Abstract
Purpose
Rotator cuff tears (RCT) are a common source of pain and disability of the shoulder and are frequently combined with pathology of the long head of the biceps tendon (LHBT). The aim of this study was to evaluate the long-term results (5–10 years) of arthroscopic debridement of the rotator cuff with or without tenotomy of the LHBT in patients with irreparable rotator cuff tears.
Methods
Patient files between January 2005 and December 2010 were retrospectively reviewed. Suitable patients were contacted and invited to the outpatient clinic for assessment of their shoulder function by the constant score and were asked to fill out questionnaires, comprising the Oxford Shoulder Score (OSS), the SF-12, change in pain and function and satisfaction rate.
Results
The outcome measures of 39 patients with a mean age of 75.6 (SD 6.6) years were evaluated at a mean follow-up time of 6.5 (SD 1.5) years. All patients had filled out the questionnaires and 23 patients (59%) visited the outpatient clinic. The median corrected constant score for age and gender was 90 (P25-P75: 73–94). Twenty-six patients (67%) were satisfied with the result. No significant differences in outcome measures were found between patients treated solely with debridement and patients treated with debridement combined with tenotomy of the LHBT.
Conclusions
Both arthroscopic debridement and debridement combined with a bicepstenotomy yields high satisfactory shoulder function in elderly patients at long term.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rotator cuff tears (RCTs) are a common source of pain and disability of the shoulder [1,2,3]. The incidence of RCTs increases proportionately with age. When conservative treatment fails, operative treatment can be considered, and a range of available surgical interventions exist. However, there is no consensus concerning the preferred surgical treatment, especially in elderly patients or in case of an irreparable rotator cuff tear [4]. When possible, the rotator cuff will be repaired to improve the biomechanics of the shoulder. The success rate of repair depends on a variety of factors with a reported re-rupture rate of 20–65% [5, 6]. In case of irreparability, a variety of treatment options are available like tendon transfer, partial repair, hemiarthroplasty and reversed total shoulder arthroplasty [1, 2, 6, 7]. Also arthroscopic debridement and subacromial decompression can be beneficial [8]. Debridement is often combined with bicepstenotomy or tenodesis due to the association of RCTs with lesions of the long head of the biceps tendon (LHBT) [9,10,11]. Although tenodesis or tenotomy does not improve shoulder strength and possibly causes humeral head migration [12], the upward function is usually improved because of the relief of pain caused by mechanical impingement [4]. Even though early and midterm results are promising [12, 13], long-term results are still questioned [8, 13]. The primary aim of this study was to assess the long-term outcome of patients who have undergone arthroscopic debridement with or without a tenotomy of the LHBT in case of an irreparable RCT.
Materials and methods
Patients
Patients were retrospectively identified when treated by means of arthroscopic debridement of a full-thickness irreparable rotator cuff tear, with or without a tenotomy of the LHBT. Arthroscopic surgery was performed only after failed conservative treatment of at least six months consisting of physiotherapy, nonsteroidal anti-inflammatory medication and subacromial corticosteroid injections. All patients were surgically treated between January 2005 and December 2010. In case of a previous operation, recurrence operation, conversion to an open procedure or a simultaneous lateral clavicle resection, patients were excluded.
The study was approved by the local ethical committee, and informed consent of all patients to participate in the study was obtained.
Procedure
Suitable patients were asked for their willingness to complete questionnaires and to visit the outpatient clinic for physical examination. The questionnaires consisted of the Oxford Shoulder Score (OSS) [14], the 12 item short form health survey (SF-12) [15], and the visual analogue scale (VAS) for average pain, present during the last week. At the outpatient clinic, the Constant score (CS) was assessed [16]. To complete the CS, muscle strength and range of motion (ROM) of the shoulder were evaluated.
Rotator cuff tear
All patients had full-thickness and irreparable rotator cuff tears. A RCT was recorded as “irreparable” if it could not be repaired back to the rotator cuff footprint [8]. The decision not to repair was based on the presence of one or more of the following criteria: retraction of more than 50 mm, superior humeral head migration with an acromio-humeral distance of less than 7 mm and substantial cuff muscle atrophy or fatty infiltration (Goutallier stage 3 or 4) [17], when MRI was available. The final decision to repair was based on per-operative findings of medial tendon retraction past the superior border of the glenoid and/or poor tissue quality.
Operative technique
The procedure was performed by two experienced orthopaedic shoulder surgeons. Patients were treated with glenohumeral arthroscopy by use of general anaesthesia with or without an interscalene anaesthesia. Surgery was performed with the patient in beach-chair position. Posterior, antero-superior and antero-lateral portals were used. The avascular tendon edges were debrided in all cases. When the LHBT was degenerative, strongly widened/flattened or partial ruptured, a tenotomy was performed by sectioning the tendon at its origin at the supraglenoid tubercle and superior labrum. When necessary, debridement was combined by a (partial) bursectomy or acromioplasty (without resection of the coracoacromial ligament). In case of a pre-operative ruptured tendon, the remaining intra-articular parts of the biceps tendon were debrided and removed from the superior labrum. Hospital admission was at least 24 hours. Patients started with exercises under supervision of a physiotherapist directly post-operative. For pain relief, patients were allowed to use a collar and cuff for a maximum of 6 weeks. After discharge, patients were referred to a physiotherapist and were immediately allowed to start with active and active assisted shoulder range of motion in all directions.
Outcome measures
Patients visiting the outpatient clinic were assessed by use of the Constant score (CS) [16]. Active range of motion was measured by a goniometer, and strength by a dynamometer (microfet2 – Hoggan scientific, Salt Lake City, USA) using the average score of three measurements. Additionally, due to the advanced age of this group, the age- and gender-corrected Constant score was calculated [18]. The results were graded as excellent (90 to 100 points), good (80–89 points), fair (70–79 points) or poor (less than 70 points) [19]. Good and excellent Constant scores were considered satisfactory. Fair and poor Constant scores were considered unsatisfactory.
Other outcome measures included the Oxford Shoulder Score (OSS) [14], a general Short Form Health Survey (SF-12) [20], a Visual Analogue Scale (VAS) for average pain last week, and a questionnaire concerning satisfaction rate and change in daily life shoulder function. The OSS is a joint-specific patient reported outcome score which contains 12 items to score from 1 to 5. The total sum score ranges from 12 (best) to 60 (worst). The score was categorised as excellent (12–23), good (24–35), fair (36–47) or poor (48–60). The SF-12 score was compared to the mean score of the Dutch population [15].
Statistical analysis
Data were analysed using IBM SPSS Statistics for Windows, Version 22.0 (Armonk, NY: IBM Corp). Continuous variables were described as means with standard deviations (SD) in the case of a normal distribution; otherwise, as medians and interquartile ranges (IQR) were used. Categorical data were presented as frequencies with accompanying percentages.
For continuous data, differences in patient characteristics and clinical outcome measures between subgroups were compared using the Student’s t tests or the Mann Whitney U tests (MWU) according to their distributions. Pre- and post-operative values of clinical data (abduction, forward flexion and external rotation) were compared by use of paired t tests. Categorical variables were analysed by use of Chi2-tests or Fischer’s Exact test. The SF-12 of the study population was compared with normal values of the general population by using the Student’s t test.
The association between outcome measures was assessed by calculation of the Spearman correlation coefficient. A p value < 0.05 was considered statistically significant.
Results
Patient population
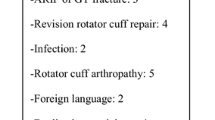
Between January 2005 and December 2010, 67 patients were arthroscopically treated for an irreparable full-thickness RCT. Out of these 67 patients, 48 (72%) were suitable for evaluation. The other 19 patients (28%) were excluded due to secondary surgery, conversion to an open procedure, prior surgery and death. All 48 patients were asked to fill out the questionnaires and were invited to the outpatient clinic for physical evaluation. Of these, 39 patients (85%) were willing to participate of which 23 (59%) were willing to visit the outpatient clinic. The other 16 patients (41%) completed the questionnaires without visiting the outpatient clinic (Fig. 1). The mean age at follow-up was 75.6 years (SD 6.6) with a mean follow-up time of 6.5 years (SD 1.5) (Table 1). Of all 39 patients, 22 (56%) were treated with debridement only. In 10 of these patients (45%), the LHBT had ruptured preoperatively. Seventeen patients (44%) were treated with debridement combined with tenotomy of the LHBT. Thus, post-operatively, the LHBT was absent in 27 patients (69%) and intact in 12 patients (31%).
Selection bias
To assess selection bias of the clinical results, differences between patients who visited the outpatient clinic and patients who solely filled out the questionnaires were evaluated (Table 1). Significantly more male (82%) than female patients (41%) visited the outpatient clinic (p = 0.01). No significant differences were observed with regard to time-to-follow up, age, acromioplasty and type of operation (debridement or debridement and tenotomy).
Except for the VAS score (p = 0.04) and the physical component score (PCS) of the SF-12 (p = 0.04), no significant differences were observed relating to the OSS and the mental component score (MCS) of the SF-12. Change in function, pain and satisfaction also showed no significant differences (Table 2).
Outcome measures
Constant score
The median Constant score (CS) was 77 (P25-P75: 63–85) (Table 2). The CS did not differ significantly between patients treated with debridement only and patients with debridement in combination with a bicepstenotomy (p = 0.69). No significant differences were observed between male and female patients (p = 0.27). The corrected CS for age and gender showed a median score of 90 (P25-P75: 73–94), with a satisfactory outcome of 72%. No significant difference was observed between male and female patients (p = 0.95). Like the uncorrected CS, the corrected CS did not differ significantly between patients treated with a debridement only and those with supplementary tenotomy of the LHBT (p = 0.95). Additionally, a positive correlation was detected between the corrected CS and the OSS (r = 0.84, p < 0.001).
Secondary outcome measures
Oxford Shoulder Score
The median of the OSS was 21.0 (IQR 17.0–27.0) with 12 patients (31%) achieving good results and 26 patients (67%) achieving excellent results.
SF-12
The median physical component score (PCS) was 42.5 (IQR: 30.4–51.1) and the median of mental component score (MCS) was 53.3 (IQR: 50.3–58.2). The PCS was significantly lower for patients who visited the outpatient clinic compared to patients who solely filled out the questionnaires (p = 0.04). The PCS was significantly lower (p < 0.001) compared to the normal values of the Dutch population while the MCS was not (p = 0.09) [15]. Additionally, no significant associations of the PCS were observed with gender or type of operation.
Pain, function and satisfaction
Of all 39 patients, 26 (67%) were satisfied, eight (20%) were neutral and five (13%) were dissatisfied. Patients who were dissatisfied did not differ from the rest of the series with regard to demographics or operative findings. Thirty-three (85%) patients reported improvement of their shoulder function and six (15%) patients did not experience any improvement (neutral/worse). Concerning pain, 34 patients (87%) reported improvement, whereas five patients (13%) did not experience improvement. The median (postoperative) VAS score was 2.0 (IQR 0.0–4.0). No other significant differences were found with regard to VAS score (Table 2).
Range of motion
With the numbers available, no significant differences were found between the pre-operative and follow-up range of motion for abduction, forward flexion and external rotation (p > 0.10 for all comparisons) (Fig. 2).
Discussion
In our study, we evaluated patients with an irreparable full-thickness RCT (n = 39) with a mean age of 76 years at a mean follow-up time of 6.5 years. Of all patients, 67% were satisfied with the result of the operation. Overall, 72% of the patients had a satisfactory shoulder function with a corrected Constant score of 80 points or more. Furthermore, the outcome measures and satisfaction of patients treated with debridement only are comparable with patients treated by debridement combined with tenotomy of the LHBT.
The fact that debridement without an attempt to repair can be successful for treatment in elderly patients with low physical demands has been established in the literature [8, 9, 12, 13, 21]. Also, the combination with tenotomy or tenodesis of the LHBT was reported to yield good clinical outcomes [22]. Our findings confirm the observations of previous studies. Slenker et al. [22], reviewed 16 studies with 433 tenodesis and 699 tenotomy procedures with comparably favourable results. In contrast to other previous studies, our study consisted of a relative old population [12, 23]. Assuming that the shoulder function deteriorates with age, the CS was corrected for age and gender. The median score for the corrected CS was still 90 and therefore higher or in accordance with scores reported in existing literature [13, 23, 24].
It is important to bear in mind the possible bias in this study. For example, we excluded eight patients because of secondary surgery. Six of them were not served by a debridement alone, and pain and disability of the shoulder persisted after surgery. These patients ultimately received a shoulder prosthesis at a mean time of 15 months (range 9–35 years). This implies that there is a failure rate in 12% of the patients who primarily have been treated with an arthroscopic debridement in case of a RCT. Additionally, there was a difference in patient population between patients who did and who did not visit the outpatient clinic, indicating selection bias. This might lead to an underestimation of the treatment effect, whereas the failures would overrate the treatment effect. Therefore, the results of this study are only valid for patients without secondary surgery.
Within the scope of this study, limitations are acknowledged. It was a retrospective study with a non-comparable group. The number of patients was small and conceivably too small to achieve significant validity; therefore, a bigger cohort would be needed. Due to the retrospective design, it was impossible to compare the pre-operative and post-operative shoulder strength in an objective manner. Furthermore, in this study, radiographic evaluation was not performed. This could have been of additional value since treatment of irreparable RCTs can be associated with progression of osteoarthritic changes in the glenohumeral joint [23]. However, the subjective experiences of the results after surgery are very useful and important to evaluate the success of an operation. Nevertheless, the strong aspect of this study was the long-term follow-up with a mean of leastways 6.5 years. In addition, we evaluated 81% of all suitable patients present in the database of our institution. A percentage that should provide reliable information about this treatment within this population.
Conclusion
According to the results of this study, both arthroscopic debridement alone and debridement combined with a tenotomy of the LHBT yield a high satisfactory shoulder function in elderly patients at long-term follow-up and can therefore be of additional value in the treatment of an irreparable rotator cuff tear.
References
Khair MM, Gulotta LV (2011) Treatment of irreparable rotator cuff tears. Curr Rev Musculoskelet Med 4:208–213. https://doi.org/10.1007/s12178-011-9098-3
Franceschi F, Papalia R, Vasta S et al (2015) Surgical management of irreparable rotator cuff tears. Knee Surg Sport Traumatol Arthrosc 23:494–501. https://doi.org/10.1007/s00167-012-2317-7
Kang JR, Sin AT, Cheung EV (2017) Treatment of massive irreparable rotator cuff tears: a cost-effectiveness analysis. Orthopedics 40:65–76. https://doi.org/10.3928/01477447-20160926-06
Bedi A, Dines J, Warren R (2010) Masssive tears of the rotator cuff. J Bone Joint Surg Am 92:1894–1908. https://doi.org/10.2106/JBJS.I.01531
Berth A, Neumann W, Awiszus F, Pap G (2010) Massive rotator cuff tears: functional outcome after debridement or arthroscopic partial repair. J Orthop Traumatol 11:13–20. https://doi.org/10.1007/s10195-010-0084-0
Chen K-H, Chiang E-R, Wang H-Y, Ma H-L (2017) Arthroscopic partial repair of irreparable rotator cuff tears: factors related to greater degree of clinical improvement at 2 years of follow-up. Arthroscopy 33:1949–1955. https://doi.org/10.1016/j.arthro.2017.06.047
Gerber C, Canonica S, Catanzaro S, Ernstbrunner L (2018) Longitudinal observational study of reverse total shoulder arthroplasty for irreparable rotator cuff dysfunction: results after 15 years. J Shoulder Elb Surg. https://doi.org/10.1016/j.jse.2017.10.037
Anley CM (2014) Arthroscopic treatment options for irreparable rotator cuff tears of the shoulder. World J Orthop 5:557. https://doi.org/10.5312/wjo.v5.i5.557
Szabo I, Boileau P, Walch G (2008) The proximal biceps as a pain generator and results of tenotomy. Sport Med Arthrose 16:180–186
Pill SG, Walch G, Hawkins RJ, Kissenberth MJ (2012) The role of the biceps tendon in massive rotator cuff tears. Instr Course Lect 61:113–120
Gerber C, Wirth SH, Farshad M (2011) Treatment options for massive rotator cuff tears. J Shoulder Elb Surg 20:S20–S29. https://doi.org/10.1016/j.jse.2010.11.028
Walch G, Edwards TB, Boulahia A et al (2005) Arthroscopic tenotomy of the long head of the biceps in the treatment of rotator cuff tears: clinical and radiographic results of 307 cases. J Shoulder Elb Surg 14:238–246. https://doi.org/10.1016/j.jse.2004.07.008
Kempf JF, Gleyze P, Bonnomet F et al (1999) A multicenter study of 210 rotator cuff tears treated by arthroscopic acromioplasty. Arthroscopy 15:56–66. https://doi.org/10.1053/ar.1999.v15.015005
Berendes T, Pilot P, Willems J et al (2010) Validation of the Dutch version of the Oxford shoulder score. J Shoulder Elb Surg 19:829–836. https://doi.org/10.1016/j.jse.2010.01.017
Mols F, Pelle AJ, Kupper N (2009) Normative data of the SF-12 health survey with validation using postmyocardial infarction patients in the Dutch population. Qual Life Res 18:403–414. https://doi.org/10.1007/s11136-009-9455-5
Constant CR, Murley AH (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164. https://doi.org/10.1097/00003086-198701000-00023
Goutallier D, Postel J-M, Bernageau J et al (1994) Fatty muscle degeneration in cuff ruptures (pre- and postoperative evaluation by CT scan). Clin Orthop Relat Res 304:78–83. https://doi.org/10.1097/00003086-199407000-00014
Katolik LI, Romeo AA, Cole BJ et al (2005) Normalization of the constant score. J Shoulder Elb Surg 14:279–285. https://doi.org/10.1016/j.jse.2004.10.009
Galatz LM, Griggs S, Cameron BD, Iannotti JP (2001) Prospective longitudinal analysis of postoperative shoulder function: a ten-year follow-up study of full-thickness rotator cuff tears. J Bone Joint Surg Am 83–A:1052–1056
Ware JE, Kosinski M, Keller SD (1996) A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 34:220–233. https://doi.org/10.2307/3766749
Rockwood C, Williams G, Burkhead W (1995) Débridement of degenerative, irreparable lesions of the rotator cuff. J Bone Joint Surg Am 77:857–866
Slenker NR, Lawson K, Ciccotti MG et al (2012) Biceps tenotomy versus tenodesis: clinical outcomes. Arthroscopy 28:576–582. https://doi.org/10.1016/j.arthro.2011.10.017
Liem D, Lengers N, Dedy N et al (2008) Arthroscopic debridement of massive irreparable rotator cuff tears. Arthroscopy 24:743–748. https://doi.org/10.1016/j.arthro.2008.03.007
Edwards TB, Walch G, Sirveaux F et al (2005) Repair of tears of the subscapularis. J Bone Joint Surg Am 87–A:725–730. https://doi.org/10.2106/JBJS.D.02051
Acknowledgments
All work presented was carried out by the four listed authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Pander, P., Sierevelt, I.N., Pecasse, G.A. et al. Irreparable rotator cuff tears: long-term follow-up, five to ten years, of arthroscopic debridement and tenotomy of the long head of the biceps. International Orthopaedics (SICOT) 42, 2633–2638 (2018). https://doi.org/10.1007/s00264-018-3991-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-018-3991-y