Abstract
Introduction
External fixation is widely accepted as a provisional or sometimes definitive treatment for long-bone fractures. Indications include but are not limited to damage control surgery in poly-traumatized patients as well as provisional bridging to definite treatment with soft tissue at risk. As little is known about surgeon’s habits in applying this treatment strategy, we performed a national survey.
Methods
We utilized the member database of the German Trauma Society (DGU). The questionnaire encompassed 15 questions that addresses topics including participants’ position, experience, workplace, and questions regarding specifics of external fixation application in different anatomical regions. Furthermore, we compared differences between trauma centre levels and surgeon-related factors.
Results
The participants predominantly worked in level 1 trauma centres (42.7%) and were employed as attendings (54.7%). There was widespread consensus for planning and intra-operative radiographical control of external fixation. Surgeons appointed at a level I trauma centre preferred significantly more often supra-acetabular pin placement in external fixation of the pelvis rather than the utilization of iliac pins (75.8%, p = 0.0001). Moreover, they were more likely to favor a mini-open approach to insert humeral pins (42.4%, p = 0.003). Overall, blunt dissection and mini-open approaches seemed equally popular (38.2 and 34.1%). Department chairmen indicated more often than their colleagues to follow written pin-care protocols for minimization of infection (16.7%, p = 0.003).
Conclusion
Despite the fact that external fixation usage is widespread and well established among trauma surgeons in Germany, there are substantial differences in the method of application.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The use of external fixation is widely accepted as a provisional and in specific cases definitive treatment of fractures. There are many commonly accepted indications for the application of an external fixator, such as damage control surgery in poly-traumatized patients, provisional stabilization when soft tissues are not amenable to definitive open fixation, and occasionally definitive management of certain fractures [30, 34, 39]. Furthermore, external fixator constructs can serve as adjuvant tools for treating non-unions or bone defects after trauma [17, 37]. Especially in the treatment of post-traumatic bone defects, external fixation is but one of the options [1]. With the advent of the concept of damage control orthopaedics, indications for application further expanded. However, there is still considerable variance among surgeons concerning external fixation application technique, indications, and after-care guidelines.
Techniques for the application of an external fixator vary greatly based on surgeon preference and anatomical location. External fixation as provisional or definitive stabilization of rotationally unstable pelvic ring injuries represents an important tool for trauma surgeons in adults and children and can even be applied in late open-book deformities [10, 11, 21, 36]. Pin purchase in the pelvic region can be obtained either by supra-acetabular or iliac crest placement, or even by a combination of the two. Although supra-acetabular pins have been shown to have increased biomechanical stability in several studies [12, 22], the degree of experience and preference of the treating physician, as well as other external factors (e.g., morbid obesity and proximity of concomitant soft tissue injury), can lead to a variety of different application techniques. Although the recent advent of the internal subcutaneous fixator has decreased the use of external pelvic fixation, its use is still widespread due to the application difficulties and complications that may be associated with an infix [10, 11].
Similarly, there are multiple techniques described to avoid damage to the radial nerve when placing humeral external fixation pins. These can include adhering to a predefined safe zone, indirect blunt dissection/palpation, or mini-open approaches with direct visualization of the nerve [5, 19].
The aim of this study was to assess the preferences for external fixation application and management among German trauma surgeons registered with the German Trauma Society (DGU). Our objective was to investigate the use, management, and perception of external fixation, excluding variables such as adjacent soft tissue injuries, morbid obesity, and other external factors, which would otherwise cause deviation from typical use. We sought to further evaluate if a consensus exists among DGU surgeons, or if trends could be identified when taking surgeon experience and level I trauma status into consideration.
Materials and methods
We utilized the database of the German Trauma Society (DGU) to obtain contact information of its active members. Active members were then contacted via email and asked to participate in an online survey that included our questionnaire. If members did not reply to the invitation to fill out the survey, a reminder email was sent one additional time. The questionnaire was developed by the two senior authors, T.D and H-C.P, who have a combined practice experience of 43 years. The questionnaire was designed to encompass a wide range of external fixation topics based on variances seen throughout their years of clinical experience and commonly debated techniques in the literature.
Definitions
For the compilation of the questionnaire, the authors adhered to the following definitions:
-
1.
Polytrauma
A patient suffering two or more traumatic injuries resulting in an abbreviated injury severity (AIS) score ≥ 3 combined with at least one additional variable condition. These variables include age ≥ 70, hypotension, acidosis, and/or coagulopathy [32].
-
2.
Trauma centre level
These were adapted from the definition provided in the German Trauma Society trauma network. According to the DGU, level III trauma centres are equivalent to local community low-energy trauma centres, level II includes regional trauma centres, and level I trauma centres are considered to provide the highest level of trauma care with region-spanning collaboration with lower tier centres, with referrals, with transfers, and with upgrades from both lower tier trauma centres and non-trauma hospitals.
The distributed version of the questionnaire included 14 questions grouped into three subsections. In the first subsection, the questionnaire asked for the responder’s demographic information and workplace environment. This included job title/position, background and degree of specialty training, years of clinical experience, and the identified level of the surgeon’s primary trauma centre. In the second subsection, items 5 through 11 contained questions dealing with general preferences for the application and management of external fixators. This covered a wide-range of topics including the likelihood and frequency of use of pre-operative template sketches or plots, use of intra-operative fluoroscopy, pin-site tract infection prophylaxis, environment for external fixation removal, and time to definitive surgery/fixation. The second subsection also queried the surgeon’s opinions regarding the major drawbacks of external fixation and priorities of application with regard to speed, reduction, and soft tissue management. In the third subsection, items 12 through 14 dealt with specific anatomic application techniques with one question each—including the humerus, pelvis, and ankle-spanning external fixators. For the humerus, the question was directed at protocols for avoiding radial nerve damage. With regard to the pelvis, the questions focused on supra-acetabular versus iliac crest versus combination pin-placement preferences. Finally, the ankle-spanning external fixation question inquired about the use of transcalcaneal pins and/or metatarsal pins for distal fixation and the role of fluoroscopy usage intra-operatively.
Nominal scales were utilized for all but two of the questions allowing responders to select from several predetermined single-choice options. The remaining two questions were assigned an ordinal scale where the responder was asked to rank their particular feeling towards the topic addressed. These two questions were in the second subsection of the questionnaire concerning the priorities and disadvantages of external fixation application, where the responders could assign the numbers 1 to 7 and 1 to 5, respectively, to reflect priorities and impact of the referenced options. The survey clearly designated the value of 1 as being the highest priority, with 7 and 5 being of the lowest priority, respectively.
Returned questionnaires were scrutinized for missing entries and data was collected and entered into an Excel spreadsheet (Microsoft, Redmond, Washington, USA).
Statistical analysis
Data stored in the Microsoft Excel file was then transferred to SPSS version 23.0 (IBM, Chicago, Illinois, USA) for statistical analysis. Questions that were designed for single-choice responses were further evaluated for potential significant differences among surgeons at different levels of trauma centres and among differing levels of surgeon position. We further grouped surgeons from different trauma centre levels into two main groups. The first group was comprised of surgeons who identified their primary workplace as a level I trauma centre, while the second group was comprised of surgeons from primarily level II trauma centres and below.
In a separate analysis, we subdivided the responses from those that were identified as department chairmen and compared them to all other responders. Preliminary crosstabs with a chi-square test were performed to test for independence between the categorical parameters and to analyze question responses for significant differences. With the contingency tables being lager than 2 × 2, follow-up subtables were created and tested with the chi-squared test and the Fischer test to evaluate whether significant differences between levels of trauma centre or position of the surgeon existed.
Results
The questionnaire was distributed to the entirety of the DGU, which comprised 375 hospitals at the time of the survey. A total of 365 surgeons returned the survey with varying levels of completeness. Three-hundred eleven surgeons completed the full survey, an additional five surgeons completed the majority of the survey with the exception of site-specific application techniques, and the remaining 49 surgeons returned the survey with only identifying information and level of experience.
Demographic of responding hospitals and responders
Out of the 365 total responders, 110 identified themselves as the chairmen of their respective departments, 190 identified as attendings, 36 as fellows, and the remaining 29 identified as surgical residents. The vast majority of responders had more than ten years of experience. In contrast, only 7.7% of responders considered themselves to be “in training”. The majority of surgeons (42.7%) identified their primary work environment as a level I trauma center, while level II and level III trauma centers comprised 29.9 and 18.4% of responders, respectively. Participants’ demographics are summarized in Fig. 1.
General considerations in external fixation application
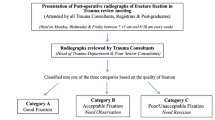
With regard to pre-operative planning, 93% of responding surgeons indicated that they do not routinely draw or plot a physical pre-operative template. For intra-operative control, 96.5% of responders indicated a preference for the use of fluoroscopy in at least two orthogonal planes, as opposed to only one view or no fluoroscopy use all together. Responses to techniques for mitigating the incidence of pin-tract infections showed only 41.1% of surgeons provide patients with specific training in the inpatient setting on how to avoid hardware infections. An even smaller percentage (8.5%) confirmed the presence of written instructions for pin-site care protocols to prevent infections. Removal of external fixation pins was predominantly preferred with an awake patient under local or no analgesia in an outpatient clinic setting (59.5%). Responders chose major soft tissue trauma as the main indication for external fixation application. Time to conversion surgery was overwhelmingly dependent on the condition of soft tissues (94.0%). Outcomes of general questions regarding external fixation usage are displayed in Fig. 2.
Ranking of external fixation disadvantages and priorities
When surgeons were asked to rank drawbacks of external fixation, pin-tract infections were unanimously ranked as the primary disadvantage. The most inconsequential disadvantage of external fixation among responders was a decreased quality of computed-tomography (CT) scans with external fixators in place. Regarding indications, overwhelming importance was attributed to prevent further insult to the soft tissues in the acute setting. Adherence to predefined application standards ranked lowest on the list of priorities.
Region-specific habits
The majority of responders (64.6%) indicated a preference for supra-acetabular pin placement with regard to pelvic external fixation application. In the upper extremity, careful blunt dissection and mini-open approaches with direct visualization were similarly utilized with 39.2 and 33.1%, respectively, to prevent inadvertent nerve injury when placing humeral pins. For ankle-spanning external fixation, 75.9% of surgeons prefer transcalcaneal pin placement when possible. 98.1% of these responders also indicated the use of intra-operative fluoroscopy was preferred to assess articular reduction of the ankle joint. No consensus was reached regarding the placement locations of the distal pins over the foot. An overview of region-specific habits is shown in Fig. 3.
Comparative results
Surgeons in a level I trauma centre were more likely to directly provide specific instructions to patients with regard to self-guided pin-site care compared to the rest of responders (54.5 vs. 31.3%, p = 0.0001). For region-specific application techniques, level I trauma surgeons were also more likely to opt for a mini-open approach for visualization of the radial nerve (42.4% vs. 26.3%, p = 0.003) and more likely to favour supra-acetabular pin placement (75.8% vs. 45.3%, p = 0.0001) than their level II and level III trauma centre colleagues. In addition, this level I surgeon cohort was less apt to indicate that pin-site care was primarily the nurse’s responsibility (21.7% vs. 36.8% p = 0.004).
Participants identified as department chairmen more commonly adhered to a predefined pin-site care protocol compared to the rest of their colleagues (16.7% vs. 5.3%, p = 0.003) and were more likely to remove external fixators in the operating theatre setting without general anaesthesia (15.6% vs. 4.9%, p = 0.004).
Discussion
External fixation indications, techniques, and management vary greatly among different regions around the globe, and as demonstrated here, even among different surgeons in the same region. Properly applied external fixators represent an important tool for any trauma surgeon, since their first introduction at the end of the nineteenth century in the USA by Clayton Parkhill or at the beginning of the twentieth century by the Belgian Albin Lambotte [15]. Its utility in treating open fractures alone has been quantified ranging from 29% in Gustilo type I injuries to 93% in Gustilo type III injuries [14]. Though the indications for external fixation have expanded with the damage control concept, it is important to note that its use has decreased in other specific applications, such as in the case of distal radius fractures. Jo et al. showed external fixation use has decreased to only 16% with the advent of angular stable fixation of the distal radius [18]. However, this does not mean that external fixation has gone out of style and is still an active topic of research being combined with modern techniques [35].
Because its overall popularity still persists, we sought to evaluate if a widespread consensus for the application and management of external fixation exists among German trauma surgeons.
Results were mixed with a majority of surgeons agreeing in a few aspects and others with a more balanced response.
Reported standards
Intra-operative orthogonal radiographs in a minimum of two planes are widely accepted and seem to be the gold standard for intra-operative quality control. With regard to anatomical region-specific habits in external fixation, we were able to identify two areas where a clear majority was in agreement. The first of these was the preference for a transcalcaneal pin when performing ankle-spanning fixation of the lower extremity, agreed upon by 75.9% of responding surgeons. The other was the preference for supra-acetabular only pin construct for the pelvis, with 64.6% in agreement, compared to 12% of surgeons opting for pin placement only in the iliac crest. Not surprisingly, this habit is in line with the literature demonstrating the superior biomechanical stability of pin constructs with pins in the supra-acetabular osseous pathway [12, 22].
No consensus reached
Interestingly, no consensus was reached regarding the preferred method for placing pins in the distal humerus, where the radial nerve is a known at risk structure ([3, 28]. Both mini-open approaches with direct visualization of the radial nerve and blunt dissection with palpation down to the bone were similarly accepted. Clement et al. was able to show variations in the course of the radial nerve in the distal third of the humerus with an injury rate of 10% caused by pins transfixing the nerve. These observations led the authors to recommend mini-open approaches with visualization of the nerve to avoid such injuries [5]. Several authors have also tried to define lateral “safe zones” for pin placement relative to distances defined by the transepicondylar width [2, 19]. The predefined “safe zones” to avoid radial nerve injuries as described by these authors seem less popular among our responders [38].
The preferred method for prevention of pin-tract infections was another topic where physicians were not in general agreement. Although pin-tract infections were ranked as the highest drawback with external fixation treatment in our survey, predefined protocols for infection prophylaxis seem to be the exception. Looking at the literature, this should not come as a surprise. Numerous studies contradict each other in topics of pin-site care, ranging from frequency [4, 42] and method of pin care [9, 13, 23, 33, 41] to various pin coatings [6,7,8, 26, 27, 44]. It is therefore not surprising that subsequent Cochrane systematic reviews found that high-quality studies concerning pin-tract infections are still missing and that there is insufficient evidence to formulate a standardized protocol to prevent pin-site infections [24, 25]. This is further impeded by the fact that there is a lack of a universally accepted definition of a pin-tract infection, making it difficult to compare results from different studies and form a consensus. Nevertheless, numerous protocols have been proposed in an attempt to help prevent the occurrence of pin-site infections and improve the ability to safely convert to definitive surgery [16, 20].
It is unclear whether there are distinct differences between the German and other international standards. It is certainly evident that the use of external fixators is variable within Europe, and even within Germany. Historically, some centers in Germany have performed extensive use of external fixation, even in cases amenable to an intramedullary nail [43]. In general, reamed-locked nailing is foreseen for long-bone fractures without the use of external fixation. Only in cases with severe soft tissue injuries, or polytrauma in uncertain condition, an initial external fixator is recommended [31]. There are distinct standards for the conversion of an ex fix into a reamed-locked nail. The protocol entails redraping and reprepping in order to minimize the risk of infection [16]. In western societies, trauma systems often are advantageous as they provide dedicated trauma operating rooms, thus allowing for rapid and easy use of external fixation [40]. In others, this may not so easily be obtainable [29].
A major strength of our study was the response rate of 316 surgeons in the DBU that were willing to participate. On the chairman level, we also had the benefit of a broad demographic distribution with regard to trauma centre level among responders. This allowed us to better understand the preferences and standard operating procedures of the whole spectrum of trauma hospitals, not just confined to level I centres.
One limitation of the study was that the most common demographic among responding surgeons was senior-level physicians at level I trauma centres. This likely can be attributed to the increased interest in research in these institutions, but this is speculative. This does, however, allow us to better understand standard operating procedures preferred by attendings and chairmen at level I facilities, but potentially under-represents a major group of surgeons also performing external fixation in the community as well as physicians in training, such as residents and fellows.
Given the limitations mentioned above, we feel that the following conclusions are justified:
-
1.
There seems to be a weak consensus on core issues and prevention methods for complications involving external fixation. This especially includes pin-tract infection prophylaxis.
-
2.
Written-down protocols and standard operating procedures are the exception.
-
3.
It is unclear whether the lack of standardization of application and management has an impact on patient outcomes.
Further studies are needed to evaluate the association between the application and management habits with the clinical outcomes of patients. If outcomes were to diverge, efforts should be undertaken to standardize external fixator use, and cooperation between lower and higher tier trauma centres should be encouraged.
Conclusion
Although the use of external fixation is widespread and established among trauma surgeons in Germany, there are substantial differences in application technique and management. A wider consensus and cooperation between trauma centres of varying levels might be necessary to achieve standardization to optimize care and better prevent complications in the future. This might further entail that principles of external fixation may be worth undergoing further assessment to allow for better standardization.
References
Alrabai HM, Gesheff MG, Conway JD (2017) Use of internal lengthening nails in post-traumatic sequelae. Int Orthop 41(9):1915–1923
Bloom T, Zhao C, Mehta A, Thakur U, Koerner J, Sabharwal S (2014) Safe zone for superolateral entry pin into the distal humerus in children: an MRI analysis. Clin Orthop Relat Res 472(12):3779–3788
Caldwell JM, Kim HM, Levine WN (2013) Radial nerve injury associated with application of a hinged elbow external fixator: a report of 2 cases. J Shoulder Elb Surg 22(3):e12–e16
Cavusoglu AT, Er MS, Inal S, Ozsoy MH, Dincel VE, Sakaogullari A (2009) Pin site care during circular external fixation using two different protocols. J Orthop Trauma 23(10):724–730
Clement H, Pichler W, Tesch NP, Heidari N, Grechenig W (2010) Anatomical basis of the risk of radial nerve injury related to the technique of external fixation applied to the distal humerus. Surg Radiol Anat 32(3):221–224
Coester LM, Nepola JV, Allen J, Marsh JL (2006) The effects of silver coated external fixation pins. Iowa Orthop J 26:48–53
Collinge CA, Goll G, Seligson D, Easley KJ (1994) Pin tract infections: silver vs uncoated pins. Orthopedics 17(5):445–448
DeJong ES, DeBerardino TM, Brooks DE, Nelson BJ, Campbell AA, Bottoni CR, Pusateri AE, Walton RS, Guymon CH, McManus AT (2001) Antimicrobial efficacy of external fixator pins coated with a lipid stabilized hydroxyapatite/chlorhexidine complex to prevent pin tract infection in a goat model. J Trauma 50(6):1008–1014
Egol KA, Paksima N, Puopolo S, Klugman J, Hiebert R, Koval KJ (2006) Treatment of external fixation pins about the wrist: a prospective, randomized trial. J Bone Joint Surg Am 88(2):349–354
Fang C, Alabdulrahman H, Pape HC (2017a) Complications after percutaneous internal fixator for anterior pelvic ring injuries. Int Orthop 41(9):1785–1790
Fang C, Alabdulrahman H, Pfeifer R, Tarkin IS, Pape HC (2017b) Late reconstruction of severe open-book deformities of the pelvis - tips and tricks. Int Orthop 41(9):1777–1784
Gardner MJ, Nork SE (2007) Stabilization of unstable pelvic fractures with supraacetabular compression external fixation. J Orthop Trauma 21(4):269–273
Gordon JE, Kelly-Hahn J, Carpenter CJ, Schoenecker PL (2000) Pin site care during external fixation in children: results of a nihilistic approach. J Pediatr Orthop 20(2):163–165
Gumbel D, Matthes G, Napp M, Lange J, Hinz P, Spitzmuller R, Ekkernkamp A (2016) Current management of open fractures: results from an online survey. Arch Orthop Trauma Surg 136(12):1663–1672
Hernigou P (2017) History of external fixation for treatment of fractures. Int Orthop 41(4):845–853
Horst K, Andruszkow H, Weber C, Dienstknecht T, Hildebrand F, Tarkin I, Pape HC (2015) Standards of external fixation in prolonged applications to allow safe conversion to definitive extremity surgery: the Aachen algorithm for acute ex fix conversion. Injury 46(Suppl 3):S13–S18
Hosny GA, Ahmed AA, Hussein MA (2018) Clinical outcomes with the corticotomy-first technique associated with the Ilizarov method for the management of the septic long bones non-union. Int Orthop. https://doi.org/10.1007/s00264-018-3924-9
Jo YH, Lee BG, Kim JH, Lee CH, Kim SJ, Choi WS, Koo JW, Lee KH (2017) National surgical trends for distal radius fractures in Korea. J Korean Med Sci 32(7):1181–1186
Kamineni S, Ankem H, Patten DK (2009) Anatomic relationship of the radial nerve to the elbow joint: clinical implications of safe pin placement. Clin Anat 22(6):684–688
Kazmers NH, Fragomen AT, Rozbruch SR (2016) Prevention of pin site infection in external fixation: a review of the literature. Strategies Trauma Limb Reconstr 11(2):75–85
Kenawey M (2017) Surgical considerations with the operative fixation of unstable paediatric pelvic ring injuries. Int Orthop 41(9):1791–1801
Kim WY, Hearn TC, Seleem O, Mahalingam E, Stephen D, Tile M (1999) Effect of pin location on stability of pelvic external fixation. Clin Orthop Relat Res (361):237–244
Lagerquist D, Dabrowski M, Dock C, Fox A, Daymond M, Sandau KE, Halm M (2012) Care of external fixator pin sites. Am J Crit Care 21(4):288–292
Lethaby A, Temple J, Santy J (2008) Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database Syst Rev (4):Cd004551
Lethaby A, Temple J, Santy-Tomlinson J (2013) Pin site care for preventing infections associated with external bone fixators and pins. Cochrane Database Syst Rev (12):Cd004551
Mason WT, Khan SN, James CL, Chesser TJ, Ward AJ (2005) Complications of temporary and definitive external fixation of pelvic ring injuries. Injury 36(5):599–604
Masse A, Bruno A, Bosetti M, Biasibetti A, Cannas M, Gallinaro P (2000) Prevention of pin track infection in external fixation with silver coated pins: clinical and microbiological results. J Biomed Mater Res 53(5):600–604
McKee MD, Bowden SH, King GJ, Patterson SD, Jupiter JB, Bamberger HB, Paksima N (1998) Management of recurrent, complex instability of the elbow with a hinged external fixator. J Bone Joint Surg (Br) 80(6):1031–1036
Oestern HJ, Garg B, Kotwal P (2013) Trauma care in India and Germany. Clin Orthop Relat Res 471(9):2869–2877
Pape HC, Hildebrand F, Pertschy S, Zelle B, Garapati R, Grimme K, Krettek C, Reed RL 2nd (2002) Changes in the management of femoral shaft fractures in polytrauma patients: from early total care to damage control orthopedic surgery. J Trauma 53(3):452–461 discussion 461-452
Pape HC, Rixen D, Morley J, Husebye EE, Mueller M, Dumont C, Gruner A, Oestern HJ, Bayeff-Filoff M, Garving C, Pardini D, van Griensven M, Krettek C, Giannoudis P (2007) Impact of the method of initial stabilization for femoral shaft fractures in patients with multiple injuries at risk for complications (borderline patients). Ann Surg 246(3):491–499 discussion 499-501
Pape HC, Lefering R, Butcher N, Peitzman A, Leenen L, Marzi I, Lichte P, Josten C, Bouillon B, Schmucker U, Stahel P, Giannoudis P, Balogh Z (2014) The definition of polytrauma revisited: an international consensus process and proposal of the new ‘Berlin definition’. J Trauma Acute Care Surg 77(5):780–786
Patterson MM (2005) Multicenter pin care study. Orthop Nurs 24(5):349–360
Patterson MJ, Cole JD (1999) Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma 13(2):85–91
Qiao F, Li D, Jin Z, Hao D, Liao Y, Gong S (2016) A novel combination of computer-assisted reduction technique and three dimensional printed patient-specific external fixator for treatment of tibial fractures. Int Orthop 40(4):835–841
Riemer BL, Butterfield SL, Diamond DL, Young JC, Raves JJ, Cottington E, Kislan K (1993) Acute mortality associated with injuries to the pelvic ring: the role of early patient mobilization and external fixation. J Trauma 35(5):671–675 discussion 676-677
Sasaki G, Watanabe Y, Takaki M, Yasui Y, Miyamoto W, Kawano H, Matsushita T (2017) Chipping and lengthening over nailing technique for femoral shaft nonunion with shortening. Int Orthop 41(9):1859–1864
Scaglione M, Fabbri L, Dell’ Omo D, Goffi A, Guido G (2015) The role of external fixation in the treatment of humeral shaft fractures: a retrospective case study review on 85 humeral fractures. Injury 46(2):265–269
Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr (2004) A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 18(8 Suppl):S32–S38
Sturm JA, Pape HC, Dienstknecht T (2013) Trauma care in Germany: an inclusive system. Clin Orthop Relat Res 471(9):2912–2923
W-Dahl A, Toksvig-Larsen S (2004) Pin site care in external fixation sodium chloride or chlorhexidine solution as a cleansing agent. Arch Orthop Trauma Surg 124(8):555–558
W-Dahl A, Toksvig-Larsen S, Lindstrand A (2003) No difference between daily and weekly pin site care: a randomized study of 50 patients with external fixation. Acta Orthop Scand 74(6):704–708
Weise K, Hontzsch D (1988) Change in the procedure following external fixation--osteosynthesis in closed and 1st to 2d degree open tibial fractures. Z Unfallchir Versicherungsmed Berufskr 81(2):93–104
Zhang E, Li F, Wang H, Liu J, Wang C, Li M, Yang K (2013) A new antibacterial titanium-copper sintered alloy: preparation and antibacterial property. Mater Sci Eng C Mater Biol Appl 33(7):4280–4287
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tiziani, S., Dienstknecht, T., Osterhoff, G. et al. Standards for external fixation application: national survey under the auspices of the German Trauma Society. International Orthopaedics (SICOT) 43, 1779–1785 (2019). https://doi.org/10.1007/s00264-018-4127-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4127-0