Health-related quality of life in total hip and total knee arthroplasty: A qualitative and systematic review of the literature. J Bone Joint Surg Am 86-A(5):963–974. https://doi.org/10.2106/00004623-200405000-00012
Xu K, Li Y, Zhang H, Wang C, Xu Y, Li Z (2014) Computer navigation in total hip arthroplasty: A meta-analysis of randomized controlled trials. Int J Surg 12(5):528–533. https://doi.org/10.1016/j.ijsu.2014.02.014
van der List J, Chawla H, Joskowicz L, Pearle A (2016) Current state of computer navigation and robotics in unicompartmental and total knee arthroplasty: A systematic review with meta-analysis. Knee Surg Sports Traumatol Arthrosc 24(11):3482–3495. https://doi.org/10.1007/s00167-016-4305-9
Jacofsky D, Allen M (2016) Robotics in arthroplasty: A comprehensive review. J Arthroplast 31(10):2353–2363. https://doi.org/10.1016/j.arth.2016.05.026
Picard F, Moody J, DiGioia A, Jaramaz B (2004) Clinical classification of CAOS systems. In: DiGioia A, Jaramaz B, Picard F, Nolte L (eds) Computer and robotic assisted knee and hip surgery, vol 1. Oxford University Press, New York, pp 43–48
Buza J, Waterlain A, Thakkar S, Meree P, Vigdorchik J (2017) Navigation and robotics in knee arthroplasty. JBJS Rev 5(2):e4. https://doi.org/10.2106/JBJS.RVW.16.00047
Karthik K, Colegate-Stone T, Dasgupta P, Tavakkolizadeh A, Sinha J (2015) Robotic surgery in trauma and orthopaedics: A systematic review. J Bone Joint Surg Br 97-B(3):292–299. https://doi.org/10.1302/0301-620x.97b3.35107
Lang J, Mannava S, Floyd A, Goddard M, Smith B, Mofidi A, Seyler T, Jinnah R (2011) Robotic systems in orthopaedic surgery. J Bone Joint Surg Br 93-B(10):1296–1299. https://doi.org/10.1302/0301-620x.93b10.27418
Porter I, Goncalves-Bradley D, Ricci-Cabello I, Gibbons C, Gangannagaripalli J, Fitzpatrick R, Black N, Greenhalgh J, Valderas J (2016) Framework and guidance for implementing patient-reported outcomes in clinical practice: Evidence, challenges and opportunities. J Comp Eff Res 5(5):507–519. https://doi.org/10.2217/cer-2015-0014
Atkins D, Eccles M, Flottorp S, Guyatt G, Henry D, Hill S, Liberati A, O'Connell D, Oxman A, Phillips B, Schunemann H, Edejer T, Vist G, Williams J, Grade Working Group (2004) Systems for grading the quality of evidence and the strength of recommendations I: Critical appraisal of existing approaches the GRADE working group. BMC Health Serv Res 4(1):38. https://doi.org/10.1186/1472-6963-4-38
Higgins J, Green S (2011) Cochrane handbook for systematic reviews of interventions. www.cochrane-handbook.org. Accessed 1 May 2017
Moher D, Liberati A, Tetzlaff J, Altman D, PRISMA Group (2010) Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Downs S, Black N (1998) The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health 52(6):377–384. https://doi.org/10.1136/jech.52.6.377
Pynsent P, Adams D, Disney S (2005) The Oxford hip and knee outcome questionnaires for arthroplasty. J Bone Joint Surg Br 87-B(2):241–248. https://doi.org/10.1302/0301-620X.87B2.15095
Lingard E, Katz J, Wright R, Wright E, Sledge C, Kinemax Outcomes Group (2001) Validity and responsiveness of the Knee Society Clinical Rating System in comparison with the SF-36 and WOMAC. J Bone Joint Surg Am 83-A(12):1856–1864. https://doi.org/10.2106/00004623-200112000-00014
Moonot P, Medalla GA, Matthews D, Kalairajah Y, Field RE (2009) Correlation between the Oxford knee and American Knee Society scores at mid-term follow-up. J Knee Surg 22(3):226–230. https://doi.org/10.1055/s-0030-1247753
Singh J, Schleck C, Harmsen W, Lewallen D (2013) Validation of the Hospital for Special Surgery knee questionnaire: convergent validity, responsiveness and sensitivity to change. Paper presented at the American College of Rheumatology Annual Meeting, San Diego, CA, October 25–30
Singh J, Schleck C, Harmsen W, Lewallen D (2016) Validation of the Mayo Hip Score: Construct validity, reliability and responsiveness to change. BMC Musculoskelet Disord 17:39. https://doi.org/10.1186/s12891-016-0868-3
McGrory B, Harris W (1996) Can the Western Ontario and McMaster Universities (WOMAC) Osteoarthritis Index be used to evaluate different hip joints in the same patient? J Arthroplast 11(7):841–844. https://doi.org/10.1016/S0883-5403(96)80184-7
Bargar W, Bauer A, Borner M (1998) Primary and revision total hip replacement using the ROBODOC system. Clin Orthop Relat Res 354:82–91. https://doi.org/10.1097/00003086-199809000-00011
Honl M, Dierk O, Gauck C, Carrero V, Lampe F, Dries S, Quante M, Schwieger K, Hille E, Morlock M (2003) Comparison of robotic-assisted and manual implantation of a primary total hip replacement: A prospective study. J Bone Joint Surg Am 85-A(8):1470–1478. https://doi.org/10.2106/00004623-200308000-00007
Siebel T, Kafer W (2005) Clinical outcome following robotic assisted versus conventional total hip arthroplasty: A controlled and prospective study of seventy-one patients. Z Orthop Ihre Grenzgeb 143(4):391–398. https://doi.org/10.1055/s-2005-836776
Nishihara S, Sugano N, Nishii T, Miki H, Nakamura N, Yoshikawa H (2006) Comparison between hand rasping and robotic milling for stem implantation in cementless total hip arthroplasty. J Arthroplast 21(7):957–966. https://doi.org/10.1016/j.arth.2006.01.001
Hananouchi T, Sugano N, Nishii T, Nakamura N, Miki H, Kakimoto A, Yamamura M, Yoshikawa H (2007) Effect of robotic milling on periprosthetic bone remodeling. J Orthop Res 25(8):1062–1069. https://doi.org/10.1002/jor.20376
Nakamura N, Sugano N, Nishii T, Kakimoto A, Miki H (2010) A comparison between robotic-assisted and manual implantation of cementless total hip arthroplasty. Clin Orthop Relat Res 468(4):1072–1081. https://doi.org/10.1007/s11999-009-1158-2
Lim S, Ko K, Park C, Moon Y, Park Y (2015) Robot-assisted primary cementless total hip arthroplasty with a short femoral stem: A prospective randomized short-term outcome study. Comput Aided Surg 20(1):41–46. https://doi.org/10.3109/10929088.2015.1076044
Bukowski B, Anderson P, Khlopas A, Chughtai M, Mont M, Illgen R (2016) Improved functional outcomes with robotic compared with manual total hip arthroplasty. Surg Technol Int 29:303–308
Park S, Lee C (2007) Comparison of robotic-assisted and conventional manual implantation of a primary total knee arthroplasty. J Arthroplast 22(7):1054–1059. https://doi.org/10.1016/j.arth.2007.05.036
Song E, Seon J, Park S, Jung W, Park H, Lee G (2011) Simultaneous bilateral total knee arthroplasty with robotic and conventional techniques: A prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 19(7):1069–1076. https://doi.org/10.1007/s00167-011-1400-9
Song E, Seon J, Yim J, Netravali N, Bargar W (2013) Robotic-assisted TKA reduces postoperative alignment outliers and improves gap balance compared to conventional TKA knee. Clin Orthop Relat Res 471(1):118–126. https://doi.org/10.1007/s11999-012-2407-3
Liow M, Goh G, Wong M, Chin P, Tay D, Yeo S (2016) Robotic-assisted total knee arthroplasty may lead to improvement in quality-of-life measures: A 2-year follow-up of a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc 25(9):22942–22951. https://doi.org/10.1007/s00167-016-4076-3
Cobb J, Henckel J, Gomes P, Harris S, Jakopec M, Rodriguez F, Barrett A, Davies B (2006) Hands-on robotic unicompartmental knee replacement: A prospective, randomised controlled study of the Acrobot system. J Bone Joint Surg Br 88-B(2):188–197. https://doi.org/10.1302/0301-620X.88B2.17220
Coon T, Driscoll M, Horowitz S, Conditt M (2011) Robotically assisted UKA is more accurate than manually instrumented UKA. Int J Med Robot 7:50
Australian Government (2005) Impacts of advances in medical technology in Australia. Productivity Commission. https://www.pc.gov.au/inquiries/completed/medical-technology/report/medicaltechnology.pdf. Accessed 14 Nov 2017
American Joint Replacement Registry (2016) AJRR's patient-reported outcome measure guide. http://www.ajrr.net/images/downloads/Data_elements/AJRR_PROMS_GUIDE_2016_FINAL_4-5_FINAL.pdf. Accessed 14 Nov 2017
National Health Service (2017) Patient reported outcome measures (PROMs) in England: A guide to PROMs methodology. https://digital.nhs.uk/data-and-information/data-tools-and-services/data-services/patient-reported-outcome-measures-proms. Accessed 11 Feb 2018
International Consortium for Health Outcomes Measurement (2017) ICHOM: Hip & knee osteoarthritis data collection reference guide. vol 2.2.1. Massachusetts, USA
Rolfson O, Wissig S, van Maasakkers L, Stowell C, Ackerman I, Ayers D, Barber T, Benzakour T, Bozic K, Budhiparama N, Caillouette J, Conaghan P, Dahlberg L, Dunn J, Grady-Benson J, Ibrahim S, Lewis S, Malchau H, Manzary M, March L, Nassif N, Nelissen R, Smith N, Franklin P (2016) Defining an international standard set of outcome measures for patients with hip or knee osteoarthritis: Consensus of the International Consortium for Health Outcomes Measurement Hip and Knee Osteoarthritis Working Group. Arthritis Care Res 68(11):1631–1639. https://doi.org/10.1002/acr.22868
Carr A, Robertsson O, Graves S, Price A, Arden N, Judge A, Beard D (2012) Knee replacement. Lancet 379(9823):1331–1340. https://doi.org/10.1016/S0140-6736(11)60752-6
Pivec R, Johnson A, Mears S, Mont M (2012) Hip arthroplasty. Lancet 380(9855):1768–1777. https://doi.org/10.1016/S0140-6736(12)60607-2
Turktas U, Piskin A, Poehling GG (2016) Short-term outcomes of robotically assisted patello-femoral arthroplasty. Int Orthop 40(5):919–924. https://doi.org/10.1007/s00264-015-2786-7
Herry Y, Batailler C, Lording T, Servien E, Neyret P, Lustig S (2017) Improved joint-line restitution in unicompartmental knee arthroplasty using a robotic-assisted surgical technique. Int Orthop 41(11):2265–2271. https://doi.org/10.1007/s00264-017-3633-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sascha Karunaratne, Michael Duan, Evangelos Pappas, Paul Stalley, Mark Horsley and Daniel Steffens declare that they have no conflict of interest.
Brett Fritsch owns stocks in Optimised Ortho and 360 Knee Systems; has performed consulting work for Optimised Ortho, 360 Knee Systems, Arthrex, Global Orthopaedics and Omni; and has received institutional support from Arthrex, Global Orthopaedics, Zimmer and Smith & Nephew.
Richard Boyle has performed consultancy work for Stryker, Adler, Signature and Global Orthopaedics and receives research assistance from Corin.
Sanjeev Gupta has performed consultancy work for Stryker, Depuy, Global Orthopaedics and Corin.
Electronic supplementary material
Online Resource 1
(PDF 193 kb)
Online Resource 2
(PDF 29 kb)
Online Resource 3
(PDF 162 kb)
Online Resource 4
(PDF 129 kb)
Online Resource 5
(PDF 58 kb)
Rights and permissions
About this article
Cite this article
Karunaratne, S., Duan, M., Pappas, E. et al. The effectiveness of robotic hip and knee arthroplasty on patient-reported outcomes: A systematic review and meta-analysis. International Orthopaedics (SICOT) 43, 1283–1295 (2019). https://doi.org/10.1007/s00264-018-4140-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4140-3