Abstract
Purpose
To evaluate mid- to long-term results after arthroscopic rotator cuff repair and to explore possible predictors of inferior outcome.
Methods
Patients treated for full-thickness supraspinatus and/or infraspinatus tears from 2004 to 2008, using a uniform single-row arthroscopic technique, were included in the study. Pre- and post-operative QuickDASH were used as the primary outcome measure, and VAS of pain, function and satisfaction were also collected. An additional questionnaire explored demographic and preoperative factors like onset and duration of symptoms, preoperative treatment and smoking habits.
Results
One hundred and forty-seven patients (82 %) were available at 6–9 years after surgery. All outcomes improved significantly from the preoperative values. A total of 8 % of patients had undergone additional surgery to the same shoulder during the follow-up period. Long-standing symptoms (>12 months) (P < 0.01), non-acute onset of symptoms (P < 0.01) and preoperative use of NSAIDs (P = 0.01) were correlated with inferior outcome at follow-up. No other factors investigated (i.e. gender, age, smoking and steroid injections) were found to affect the primary outcome (QuickDASH).
Conclusion
The current study is one of few reports of mid- to long-term outcomes after arthroscopic single-row repair of full-thickness rotator cuff tears. Global improvement in symptoms and function was found between the preoperative and the 6–9 years evaluation, and the technique therefore seems like a viable approach for treating tears of the supra- and the infraspinatus tendon. Several predictors of inferior long-term outcome after rotator cuff repair were, however, identified: preoperative use of NSAIDs, long-standing symptoms before surgery and non-acute onset of shoulder symptoms. In light of the current findings, accurate diagnosis and prompt treatment seem important in optimizing outcomes after rotator cuff surgery.
Level of evidence
IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Conditions related to the rotator cuff tendons are a major cause of disabling shoulder problems in the adult population [7, 28, 30]. For some patients, a non-operative treatment regime that may include NSAIDS, steroid injections and non-operative rehabilitation will reduce pain and improve function sufficiently [1, 4, 5, 20, 31]. Other patients need surgical intervention to regain proper shoulder function. An ongoing debate has yet to resolve what patient characteristics predict better outcomes for the different treatment options [6, 20, 22, 29]. Patient’s age, smoking status, tear size, localization and chronicity of the tear are amongst the factors that may be important for decisions about the type of treatment [21, 24, 26, 34, 39].
Arthroscopic rotator cuff repair has become one of the most common surgical procedures performed by orthopaedic surgeons. A study from NHS (National Health Service, UK) showed an increase in such repairs from approximately 4–40 patients per 100,000 over the last decade [16]. In the same time period, the USA has seen a similar rise, by about 141 % from 1996 to 2006 [10]. The surgical treatment comes with substantial costs as well as an increased risk of complications related to the surgery (as opposed to a non-operative treatment)—therefore, critical evaluation of the surgical approach seems warranted. The majority of published studies evaluate the patients’ short- to midterm outcome after treatment—there is therefore a substantial need for more long-term results to find the true effect after intervention in patients with rotator cuff tear [38].
Thus, the aim of the present study was to evaluate the mid- to long-term results after arthroscopic rotator cuff repair. Further, we wanted to explore for preoperative factors that could predict inferior result at the outcome evaluation. The hypotheses were (1) that surgical repair would improve function and provide good long-term outcome and (2) that patient demographics and preoperative history would make it possible identify a subset of patients with inferior outcome.
Materials and methods
All patients treated surgically—by suture anchors in single row—for a symptomatic, repairable, transverse full-thickness rotator cuff tear of the supraspinatus and/or infraspinatus tendon in the period from 2004 to 2008 at our institution were eligible for inclusion in the study. Tears requiring side-to-side sutures and/or a margin convergence technique were not included, and all revision surgery was also excluded. All surgeries were performed as day-case procedures by the senior author.
At the time of surgery, the patients reported, on a standardized questionnaire, what type of preoperative treatment they had received (non-operative rehabilitation or exercises, drugs or other treatment modalities), their current work status, sick leave (and duration of such), smoking status, duration of symptoms and characteristics of their initial symptoms (acute or insidious debut). At the follow-up evaluation, patients were again asked to report on their work status.
Outcome measures
The primary outcome measure was the disabilities of the arm, shoulder and hand outcome measure (DASH). Data were collected at the time of surgery and at the time of follow-up. The QuickDASH 11-item disability/symptom subset was used [3]. Each answer was graded from 0 to 4. The component total score, from 0 to 100, was calculated by multiplying the average score by 25. A higher score indicates greater disability. Outcome by QuickDASH was rated as excellent (<20 points), good (20–39 points), fair (40–60 points) or poor (>60 points) [32].
VAS of pain (0 = no pain, 100 = worst possible pain) and VAS of function (0 = useless, 100 = perfect function) were included as secondary outcomes at both times of evaluation [33]. In addition, a VAS of satisfaction with the result of the treatment (0 = very dissatisfied, 100 = very satisfied) was included at the final follow-up evaluation [18, 29, 37].
Surgical technique
Except for a few patients with an acute onset and severe symptoms, all patients were required to undergo a minimum of 3 months of physiotherapy and a home exercise programme before being considered for surgery. All surgeries were done arthroscopically assisted with a posterior approach for visualization and additional lateral and anterior portals as needed for instrumentation. A diagnostic glenohumorel arthroscopy was performed before switching into the subacromial space. The subacromial bursa was debrided using a soft tissue resector and a radiofrequency probe—and the rotator cuff was inspected. Thereafter, a wedge-shaped moderate acromioplasty was performed to relieve the rotator cuff of any mechanical symptoms.
A debridement of the footprint on the tuberculum majus was performed to facilitate tendon healing. The mobility of the ruptured tendon(s) was assessed prior to repairing the rotator cuff. The repair was performed with one-to-four titanium screw anchors (Fastin RC, Depuy Synthes, Raynham, USA), depending on the size of the tear. Post-operatively patients used a sling for 6 weeks. They were instructed in passive range of motion exercises and moved on to active exercises after 6 weeks guided by a physiotherapist. The Ethical Committee at our institution reviewed and approved of the study (Teres Bergen ID 2010-0110). All patients gave their informed consent prior to their inclusion in the study.
Statistical analysis
All data handling and statistical analysis were performed in SPSS 21.0.0.0 (SPSS Inc., Chicago, IL, USA). The a priori significance level was set to 0.05. Due to a skewness of the outcome data BCa bootstrap confidence intervals based on 10,000 bootstrap replications were used to estimate mean group differences. Further, independent samples t test was used when testing for inter-group differences in QuickDASH sorted by; gender, smoking status, above/below 60 years of age, acute onset of symptoms, preoperative NSAID treatment and preoperative cortisone injections. ANOVA testing was used for examination of differences in duration of symptoms before surgery and function stratified by the preoperative QuickDASH score. A post hoc power calculation showed that with a total sample size of 147 patients, using a significance level of 0.05 and a SD of 20, the statistical power for detecting a minimal difference of 10 points in QuickDASH was 87 %.
Results
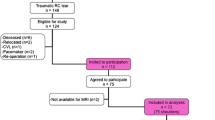
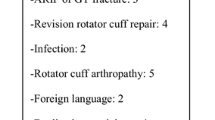
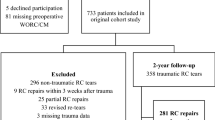
Of the 180 patients included in the study, 147 (82 %) were available for follow-up and were therefore evaluated at a mean of 7.5 (SD 1.1) years after the surgery. Demographic data are presented in Table 1. The length of the rotator cuff tear was found to be less than 1.5 cm in 9 % of patients, 1.5–2.5 cm in 68 % of patients and larger than 2.5 cm in 23 % of patients. One suture anchor was used for the repair in 77 % of patients and two or more in 23 %.
Secondary operations and complications
Twelve patients (8 %) underwent a new arthroscopic procedure to the same shoulder during the observation period due to a poor result. In eight cases, the rotator cuff tear was not healed (or a new tear had occurred); six of these had a new repair performed whereas two were considered irreparable. In three cases capsular release was performed to treat a long-standing post-operative frozen shoulder. In the last patient an acromioplasty was undertaken. Twenty-two patients (15 %) reported having experienced transient post-operative stiffness; four patients (2 %) had been treated for a superficial infection, while none had been treated for a deep infection.
Clinical outcomes
All outcome variables were found to improve significantly from preoperative evaluation to the long-term follow-up (Table 2). The mean QuickDASH did improve from 51 (SD = 20) to 14 (SD = 19, P = 0.001), the mean VAS function improved from 33 (SD = 24) to 84 (SD = 21, P = 0.001) and the mean VAS pain improved from 65 (SD = 22) to 15 (SD = 22, P = 0.001).
Predictors of long-term outcome
When comparing mean QuickDASH scores, neither gender, age above or below 60 years at time of surgery (49 % above 60), nor smoking habits (23 % smokers) were found to have any statistical significant differences (n.s.). Forty-four per cent of the patients reported to have an acute onset of their shoulder-related symptoms. This group was found to have significant better post-operative QuickDASH, mean 9 (SD 14) versus 18 (SD 20, P = 0.008), as compared to those with gradual onset of symptoms.
Outcomes (as reported in QuickDASH scores) related to preoperative use of steroids or NSAIDs are reported in Table 3. There was no difference (n.s.) in symptom’s duration between patients who received NSAIDs and those who did not. Neither was there any such difference (n.s.) between patients who had received steroids or not.
When analysing the post-operative QuickDASH dependent on the duration of symptoms before surgery, there was a clear trend towards worse outcomes in groups with long-standing symptoms (12–24 months and above 25 months) (Table 4). When comparing the post-operative results to preoperative function graded by QuickDASH as poor, fair, good or excellent (Table 5), those with a poor preoperative score (61 and above) had the worse outcome.
Discussion
The most important finding of the current study was the overall improvement in QuickDASH, VAS of pain and VAS of function from the preoperative evaluation to the long-term follow-up. Gradual onset, long history of symptoms and the use of NSAIDs predicted worse outcome in the patient population. Other potential preoperative predictors—like smoking, gender, age above/below 60 or preoperative steroid injections—were not found to correlate with an inferior outcome at the final evaluation.
There are relatively few long-term evaluations reporting on results after single-row rotator cuff repair, and to the best of our knowledge, the current study includes the largest number of patients to date. In a recent paper by Spennacchio et al. [37], a comprehensive review of 10 studies evaluating rotator cuff repair including a total of 483 patients was performed. The follow-up time spanned from a mean of 60–162 months, and the number of patients ranged from 26 to 115. Most patients were treated with a single-row technique, as in the current study, but some also had a mix of single- and double-row or other techniques. The type of rotator cuff lesions were heterogeneous, spanning from less severe PASTA lesions to full-thickness tears including subscapularis tendon tears. Evaluation was performed by a variety of outcome measures [i.e. American Shoulder and Elbow score (ASEAS), University of California, Los Angeles Score (UCLA), SF-36 (Short-Form version 36) and visual analogue score (VAS)]. Two of the studies evaluated the patency of the rotator cuff repair by means of ultrasound (US) [17, 27].
Of the studies included in the review, only the one by Gulotta et al. [17, 27] seems to have a patient population comparable to that in the present study. The healing rate was reported to be 81 % as seen on the ultrasound investigation. Unfortunately, comparison across the studies is hard since none of the other outcome parameters were alike those used on the current patient population. As summarized in the review by Spennachio, only 16 of 483 patients (3.3 %) had undergone new surgery to the same shoulder. This is less than the 12 out of 148 (8 %) who had performed new surgery in the present patient population. Aside from difference in follow-up time, variations in the policy of re-operations, socioeconomic factors (i.e. cost of health care and accessibility of non-operative treatment) and surgeons experience with re-operations might influence such differences. The heterogeneity of patient groups and differences in methods of evaluation make direct comparison across studies difficult—there is certainly a need for more patient evaluations reporting on the “true outcome” after rotator cuff repair.
A recent systematic review by Fermont et al. [12] pointed out four categories of prognostic factors that are viable in predicting patient outcomes after rotator cuff surgery. Along with demographic factors (older age, female gender) and concomitant diseases (diabetes mellitus, obesity and reduced level of activity)—morphological factors (bigger rotator cuff tears, high level of fatty infiltration) and concomitant surgical intervention of the biceps tendon or the acromioclavicular joint would be related to an inferior outcome. The current finding of inferior outcome in patients with long-standing symptoms and non-acute onset of their symptoms has, to our knowledge, rarely been reported. It is, however, well established that the ruptured supra- or infraspinatus tendon does degenerate with time and that fatty tissue will replace viable muscle [14, 23]. Although it has been found that proper surgical repair can partially reverse muscular atrophy and fatty infiltration, it is likely that there will be some irreversibility with advanced degeneration [40]. The current finding of inferior results with chronicity of symptoms is therefore not surprising.
Another highly notable result from the current population is the significant (in all outcome variables) lower post-operative score in patients who have used NSAIDs prior to the surgery. One could think that the severity of the disease—expressed by pain and symptoms prior to surgery—and thereof use of NSAIDs could be a possible confounding factor. When examining for such a relation, we were not able to find any difference in preoperative DASH score, VAS of pain and VAS of function. Neither was there any difference in duration of symptom in patients that received preoperative NSAIDs compared to the group that did not. Thus, the use of anti-inflammatory drugs probably did not delay any surgical treatment.
According to a review by Chen et al. [8], there are currently no patient-level studies investigating the effect of NSAIDs on soft tissue to bone healing. Former research has been performed in experimental rat models with a focus on the effect on tendon-to bone healing in the post-operative period [9, 11, 13]. The only study investigating rotator cuff healing was performed by Cohen et al. [9] on 180 rats that were examined at 2, 4 and 8 weeks after rotator cuff repair. There was significantly less organized collagen and lower load-to-failure at 4 and 8 weeks after the repair. The interpretation of such experimental results, as, stated by Chen, is that NSAIDs should be used prudently until more human clinical trial are performed [8].
In the present study, QuickDASH and VAS of function, VAS of pain and VAS of satisfaction has been used as outcome measures. The visual analogue scale is conventionally used in post-operative evaluations, also including rotator cuff repair [2, 15, 19, 36]. It has been validated for measuring chronic and experimental pain and has its ease in the quick and straight forward administration [33]. QuickDASH is an 11-item shortened and validated version of the more comprehensive DASH [3]. As compared to DASH, the condensed version has been found to have good reliability in evaluating shoulder-related diseases [25]. There are, however, only a handful of studies involving shoulder surgery, and only one involving rotator cuff repair that have utilized the score [35]. In 170 patients undergoing repair with or without acromioplasty Razmjou et al. found a preoperative mean QuickDASH of 44.6 and 6 months post-operative mean score of 19. The findings are not unlike those of the current study (50.9 preoperative and 14.4 at median 7-year follow-up). Although the follow-up time is non-comparable, it is interesting to see that a major improvement in the subjective score is observed within the initial 6 months after surgery—and perhaps less so after that time. A cohort of patients evaluated at constant intervals after surgery would have given a more profound insight into the convalescence after rotator cuff repair.
There are several limitations to the current study. First, if a control group receiving non-operative treatment had been included that would have revealed any potential difference in outcome between the operative and non-operative treatment modalities. Secondly, a more comprehensive evaluation of outcome would include radiological and clinical evaluation—including evaluation of range of motion and muscular function. When such evaluation has not been performed, there is a risk that some patients are “adapters” in the sense that they accept their reduced level of function and therefore report a more satisfying result than would objectively be found. A third limitation is the lack of reporting on patients who did not receive surgical treatment for their rotator cuff tear. The current study presents results from the largest follow-up evaluation of rotator cuff suture yet published. Other strengths include a uniform surgical technique and a good follow-up rate of over 80 % of the included patients, which is rare in clinical studies with extended follow-up evaluations.
Conclusion
An overall improvement was seen in the outcomes at 6–9 years after single-row arthroscopic rotator cuff repair of full-thickness rotator cuff tears—indicating a good clinical effectiveness over time. Gradual onset, long history of symptoms and the use of NSAIDs predicted worse outcome in the rotator cuff repair group, whereas age, gender and smoking status do not seem to be of importance for the outcome. The current study adds to the debate of NSAIDs usage in some certain shoulder-related diseases.
References
Andrews JR (2005) Diagnosis and treatment of chronic painful shoulder: review of nonsurgical interventions. Arthroscopy 21:333–347
Bartl C, Kouloumentas P, Holzapfel K, Eichhorn S, Wörtler K, Imhoff A, Salzmann GM (2012) Long-term outcome and structural integrity following open repair of massive rotator cuff tears. Int J Shoulder Surg 6:1–8
Beaton DE, Wright JG, Katz JN, Upper Extremity Collaborative Group (2005) Development of the QuickDASH: comparison of three item-reduction approaches. J Bone Joint Surg Am 87:1038–1046
Boudreault J, Desmeules F, Roy J, Dionne C, Framont P, MacDermid J (2014) The efficacy of oral non-steroidal anti-inflammatory drugs for rotator cuff tendinopathy: a systematic review and meta-analysis. J Rehabil Med 46:294–306
Buchbinder R, Green S, Youd JM (2013) Corticosteroid injections for shoulder pain. Cochrane Database Syst Rev 10:ED000068
Carr AJ, Rees JL, Ramsay CR, Fitzpatrick R, Gray A, Moser J, Dawson J, Bruhn H, Cooper CD, Beard DJ, Campbell MK (2014) Protocol for the United Kingdom Rotator CuffStudy (UKUFF): a randomised controlled trial of open and arthroscopic rotatorcuff repair. Bone Joint Res 3:155–160
Chaudhury S, Gwilym SE, Moser J, Carr AJ (2010) Surgical options for patients with shoulder pain. Nat Rev Rheumatol 6:217–226
Chen MR, Dragoo JL (2012) The effect of nonsteroidal anti-inflammatory drugs on tissue healing. Knee Surg Sports Traumatol Arthrosc 21:540–549
Cohen DB (2005) Indomethacin and celecoxib impair rotator cuff tendon-to-bone healing. Am J Sports Med 34:362–369
Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL (2012) National Trends in Rotator Cuff Repair. J Bone Joint Surg 94:227–233
Dimmen S, Nordsletten L, Engebretsen L, Steen H, Madsen JE (2009) The effect of parecoxib and indometacin on tendon-to-bone healing in a bone tunnel: an experimental study in rats. J Bone Joint Surg Br 91:259–263
Fermont AJM, Wolterbeek N, Wessel RN, Baeyens J-P, de Bie RA (2014) Prognostic factors for successful recovery after arthroscopic rotator cuff repair: a systematic literature review. J Orthop Sports Phys Ther 44:153–163
Ferry ST, Dahners LE, Afshari HM, Weinhold PS (2007) The Effects of common anti-inflammatory drugs on the healing rat patellar tendon. Am J Sports Med 35:1326–1333
Gumucio JP, Davis ME, Bradley JR, Stafford PL, Schiffman CJ, Lynch EB, Claflin DR, Bedi A, Mendias CL (2012) Rotator cuff tear reduces muscle fiber specific force production and induces macrophage accumulation and autophagy. J Orthop Res 30:1963–1970
Ji X, Bi C, Wang F, Wang Q (2014) Arthroscopic versus mini-open rotator cuff repair: an up-to-date meta-analysis of randomized controlled trials. Arthroscopy 31:118–124
Judge A, Murphy RJ, Maxwell R, Arden NK, Carr AJ (2014) Temporal trends and geographical variation in the use of subacromial decompression and rotator cuff repair of the shoulder in England. J Bone Joint Surg 96:70–74
Kartus J, Kartus C, Rostgård-Christensen L, Sernert N, Read J, Perko M (2006) Long-term clinical and ultrasound evaluation after arthroscopic acromioplasty in patients with partial rotator cuff tears. Arthroscopy 22:44–49
Kim HM, Caldwell J-ME, Buza JA, Fink LA, Ahmad CS, Bigliani LU, Levine WN (2014) Factors affecting satisfaction and shoulder function in patients with a recurrent rotator cuff tear. J Bone Joint Surg 96:106–112
Kim S-J, Jung M, Lee J-H, Kim C, Chun Y-M (2014) Arthroscopic repair of anterosuperior rotator cuff tears: in-continuity technique vs. Disruption of subscapularis-supraspinatus tear margin: comparison of clinical outcomes and structural integrity between the two techniques. J Bone Joint Surg 96:2056–2061
Kukkonen J, Kauko T, Virolainen P, Äärimaa V (2012) Smoking and operative treatment of rotator cuff tear. Scand J Med Sci Sports 24:400–403
Lambers Heerspink FO, Dorrestijn O, van Raay JJAM, Diercks RL (2014) Specific patient-related prognostic factors for rotator cuff repair: a systematic review. J Shoulder Elbow Surg 23:1073–1080
Longo UG, Franceschi F, Berton A, Maffulli N, Droena V (2012) Conservative treatment and rotator cuff tear progression. Med Sport Sci 57:90–99
Lundgreen K, Lian Ø, Scott A, Engebretsen L (2012) Increased levels of apoptosis and p53 in partial-thickness supraspinatus tendon tears. Knee Surg Sports Traumatol Arthrosc 21:1636–1641
Lundgreen K, Lian ØB, Scott A, Nassab P, Fearon A, Engebretsen L (2014) Rotator cuff tear degeneration and cell apoptosis in smokers versus nonsmokers. Arthroscopy 30:936–941
MacDermid JC, Khadilkar L, Birmingham TB, Athwal GS (2014) Validity of the QuickDASH in patients with shoulder related disorders undergoing surgery. J Orthop Sports Phys Ther 45:25–36
Mall NA, Tanaka MJ, Choi LS, Paletta GA (2014) Factors Affecting Rotator Cuff Healing. J Bone Joint Surg 96:778–788
Gulotta LV, Nho SJ, Dodson CC, Adler RS, Altchek DW, MacGillivray JD (2011) Prospective evaluation of arthroscopic rotator cuff repairs at 5 years: part I—Functional outcomes and radiographic healing rates. J Shoulder Elbow Surg 20:934–940
Mitchell C, Adebajo A, Hay E, Carr A (2005) Shoulder pain: diagnosis and management in primary care. BMJ 331:1124–1128
Moosmayer S, Lund G, Seljom US, Haldorsen B, Svege IC, Hennig T, Pripp AH, Smith HJ (2014) Tendon repair compared with physiotherapy in the treatment of rotator cuff tears: a randomized controlled study in 103 cases with a five-year follow-up. J Bone Joint Surg 96:1504–1514
Ostor AJK (2005) Diagnosis and relation to general health of shoulder disorders presenting to primary care. Rheumatology 44:800–805
Pegreffi F, Paladini P, Campi F, Porcellini G (2011) Conservative management of rotator cuff tear. Sports Med Arthrosc 19:348–353
Phillips NJ, Ali A, Stanley D (2003) Treatment of primary degenerative arthritis of the elbow by ulnohumeral arthroplasty. J Bone Joint Surg 85:347–350
Price DD, McGrath PA, Rafii A, Buckingham B (1983) The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 17:45–56
Randelli P, Bak K, Milano G (2015) State of the art in rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 23:341–343
Razmjou H, Davis AM, Jaglal SB, Holtby R, Richards RR (2011) Disability and satisfaction after rotator cuff decompression or repair: a sex and gender analysis. BMC Musculoskelet Disord 12:1–14
Rhee YG, Cho NS, Yoo JH (2014) Clinical outcome and repair integrity after rotator cuff repair in patients older than 70 years versus patients younger than 70 years. Arthroscopy 30:546–554
Russell RD, Knight JR, Mulligan E, Khazzam MS (2014) Structural integrity after rotator cuff repair does not correlate with patient function and pain. J Bone Joint Surg 96:265–271
Spennacchio P, Banfi G, Cucchi D, D’Ambrosi R, Cabitza P, Randelli P (2015) Long-term outcome after arthroscopic rotator cuff treatment. Knee Surg Sports Traumatol Arthrosc 23:523–529
Tilley JMR, Murphy RJ, Chaudhury S, Czernuszka JT, Carr AJ (2014) Effect of tear size, corticosteroids and subacromial decompression surgery on the hierarchical structural properties of torn supraspinatus tendons. Bone Joint Res 3:252–261
Yamaguchi H, Suenaga N, Oizumi N, Hosokawa Y, Kanaya F (2012) Will preoperative atrophy and fatty degeneration of the shoulder muscles improve after rotator cuff repair in patients with massive rotator cuff tears? Adv Orthop 2012:1–7
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest reported from any of the authors.
Rights and permissions
About this article
Cite this article
Inderhaug, E., Kollevold, K.H., Kalsvik, M. et al. Preoperative NSAIDs, non-acute onset and long-standing symptoms predict inferior outcome at long-term follow-up after rotator cuff repair. Knee Surg Sports Traumatol Arthrosc 25, 2067–2072 (2017). https://doi.org/10.1007/s00167-015-3845-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-015-3845-8