Abstract
Purpose
Whether minimally invasive total knee arthroplasty (MIS-TKA) could offer better and faster recovery without the deviation of post-operative prosthesis position and limb alignment is still controversial. This prospective and randomized study was conducted to compare the clinical and radiological outcomes between patients who underwent the mini-subvastus approach of MIS-TKA and those who underwent the medial parapatellar approach of traditional TKA.
Methods
Fifty patients, including 50 knees, who required TKA due to osteoarthritis were randomized to the mini-subvastus group (group I) or the medial parapatellar group (group II). All patients accepted the same method of anaesthesia, equal support therapy and identical rehabilitation exercise after surgery. The evaluation system included operation time, tourniquet time, blood loss, skin incision length in flexion, straight leg raising time, the time of lower limb muscle strength up to grade 4, the time of walking with aid or without aid, the time of walking up and down the stairs, the active flexion angle, range of movement (ROM), the Knee Society Scores (KSS), visual analogue score for pain (VAS), hospital stays and radiographic outcomes.
Results
The mini-subvastus approach offered smaller skin incision length in flexion, but at the cost of operation time (P < 0.001). No significant difference was found in tourniquet time and blood loss. The patients in group I could achieve straight leg raising, the lower limb muscle strength up to grade 4, walking with or without aid, and walking up and down the stairs earlier (P < 0.001). The active flexion angle, ROM, VAS and KSS in group I were superior to those in group II until six months post-operatively (P < 0.001), but the differences was not apparent at 12 months post-operatively. More importantly, there was no significant difference between the two groups on radiological outcomes (P > 0.05).
Conclusions
The mini-subvastus approach could offer faster recovery, less pain and shorter hospital stays without compromising the principles of proper prosthesis position and limb alignment compared with the medial parapatellar approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There is no doubt that total knee arthroplasty (TKA) has played an irreplaceable role in the surgical treatment of osteoarthritis, as reported in the relevant literature [1]. The medial parapatellar approach of traditional TKA is a mature surgical technique, which offers adequate surgical field exposure and relatively accurate positioning of the prosthesis. However it inevitably causes damage to the extensor mechanism because of patellar eversion and quadriceps dissection, in contrast to minimally-invasive total knee arthroplasty (MIS-TKA). Meanwhile, the increasing number of studies on TKA have shed light on the minimally-invasive technique which was developed with the aim of using a smaller incision and reducing injury to soft tissue, hopefully leading to less damage to the extensor mechanism, less post-operative pain and faster rehabilitation [2, 3]. The mini-subvastus approach, as a development of the subvastus technique pioneered by Hoffmann et al. [4], has been claimed to offer faster and better recovery, less pain, and greater range of motion (ROM) after surgery because of the limited incision length and the small extent of injury to the extensor mechanism [5]. However, it has been reported that MIS-TKA offered an inadequate operative field which could cause deviation of the mechanical axis and impact the long-term survival of the prosthesis [6, 7]. More importantly, studies of whether the mini-subvastus approach could avert deviation of the post-operative mechanical axis and limb mis-alignment while performing better and promoting faster recovery compared with the medial parapatellar approach are rare to date, especially prospective and randomized studies. Therefore, we conducted a prospective, randomized study to compare the early clinical and radiological outcomes between patients treated by the mini-subvastus approach and the medial parapatellar approach, with a minimum follow-up of one year.
Materials and methods
From January to May 2016, we conducted this prospective, randomized study which was approved by the institutional review boards of our hospital and Lu’an Affiliated Hospital of Anhui Medical University. All 50 patients were diagnosed with primary unilateral knee osteoarthritis, 31 in the left knee and 19 in the right knee. Patients provided signed informed consent and were randomly assigned to one of two groups according to computer-generated random numbers. The patients in group I (25 patients comprising 16 females and 9 males, 16 left knees and 9 right knees) underwent surgery by the mini-subvastus approach, and the patients in group II (25 patients including 16 females and 9 males, 15 left knees and 10 right knees) were treated by the medial parapatellar approach. The exclusion criteria were: (1) the symptoms of knee osteoarthritis could be improved by non-surgical treatment, (2) active infection, (3) previous fractures around the knee or knee surgery, (4) body mass index (BMI) over 35 kg m−2, and (5) knee flexion less than 90° and varus or valgus deformity of more than 15°. The preoperative data of age, gender, BMI, visual analogue score for pain (VAS), active flexion angle of knee, ROM, the Knee Society Scores (KSS), and the number of left and right knees are presented in Table 1. To increase the reliability of this study, the gender distribution was the same between the two groups, and there was no remarkable difference in the pre-operative demographics of the patients between group I and group II.
All patients accepted the same method of anaesthesia and the same type of knee prosthesis (posterior cruciate-retaining total knee prostheses, CR) and all operations were performed by two skilled joint surgeons. In the mini-subvastus approach group, the skin incision started from the medial aspect of the tibial tubercle and extended to the medial aspect of the superior pole, extending 8.5–10.5 cm along the medial side of the patella and vastus. The operative outcomes were not ignored simply in pursuit of a mini incision. The operative field was exposed through the application of an outward tensile force to the extensor mechanism and patella rather than by partly cutting off the quadriceps tendon and everting the patella. It should be emphasized that the vastus medialis of the extensor mechanism was rigorously preserved without any dissection. Then, making use of the “moving window” technique and specialized intramedullary alignment for the femoral component together with extramedullary alignment for the tibial component, the limited operation field could be shifted from the inferior to the superior aspect and from the medial to the lateral aspect as much as possible, allowing successful osteotomy and fixation of the prosthetic components. In the group treated by the parapatellar approach, the skin incision approximately 12–15 cm long extended from the tibial tubercle up to 5–8 cm proximal to the superior pole of the patella. The total knee could then be exposed to the surgical field by partly dissecting the quadriceps extensor mechanism and performing patella eversion, through which the surgeon could easily complete the osteotomy and prosthesis fitting. A tourniquet was used for every patient from the beginning of the installation of the prosthesis to the end of the operation. A C-arm X-ray machine was used for each patient, which enabled the surgeon to ensure better positioning of the prosthesis as far as possible. The posterior cruciate ligament was not resected in any patient, and a drainage tube was used in every patient in the two groups. No patients received a blood transfusion in either of the groups. All patients accepted cefotiam for normal anti-infection prophylaxis and rivaroxaban to prevent blood clots, but also adopted the uniform methods of functional training including active and passive flexion–extension of the operative knee, active flexion–extension of hips and ankles and trying to walk with aid or without aid once straight leg raising could be completed after operation. The patient assessment and data collection were performed by another surgeon, and a rehabilitation physician was responsible for conducting post-operative rehabilitation exercises with the patients. Furthermore, the two doctors did not know what type of approach was used for each patient or the relationship between surgical approach and incision length.
The data of operation time, tourniquet time, skin incision length in flexion, hospital stays, and blood loss including intra-operative blood loss and post-operative drainage for all patients were recorded after operation. The straight leg raising time and the time of lower limb muscle strength up to grade 4 were chosen as the evaluation indices for rehabilitation of the extensor mechanism. When the patients were able to accomplish straight leg raising, they were guided to make attempts to walk with or without aid, then the straight leg raising time and the time of walking with and without aid were recorded. We also recorded the time of walking up and down the stairs as a rehabilitation indicator. The active flexion angle of the knee, ROM and VAS (pain score according to a 10 cm visual analog scale, with 0 cm indicating no pain and 10 cm indicating the most severe pain) were evaluated at four days, seven days, one month, six months and 12 months after surgery; in addition, VAS was evaluated at one day after surgery. It needs to be emphasized that VAS was assessed three times a day when the patients were at rest and the median was recorded. The KSS was assessed and recorded at one month, six months and 12 months after surgery. The radiographic outcomes after surgery involving the frontal femoral component angle (FFC) and the frontal tibial component angle (FTC) were used to assess the position of the prosthesis via posteroanterior and lateral radiographs of the knee. In addition, we assessed the hip–knee–ankle angle (HKA) reflecting the mechanical axis (MA) from a post-operative full-length standing radiograph of the lower extremity. The HKA measured on the lateral side of the midline was made up of the mechanical axis of the femur and the mechanical axis of the tibia. The FFC measured on the lateral side of the midline was made up of the femoral axis and a line parallel to the distal surface of the femoral component. The FTC measured on the lateral side of the midline was made up of the tibial axis and a line parallel to the surface of the tibial component. The ideal values of the HKA, FFC, and FTC were 180°, 96° and 90°, respectively, before surgery [7]. All the above indicators were compared between group I and group II.
Statistical analysis was performed on a Windows-7 computer with SPSS 19.0 (SPSS Inc., Chicago, IL, USA). The independent t-test (Student’s t-test) and analysis of variance (ANOVA) were used to evaluate preoperative data of all patients. The clinical and radiographic results were also compared with independent t-tests and ANOVA. A value of P < 0.05 was considered significant.
Results
All patients of both groups accepted a minimum follow-up of one year. There was no remarkable difference between the groups in terms of age, gender, BMI, VAS, active flexion angle, ROM, KSS (knee score and functional score) and the proportion of left or right knees before operation (P > 0.05; Table 1).
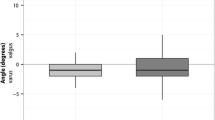
Between group I and group II, there were dramatic differences in mean operation time and skin incision length in flexion (P < 0.001; Table 2), but the mean blood loss and tourniquet time were comparable (P = 0.594 and P = 0.686, respectively; Table 2). The mean operation time in group II (66.6 minutes; range 57–76) was shorter than in group I (86.8 minutes; range 78–97) (Table 2), and the patients in group I had a smaller skin incision in flexion (mean 9.5 cm versus mean 13.6 cm; Table 2). The mean hospital stay after operation was 4.8 days (range 3–6) in group I, which was significantly shorter than the mean of 6.3 days (range 5–7) in group II (P < 0.001; Table 2). In addition, the mean straight leg-raising time was 1.1 days (range 1–2) in group I and 4.8 days (range 3–6) in group II (P < 0.001; Table 2). The mean time taken to restore lower limb muscle strength up to grade 4 was 1.2 days (range 1–3) in group I, which was significantly earlier than 5.6 days (range 4–7) in group II (P < 0.001; Table 2). The patients in group I achieved walking with an aid and without an aid at a mean of 1.7 days (range 1–3) and mean 3.7 days (range 3–5), respectively, compared with 6.0 days (range 4–8) and 7.6 days (range 6–9), respectively, in group II (P < 0.001; Table 2). Walking up and down the stairs was completed earlier in group I at a mean of 8.1 days (range 7–10) compared with a mean of 13.7 days (range 12–16) in group II (P < 0.001; Table 2). The mean flexion angle and ROM were greater in group I than group II at four days, seven days, one month and six months after operation (P < 0.001), but the differences disappeared at 12 months after operation (P > 0.05) (Fig. 1 and Fig. 2). The patients in group I had a significantly lower VAS at one day, four days, seven days, one month and six months, especially at one, four and seven days after operation versus the patients in group II (P < 0.001), but the difference had disappeared at 12 months after operation (P > 0.05; Fig. 3). The mean KSS including knee score and functional score in group I were significantly higher than those in group II at one month and six months after operation (P < 0.01), but no significant difference was found at 12 months after operation (P > 0.05; Fig. 4 and Fig. 5).
With regard to the radiographic outcomes after operation, the mean HKA, FFC and FTC did not differ markedly between the two groups (P > 0.05; Table 2), and no patients had an implant position or limb alignment deviated by more than ±2° from the target angle in either group after operation. No significant intra-operative or post-operative complication was reported in any patient up to the final follow-up.
Discussion
The most important finding of the study is that the mini-subvastus approach could offer faster recovery and less pain, with no higher risk of deviation of the prosthesis position or limb alignment in the patients who underwent TKA by the mini-subvastus approach. With the maturation of the traditional TKA technique, orthopaedic surgeons have shifted their attention to the minimally-invasive TKA technique which could offer less pain and faster recovery after surgery. It has been reported that the mini-subvastus approach, as one type of minimally-invasive technique, could offer less pain, faster return of knee function and higher patient satisfaction compared with the traditional technology by avoiding patellar eversion, and avoiding damage to the extensor mechanism and soft tissue balance [4, 8]. Pan et al. [4], who conducted a prospective randomized study of 35 minimally-invasive TKAs, and Lai et al. [5], who performed a prospective randomized controlled study of 35 minimally-invasive TKAs with a minimum follow-up of two years, however, suggested that the mini-subvastus approach could not ensure the ideal prosthesis position, resulting in the risk of associated complications. In addition there have been very few prospective randomized studies on whether use of the mini-subvastus approach can achieve ideal prosthesis position and limb alignment while offering better and faster recovery versus the medial parapatellar approach [4, 5]. Therefore, we performed a prospective randomized study, and found no remarkable difference between the groups with regard to demographic data and clinical data before operation, thus increasing the reliability of the outcome measures.
As previous studies have reported [4, 5, 9], we also found that the mini-subvastus approach could lead to longer operation time and a shorter skin incision in flexion versus traditional TKA, such as the medial parapatellar approach in our study. However we did not find longer tourniquet time or less blood loss in our study, suggesting that there was no significant difference between the mini-subvastus approach and the medial parapatellar approach with regard to tourniquet time and blood loss. A tourniquet was used for every patient from the beginning of the installation of the prosthesis to the end of the operation in our study, and although the mini-subvastus approach requires longer prosthetic installation time it requires less incision suture time. Although a longer operation time was required to complete TKA by the mini-subvastus approach, it has been reported that there is no evidence that further shortening of the operation time will lead to better patient outcomes for primary TKAs lasting less than 120 minutes [10]. Meanwhile, the shorter skin incision produced a better esthetic outcome which could improve patient satisfaction.
In consideration of the fact that direct measurement of quadriceps strength by a dynamometer, although very accurate, could cause severe pain to the patients [11], we indirectly assessed the recovery of quadriceps strength by measuring straight leg raising time and the time of lower limb muscle strength up to grade 4, which has never been used to assess the recovery of the quadriceps after TKA in other studies. Our study suggested that patients treated by the mini-subvastus approach could achieve straight leg raising notably earlier than the patients treated by the medial parapatellar approach, which was in agreement with the outcomes reported by other authors [4, 8, 12]. The mean time taken for extremity muscle strength to reach grade 4 in group I was also remarkably shorter than in group II. All of these results suggested that the mini-subvastus approach offered earlier recovery of quadriceps strength because it avoided incising the quadriceps and everting the patella, and it has been suggested that TKA without patellar eversion could reduce the risk of complications, which was demonstrated in a systematic review and meta-analysis conducted by Yang et al. [13].
Our study also found that the patients who underwent TKA by the mini-subvastus approach could achieve earlier walking with or without aid and walking up and down stairs compared with the patients treated by the medial parapatellar approach. Moreover, getting out of bed as soon as possible might reduce the risk of complications caused by long-term immobilization and improve heart–lung capability. Most previous prospective randomized studies of MIS-TKA suggested that there were no significant differences between patients who accepted MIS-TKA and those who accepted traditional TKA with regard to the long-term outcomes of ROM [4, 5, 14, 15]. In our study, for a more comprehensive assessment of early clinical outcomes, we measured the active flexion angle and ROM at four days, seven days, one month, six months and 12 months after operation. We found that both the flexion and the ROM in group I were markedly superior to those in group II at four days, seven days, one month and six months after operation, especially at four and seven days after operation; however, the differences diminished with time. Furthermore, the mean knee score, functional score (KSS) and VAS in group I were significantly higher than in group II up to six months post-operatively. It should be emphasized that the earlier pain was assessed three times a day at one day, four days, seven days, one month, six months and 12 months after operation, instead of only at one day after operation as in the prospective randomized study conducted by Lai et al. [5]. Our results showed that the patients who underwent TKA by the mini-subvastus approach suffered less pain compared with the patients in group II at one day, four days, seven days, one month and six months, and especially at one, four and seven days. Therefore, we conclude that patients treated by mini-subvastus approach TKA recovered faster, experienced less pain and had shorter hospital stays.
Although minimally-invasive technology can bring many benefits, some authors have suggested that prosthesis position and limb alignment, which are important in TKA, could not be ensured through the mini-subvastus approach. Such poor prosthesis positioning and limb alignment might result in a negative effect on the long-term survival of the prosthesis and related complications, such as early poly wear loosening [3, 6, 7, 16]. Lai et al. [5] suggested that patients could receive temporary benefits from the mini-subvastus approach, but at the expense of the higher risk of component malposition. We assessed the position of the prosthesis via the HKA angle, the FFC angle and the FTC angle [5, 7, 9]. Our study, however, demonstrated that there was no significant difference in post-operative HKA, FFC or FTC between the groups, and none of the patients had the implant position or limb alignment deviated by more than ±2° from the target angle in both groups after operation. Although the operative field of the mini-subvastus approach was smaller than the operative field of the traditional approach, the surgeon could successfully complete osteotomy and prosthesis fitting through the “mobile windows” technique with the use of special surgical instruments. Schroer et al. [17] previously reported the complication rate of 600 patients who underwent minimally-invasive TKA performed via the mini-subvastus approach, and found that it did not lead to an increased complication rate in comparison with traditional TKA. In agreement with this, we found no significant complication in any patient in our study up to our final follow-up. Certainly, the surgical technique of the surgeon also plays an important role in the success of the operation.
A limitation of our study was the relatively small number of patients involved, which could negatively affect the power of this study, and a larger sample size will be necessary to confirm our results.
Conclusions
In conclusion, based on the findings of our study, we suggest that the patients who underwent TKA via the mini-subvastus approach experienced faster recovery, less pain, shorter skin incision length and shorter hospital stays. Although there was no greater risk of deviation of the prosthesis position and of limb alignment in the patients who underwent TKA by the mini-subvastus approach compared with the patients treated by the medial parapatellar approach, further investigation with more patients is necessary.
References
Heekin RD, Fokin AA (2014) Mini-midvastus versus mini-medial parapatellar approach for minimally invasive total knee arthroplasty. J Arthroplast 29(2):339–342
Kohrt W, Shulman B, Muratore T, Bade M, Dayton M, Stevens-Lapsley J (2012) Minimally invasive total knee arthroplasty: surgical implications for recovery. J Knee Surg 26(03):195–202
Lin SY, Chen CH, Fu YC, Huang PJ, Lu CC, Su JY, Chang JK, Huang HT (2013) Comparison of the clinical and radiological outcomes of three minimally invasive techniques for total knee replacement at two years. Bone Joint J 95-B(7):906
Pan WM, Li XT, Qian ZL, Zhang Q, Zhang CM (2010) Mini-subvastus versus a standard approach in total knee arthroplasty: a prospective, randomized, controlled study. J Int Med Res 38(3):890–900
Lai Z, Shi S, Fei J, Wei W (2014) RETRACTED ARTICLE: Total knee arthroplasty performed with either a mini-subvastus or a standard approach: a prospective randomized controlled study with a minimum follow-up of 2 years. Arch Orthop Trauma Surg 134(8):1155–1162
Lin W-P, Lin J, Horng L-C, Chang S-M, Jiang C-C (2009) Quadriceps-sparing, minimal-incision total knee arthroplasty. J Arthroplast 24(7):1024–1032
Thiengwittayaporn S, Fusakul Y, Kangkano N, Jarupongprapa C, Charoenphandhu N (2015) Hand-held navigation may improve accuracy in minimally invasive total knee arthroplasty: a prospective randomized controlled trial. Int Orthop 40(1):51–57
Schroer WC, Diesfeld PJ, Reedy ME, LeMarr AR (2008) Mini-subvastus approach for total knee arthroplasty. J Arthroplast 23(1):19–25
Thiengwittayaporn S, Kanjanapiboonwong A, Junsee D (2013) Midterm outcomes of electromagnetic computer-assisted navigation in minimally invasive total knee arthroplasty. J Orthop Surg Res 8(1):37
Young SW, Mutu-Grigg J, Frampton CM, Cullen J (2014) Does speed matter? Revision rates and functional outcomes in TKA in relation to duration of surgery. J Arthroplast 29(7):1473–1477.e1471
Cho K-Y, Kim K-I, Umrani S, Kim S-H (2013) Better quadriceps recovery after minimally invasive total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22(8):1759–1764
Tsuji S, Tomita T, Fujii M, Laskin RS, Yoshikawa H, Sugamoto K (2010) Is minimally invasive surgery–total knee arthroplasty truly less invasive than standard total knee arthroplasty? J Arthroplast 25(6):970–976
Yang G, Huang W, Xie W, Liu Z, Zheng M, Hu Y, Tian J (2015) Patellar non-eversion in primary TKA reduces the complication rate. Knee Surg Sports Traumatol Arthrosc 24(3):921–930
Chiang H, Lee C-C, Lin W-P, Jiang C-C (2012) Comparison of quadriceps-sparing minimally invasive and medial parapatellar total knee arthroplasty: a 2-year follow-up study. J Formos Med Assoc 111(12):698–704
Tasker A, Hassaballa M, Murray J, Lancaster S, Artz N, Harries W, Porteous A (2014) Minimally invasive total knee arthroplasty; a pragmatic randomised controlled trial reporting outcomes up to 2 year follow up. Knee 21(1):189–193
Kashyap SN, van Ommeren JW (2008) Clinical experience with less invasive surgery techniques in total knee arthroplasty: a comparative study. Knee Surg Sports Traumatol Arthrosc 16(6):544–548
Schroer WC, Diesfeld PJ, Reedy ME, Lemarr AR (2007) Evaluation of complications associated with six hundred mini-subvastus total knee arthroplasties. J Bone Joint Surg Am Vol 89(Suppl_3):76–81
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all the authors, the corresponding author states that there is no conflict of interest.
Rights and permissions
About this article
Cite this article
Li, Z., Cheng, W., Sun, L. et al. Mini-subvastus versus medial parapatellar approach for total knee arthroplasty: a prospective randomized controlled study. International Orthopaedics (SICOT) 42, 543–549 (2018). https://doi.org/10.1007/s00264-017-3703-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3703-z