Abstract
Purpose
Closed reduction and spica cast immobilization are routinely used for young patients with developmental dysplasia of the hip with reducible hips. Our primary objective was to assess the interpretation quality of immediate post-operative pelvis radiographs after treatment.
Methods
A series of 28 randomly selected patients (30 hips) with pre- and post-operative pelvis radiographs and post-operative magnetic resonance imaging were included. Each was presented twice with an interval of two weeks, in alternating orders. Raters with different experience and specialties from different institutions rated the quality of reduction (hip in or out) after treatment.
Results
Thirteen surgeons and three radiologists evaluated 30 hips (28 patients). Agreement was not satisfactory (κ = 0.12). Experienced clinicians demonstrated similar agreement to inexperienced raters (κ = 0.04). Consistency at a two week interval was moderate (κ = 0.48, percent of agreement at 82%). The mean number of errors from the two ratings were 8.6 ± 2.5 and 8.9 ± 2.7, respectively (P = 0.72). There was no significant difference between surgeons with different levels of experience; radiologists did better than surgeons, but the difference was insignificant. Raters from different institutions had similar performance in poor judgment.
Conclusions
Our results show poor concordance between observers and ratings. Post-operative radiographs are unreliable for assessing the quality of hip reduction. The level of experience, subspecialty, and geographical origin do not impact the radiographic assessment. Based on the present findings, we recommend performing post-operative magnetic resonance imaging rather than anteroposterior pelvis radiograph to assess the hip. Compared to standard radiographs, magnetic resonance imaging allows more reliable interpretation while decreasing radiation exposure.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Closed reduction (CR) and spica cast immobilization are routinely used in the treatment of patients aged six to 18 months with developmental dysplasia of the hip (DDH) with reducible hips [1]. Some authors have shown that post-operative magnetic resonance imaging (MRI) is helpful in detecting hips that remain dislocated after CR and spica cast immobilization [2,3,4,5]. Moreover, it has also been shown that MRI correlates well with arthrography performed immediately prior to CR [6,7,8]. Despite the fact that several studies have highlighted the validity of MRI, none have focused on the reliability of plain radiograph assessment after CR and spica cast immobilization, notwithstanding the fact that radiograph interpretation can extensively affect the diagnosis and treatment of patients with DDH [8]. Additionally, the quality of plain radiograph interpretation can also be influenced by external factors, such as experience and subspecialty training, as has been shown by several studies performed on different sets of radiographs taken for other diseases [9,10,11].
The primary objective of this study was to assess the interpretation quality of immediate post-operative anteroposterior (AP) pelvis radiographs of children undergoing CR and spica cast immobilization for DDH. We aimed to evaluate intra- and inter-observer reliability among raters of different levels of experience, specialties, and institutions. We hypothesized that compared to less experienced raters, more experienced raters would score better regardless of subspecialty training or background.
Materials and methods
After securing IRB approval from our institution (n. 2017102307), a series of 28 randomly selected patients (30 hips) with pre- and post-operative AP pelvis radiographs and post-operative MRI were included.
The inclusion criteria were (a) age between six and 18 months; (b) diagnosis of unilateral or bilateral DDH confirmed by pre-operative AP pelvis radiographs; (c) treatment by hip arthrogram, CR and spica cast immobilization; (d) an exploitable set of pre- and post-operative AP pelvis radiographs; and (e) a post-operative MRI performed no later than 36 hours after index surgery.
Patients not meeting all inclusion criteria (a through e) and those with teratologic, syndromic, or neuromuscular hip dislocation were excluded.
Rater selection and grouping
Participants included 16 raters with different levels of experience and subspecialties (13 paediatric orthopaedic surgeons and 3 radiologists) from 2 different institutions, one from Asia and one from Europe. Paediatric orthopaedic surgeons were grouped according to their experience, per the number of years in clinical practice, and the geographical origin of their institution, Asia or Europe.
Raters from Institution 1 (Asia) were divided into three groups of three raters each: group A (raters 1, 2, and 3) included raters with less than five years of experience, group B (raters 4, 5, and 6) included raters with five to ten years of experience, and group C (raters 7, 8, and 9) included raters with more than ten years of experience.
Three paediatric radiologists with more than five years of experience and a special interest in musculoskeletal disorders from institution 1 (Asia) were included in group D (raters 10, 11, and 12).
Four paediatric orthopaedic surgeons with more than five years of experience from institution 2 (Europe) were included in group E (raters 13, 14, 15, and 16).
Radiographic assessment
The 28 selected AP pelvis radiographs (30 dislocated hips) were assigned to raters in random order. Each rater assessed hips on post-operative AP pelvis radiographs twice at a two-week interval, with radiographs presented in a different random order at each presentation (n = 60 evaluations).
Each post-operative AP pelvis radiograph was presented together with a vignette stating the patient’s age, gender, and diagnosis (i.e., 12-month-old female with left DDH) and with the pre-operative AP pelvis radiograph.
Raters were asked to rate each hip on post-operative AP pelvis radiograph as in (reduced) or out (dislocated).
MRI was used as the standard reference for the final assessment of hip joint reduction (in or out). All raters were blinded to MRI results during the rating process. Data were collected and analyzed by two researchers not involved in the care or imaging analysis of any of the included patients.
Statistical analysis
Statistical analysis was performed using Stata software (version 13, StataCorp LP, College Station, TX, US). The tests were two-sided, with the Type I error set at α = 0.05. Characteristics were presented as the mean ± standard deviation or median [interquartile range] for continuous data (assumption of normality assessed using the Shapiro-Wilk test) and as the number of patients and associated percentages for categorical parameters. Generalized linear mixed models (logistic) were carried out to compare percentage of errors made by raters according to the rating (first or second) and to the level of expertise, the specialty, and the geographic origin of raters. In these models, raters and patients are considered as random-effects in order to model between and within raters and patients variability. The kappa coefficient for correlated data and proportion accuracy (%) were calculated in order (1) to measure the inter observer reliability at the first rating and intra-observer reliability between first and second ratings, then (2) to compare results between observer’s evaluation and MRI at the first rating. According to the usual recommendations [12, 13], the concordance was examined as follows: < 0.2 (bad), 0.2–0.4 (low), 0.4–0.6 (moderate), 0.6–0.8 (good) and > 0.8 (excellent). Considering MRI as the standard reference, sensitivity and specificity were calculated and presented with 95% confidence intervals.
Results
Twenty-eight patients with unilateral (26 patients; 7 right, 19 left) or bilateral (2 patients) DDH, for a total of 30 dislocated hips, met the inclusion criteria. There were four male and 24 female patients with a mean age of 12 ± four months (range, 6–18). According to Tönnis classification, hips were rated as type 1 in one case, type 2 in eight cases, type 3 in 16 cases, and type 4 in five cases (Table 1).
Based on post-operative MRI findings, a total of 6 hips (6/30; 20%) were identified as out (dislocated) after arthrogram, CR, and spica cast immobilization.
Radiographic assessment
A total of 60 hips (30 for each rating) were reviewed twice by each of the 16 observers, for a total of 1920 ratings.
Overall, on average, raters misdiagnosed 8.6 ± 2.5 hips (range, 6–13) and 8.9 ± 2.7 hips (range, 5–14) in the first and the second rating, respectively. No significant difference was found between the first and the second rating or among all raters (P = 0.72). Table 2 shows the number and percentage of errors made by raters according to the level of expertise, specialty, and geographic origin of raters (Table 2). The level of experience (< 5, 5–10, and > 10 years of experience) and subspecialty training (orthopedic surgery versus radiology) of raters did not influence their performance, expressed as the number of errors/number of total ratings.
Table 3 shows inter- and intra-observer reliability of the post-operative X-ray in DDH patients in terms of agreement (%) and Cohen’s kappa. Agreement among all readers equals κ = 0.12 at first rating. Clinicians with less than ten years of experience demonstrated a similar level of agreement to raters with more than ten years of experience (κ = 0.04). Consistency was moderate when raters assessed hip reduction at a two week interval (κ = 0.48, percent of agreement at 82%). Overall, the sensitivity and specificity of post-operative AP pelvis radiographs with MRI as the standard reference were 32% [CI 23%–43%] and 81% [CI 77%–85%], respectively.
Discussion
This article aimed to assess the quality and reliability of the interpretation of post-operative AP pelvis radiographs of children treated by CR and spica cast immobilization for DDH. This study forced raters to evaluate each hip as reduced (hip in) or dislocated (hip out) in a homogeneous set of radiographs.
Our findings demonstrate that AP pelvis radiographs taken after closed reduction and spica cast immobilization are frequently misjudged, regardless of the level of experience, subspecialty training, and geographic origin of the rater. In particular, the mean overall misjudgment rate was 29.3% (range, 16.7–46.7%). Additionally, the low sensitivity and moderate specificity of the post-operative radiographic assessment (with MRI as standard reference) pushed forward the idea that AP pelvis radiographs alone, taken after cast immobilization, are probably inadequate to consistently evaluate if the hip is well reduced or not. Thus, MRI must be used as the standard reference for hip reduction and is required to post-operatively assess patients undergoing CR for DDH (hip in or out).
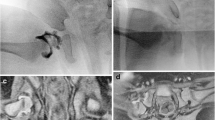
Our data provide a basis to assert that hip radiographs that have produced previous discordant interpretations continue to produce discordance on secondary review, in all groups of raters. Some hips are likely at a higher risk of being wrongly rated. In particular, we found that among misjudged hips, 8 were consistently wrongly rated by at least eight out of the 16 raters (50%) on both ratings. Among these hips, five (62.5%) were rated as in (reduced) although they were posteriorly dislocated on MRI (out) (Fig. 1). The remaining three hips (37.5%) were interpreted as out (dislocated) although MRI proved them to be in (reduced) (Table 4) (Fig. 2). These findings lead to the conclusion that approximately one hip out of four is at risk of being wrongly rated, regardless of the experience, subspecialty training, and geographic origin of the raters (Tables 2 and 3) (Fig. 3).
Why is the error rate so high? One reason could be that AP pelvis radiographs provide only frontal plane images. Raters often missed posteriorly dislocated hips. It could be hypothesized that AP radiographs give raters the impression that the hip is reduced (hip in) in the frontal plane, although it is out in the coronal view. Moreover, if the hip is not perpendicular to the source of radiation, the projected image may lead the rater to a false interpretation. We feel that it is very difficult to place the hip perpendicularly to the source of radiation due to multiple factors, such as the amount of hip abduction and rotation, asymmetry of the spica cast, and positioning of the patient [14]. Hence, radiological signs of reduction, such as Shenton’s line, medial pool distance, femoral head-acetabulum distance, and the axis of the femoral neck going to the triradiate cartilage may not be always reliable [15, 16]. In particular, in some patients, the axis of the femoral neck did not go through the triradiate cartilage centre in the radiograph: hips were rated as out although the MRI showed them to be in (reduced). Similarly, in other patients, Shenton’s line was broken on AP pelvis radiographs, and the hip was rated as out although the MRI showed the hip to be in (reduced).
A second reason could be related to the amount of contrast used for the intra-operative arthrogram. It is possible that if contrast diffuses around the joint or if too much product is used, the radiographic assessment could be more challenging and more prone to misjudgment. This seems to be particularly true when raters base their judgment on the femoral head-acetabulum distance, normally less than 4 mm [17, 18], and/or the “spur” sign, as described by Bowen [19]. Therefore, the quality of the arthrogram is important, and the amount of contrast should probably be standardized in order to avoid confounding post-operative radiographs.
Moreover, if the cast is too thick and/or is not totally radio-transparent (i.e., plaster of Paris), it might create difficulties for raters to evaluate whether the hip is in or out. In this respect, 10 out of the 16 raters (62.5%) consistently misjudged a patient immobilized in plaster of Paris (patient 26; Table 1). It is well known that plaster of Paris can be well molded; however, synthetic material has the advantage of better transparency [20].
In summary, all of the above influence the quality of radiographs and their subsequent readability.
This study has some limitations. It is a preliminary study based on radiographs of patients presenting at a single institution. Moreover, the relatively low number of radiographs did not allow the inclusion of a balanced distribution of DDH configurations.
Despite these limitations, this is the first study documenting board-certified clinicians of different levels of expertise, subspecialties, and geographical origins having low agreement when assessing hip reduction on post-operative AP pelvis radiographs of children aged six to 18 months with DDH treated by CR and spica cast immobilization.
In conclusion, post-operative AP pelvis radiographs alone appear to be inadequate to assess if the hip is reduced (hip in) or dislocated (hip out). In contrast with our hypothesis, experience and subspecialty are not protective for avoiding errors. An MRI after closed reduction and immobilization is mandatory. Institutions without MRI equipment should be very cautious in treating such patients and should eventually refer them to tertiary medical centers with MRI.
Based on the present findings, we recommend performing post-operative MRI rather than AP pelvis to assess whether the hip is reduced or not. Compared to standard radiographs, MRI allows more reliable interpretation while decreasing radiation exposure.
References
Malvitz TA, Weinstein SL (1994) Closed reduction for congenital dysplasia of the hip. Functional and radiographic results after an average of thirty years. J Bone Joint Surg Am 76(12):1777–1792
Desai AA, Martus JE, Schoenecker J, Kan JH (2011) Spica MRI after closed reduction for developmental dysplasia of the hip. Pediatr Radiol 41(4):525–529. https://doi.org/10.1007/s00247-010-1965-3
Dibello D, Odoni L, Pederiva F, Di Carlo V (2017) MRI in postreduction evaluation of developmental dysplasia of the hip: our experience. J Pediatr Orthop https://doi.org/10.1097/BPO.0000000000001037.
Ge Y, Cai H, Wang Z (2016) Quality of reduction and prognosis of developmental dysplasia of the hip: a retrospective study. Hip Int 26(4):355–359. https://doi.org/10.5301/hipint.5000348
Starr V, Ha BY (2014) Imaging update on developmental dysplasia of the hip with the role of MRI. AJR Am J Roentgenol 203(6):1324–1335. https://doi.org/10.2214/AJR.13.12449
Jaremko JL, Wang CC, Dulai S (2014) Reliability of indices measured on infant hip MRI at time of spica cast application for dysplasia. Hip Int 24(4):405–416. https://doi.org/10.5301/hipint.5000143
Gans I, Sankar WN (2014) The medial dye pool revisited: correlation between arthrography and MRI in closed reductions for DDH. J Pediatr Orthop 34(8):787–790. https://doi.org/10.1097/BPO.0000000000000187
Aoki K, Mitani S, Asaumi K, Akazawa H, Inoue H (1999) Utility of MRI in detecting obstacles to reduction in developmental dysplasia of the hip: comparison with two-directional arthrography and correlation with intraoperative findings. J Orthop Sci 4(4):255–263
Verma K, Sitoula P, Gabos P, Loveland K, Sanders J, Verma S, Shah SA (2014) Simplified skeletal maturity scoring system: learning curve and methods to improve reliability. Spine (Phila Pa 1976) 39(26):E1592–E1598. https://doi.org/10.1097/BRS.0000000000000653.
Zuckerman SL, Lakomkin N, Magarik JA, Vargas J, Stephens M, Akinpelu B, Spiotta AM, Ahmed A et al (2017) Evaluation of previously embolized intracranial aneurysms: inter- and intra-rater reliability among neurosurgeons and interventional neuroradiologists. J Neurointerv Surg. https://doi.org/10.1136/neurintsurg-2017-013231
Reem J, Carney J, Stanley M, Cassidy J (2009) Risser sign inter-rater and intra-rater agreement: is the Risser sign reliable? Skelet Radiol 38(4):371–375. https://doi.org/10.1007/s00256-008-0603-8
Fleiss JL, Cohen J (1973) The equivalence of weighted kappa and intraclass correlation coefficient as measures of reliability. Educ Psycol Meas 33:613–619
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33(1):159–174
Li Y, Guo Y, Li M, Zhou Q, Liu Y, Chen W, Li J, Canavese F, Xu H et al (2017) Acetabular index is the best predictor of late residual acetabular dysplasia after closed reduction in developmental dysplasia of the hip. Int Orthop. https://doi.org/10.1007/s00264-017-3726-5
Herring JA (1982) Inadequate reduction of congenital dislocation of the hip. J Bone Joint Surg Am 64(1):153
Race C, Herring JA (1983) Congenital dislocation of the hip: an evaluation of closed reduction. J Pediatr Orthop 3(2):166–172
Dimeglio A, Canavese F (2011) Imaging in Legg-Calvé-Perthes disease. Orthop Clin N Am 42(3):297–302. https://doi.org/10.1016/j.ocl.2011.04.003
Clohisy JC, Carlisle JC, Trousdale R, Kim YJ, Beaule PE, Morgan P, Steger-May K, Schoenecker PL, Millis M (2009) Radiographic evaluation of the hip has limited reliability. Clin Orthop Relat Res 467(3):666–675. https://doi.org/10.1007/s11999-008-0626-4
Forlin E, Choi IH, Guille JT, Bowen JR, Glutting J (1992) Prognostic factors in congenital dislocation of the hip treated with closed reduction. The importance of arthrographic evaluation. J Bone Joint Surg Am 74(8):1140–1152
Bitar KM, Ferdhany ME, Ashraf EI, Saw A (2016) Physical and clinical evaluation of hip spica cast applied with three-slab technique using fibreglass material. Malays Orthop J 10(3):17–20. https://doi.org/10.5704/MOJ.1611.008
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
No patients were involved. This is a retrospective study of patient’s data, and an IRB approval was obtained (2017102307).
Rights and permissions
About this article
Cite this article
Yong, B., Li, Y., Li, J. et al. Post-operative radiograph assessment of children undergoing closed reduction and spica cast immobilization for developmental dysplasia of the hip: does experience matter?. International Orthopaedics (SICOT) 42, 2725–2731 (2018). https://doi.org/10.1007/s00264-018-4038-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-4038-0