Abstract
Background
Alpha-defensin, a novel biomarker, has shown great potential for the accurate diagnosis of periprosthetic joint infection (PJI) in recent years: many published studies have presented encouraging results. Nevertheless, the diagnostic accuracy of alpha-defensin is inconsistent across published studies. Moreover, the optimum value of the diagnostic threshold urgently needs to be ascertained. This meta-analysis sought to estimate the precision of alpha-defensin for the diagnosis of PJI and, where possible, to confirm the threshold.
Method
We systematically searched PubMed, Embase, Cochrane, Web of Knowledge, and ClinicalTrials.gov for relevant literature on alpha-defensin in the diagnosis of PJI (searching publications from the inception of each database until February 2017, with no language restriction). Pooled sensitivity, specificity, diagnostic odds ratios, and likelihood ratios were the indexes used for assessment, with the use of a random-effects model.
Result
Eleven of the 426 studies that evaluated the diagnostic accuracy of alpha-defensin in periprosthetic joint infection (PJI) were included in this analysis. The pooled diagnostic sensitivity of alpha-defensin for PJI was 0.96 (95% confidence interval [CI], 0.87 to 0.99) and the specificity was 0.95 (95% CI, 0.91 to 0.97). Since there was substantial heterogeneity among studies, based on the inconsistency index (I2), threshold, site of arthroplasty, study design and techniques for the alpha-defensin test, subgroup analyses were performed to estimate the impacts of these variables on heterogeneity.
Conclusion
In summary, this meta-analysis clearly lends support to the conclusion that alpha-defensin is a promising addition to the current methods for diagnosis of PJI.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Periprosthetic joint infection (PJI) can result in extremely poor arthroplasty outcomes. Such infections account for approximately 14.8% of the factors leading to the failure of hip replacement, and are the major cause of revision following total knee arthroplasty, with an incidence of 25.2% [1, 2]. It is crucial to identify PJI accurately and quickly. However, the distinctions between joint infection and aseptic loosening are clinically difficult to discern due to the low virulence of the infecting micro-organisms and the formation of biofilms which can prevent bacteria from being killed by antimicrobials [3]. In addition, clinical symptoms and signs are sometimes equivocal, while the conventional culture of pathogens has low sensitivity, and inflammatory markers from serum or synovial fluid have limitations [4, 5]. Although some new techniques, such as the culture of prosthetic sonicate fluid from synovial fluid, polymerase chain reaction assays, and nuclear medicine imaging techniques, have been applied to detect infection, there is still a lack of methods with extremely high accuracy [6,7,8].
Fortunately, researchers have found substances present in serum and synovial fluid that increase or decrease in concentration in patients with an infectious condition; these are known as biomarkers. Any fluctuation in the quantity of these substances can predict the infectious state. Alpha-defensin, one of these biomarkers, is an antimicrobial peptide that is naturally released from activated neutrophils. It is active against bacteria, fungi, and viruses. When infection is present, the peptide is released, integrates into the pathogen’s membranes, and destroys the pathogen [9].
Recently, several articles reported the diagnostic value of alpha-defensin for PJI, but the results were inconsistent across these studies. In addition, there were also two meta-analysis articles that examined the diagnostic accuracy of alpha-defensin, and the findings showed great promise [10, 11]. However, very few studies were included in these two meta-analyses, which could lead to low reliability. As a few new studies have been reported recently, a meta-analysis that includes these emerging studies is needed to verify the accuracy of the previous findings. The current systematic review and meta-analysis aims to assess the diagnostic accuracy of alpha-defensin as a biomarker of PJI.
Materials and methods
This systematic review and meta-analysis is reported in adherence with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement and has been registered at International Prospective Register of Systematic Reviews (number CRD42017057499) [12].
Search strategy
We systematically searched PubMed, Embase, Cochrane, Web of Knowledge, and Clinical Trials for studies related to alpha-defensin’s utility in the diagnosis of PJI, from the inception of each database until February 2017 with no language restrictions, and the search strategy was constructed according to different databases. MeSH terms and free text words used are shown as below:
-
#1
Arthroplasty, Replacement [mh] OR (Joint Prosthesis Implantation) OR (Implantation, Joint Prosthesis) OR (Implantations, Joint Prosthesis) OR (Joint Prosthesis Implantations) OR (Prosthesis Implantation, Joint) OR (Prosthesis Implantations, Joint) OR (Replacement Arthroplasty) OR (Arthroplasties, Replacement) OR (Replacement Arthroplasties)
-
#2
Alpha-Defensins [mh] OR (alpha Defensins) OR (Antimicrobial Peptides, Neutrophil) OR (Neutrophil Antimicrobial Peptides) OR (Peptides, Neutrophil Antimicrobial)
-
#3
Bacterial Infections and Mycoses [mh] OR Prosthesis-Related Infections [mh] OR (Prosthesis Related Infections) OR (Infections, Prosthesis-Related) OR (Prosthesis-Related Infection)
Eligibility criteria
For the objective of this review, we regarded studies as eligible if they assessed the accuracy of alpha-defensin in comparison with the diagnostic results of a definite reference standard. Studies that did not provide sufficient data with which to calculate the values for true-positive, false-positive, true-negative, and false-negative results or that included the same patients were excluded. Data extraction and quality assessment.
Data extraction was completed by two researchers (Yuan and Yan), and the following information was collected: (1) study characteristics (author, year of publication, country, design, sample site, test technique and number analyzed for each study); (2) population characteristics (mean age of patients and sex); (3) cut-off or range definitions of the tests; (4) reference standard. Data that could be used to calculate the outcomes of interest were extracted. Disagreements were resolved by consensus.
The methodological quality of each included study was evaluated by using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS)-2 tool, which consists of four key domains: patient selection, index test, reference standard, and flow and timing. The risk of bias assessment of the four domains and the clinical applicability of the first three domains were assessed with signaling questions. Questions were answered “yes” for low risk of bias/concerns, “no” for high risk of bias/concerns, or “unclear” [13]. Publication bias was explored based on the regression test of asymmetry, and significant publication bias was defined as a p value <0.1.
Statistical analysis
In the two published meta-analyses [10, 11], there may have been heterogeneity among the selected studies. Therefore, we chose to use a random effects model to process the whole pooled analyses. The inconsistency index (I2) statistic was applied to estimate the heterogeneity. I2 estimates the percentage variability in results across studies that is explained by true differences in patients, tests, outcomes, and design rather than by chance; values of 25%, 50%, and 75% indicate low, moderate, and high inconsistency, respectively [14].
The diagnostic odds ratio and the likelihood of ratio were chosen as the primary outcomes of interest, along with pooled sensitivity and specificity. The likelihood ratio was defined as the probability of a given test result in patients with disease divided by the probability of that same result in patients without the disease. The positive likelihood ratio equals sensitivity/(1-specificity); the negative likelihood ratio equals (1-sensitivity)/specificity.
The diagnostic odds ratio, which equals the ratio of the positive likelihood ratio to the negative likelihood ratio, shows how much greater the odds of having the disease (PJI) are for a patient with a positive test result (alpha-defensin present) than for a patient with a negative test result. This endpoint is considered to be convincing and highly reliable, since it does not depend on the prevalence of the disease that the test is used to diagnose, and is often reasonably constant regardless of the diagnostic threshold [15].
What’s more, we visually inspected the summary receiver-operating characteristic (SROC) curves, a “shoulder and arm pattern” might suggest the existence of diagnostic threshold bias. In addition, the correlation between logit sensitivity and specificity caused by using different thresholds among studies was calculated with a mixed model; a p value of <0.05 was set to indicate a significant threshold effect [16].
As the diagnostic threshold and test technique were factors that might influence the accuracy of alpha-defensin as a biomarker, we performed subgroup analyses according to the index test threshold (5.2 mg/L or other value) and test technique (alpha-defensin immunoassay or other methods). In addition, we planned to carry out subgroup analysis with study design (retrospective compared with prospective) and prosthesis location (whether shoulder arthroplasty was included) as independent variables.
To assess the clinical utility of alpha-defensin as a biomarker, we used a Fagan nomogram. The Fagan nomogram is a graphical tool that can be used to estimate how much the result of the alpha defensin assay changes the probability that a patient has a PJI [17].
We used Stata software (version 14, StataCrop) for all statistical analyses, and the commands applied were midas and metandi.
Results
Search results
Four hundred and twenty-six articles were retrieved through the primary search, 23 of which were considered eligible after the two independent reviewers reviewed the titles and abstracts. After reading the full text of each report in detail, 11 studies were eventually included in our analysis. The consensus between our two reviewers on the final selection of studies was 93.8%, with a kappa statistic of 0.85 (standard error, 0.15; 95% confidence interval [CI], 0.56 to 1.00). The PRISMA flow diagram is provided in Fig. S1.
These 11 studies included 2712 patients treated with a revision surgery, among whom 472 (17.4%) were confirmed to have a joint infection. The average ages of patients ranged from 41 to 89 years old and males accounted for 42.3% to 48% of the study populatioin. In addition to hip and knee arthroplasty, three studies also included patients with shoulder or other joint replacement. The test technology used by most of the researchers used was alpha-defensin immunoassay (CD Diagnostics). For the reference standard, criteria [18] proposed by the Muscularskeletal Infection Society (MSIS) were chosen in 10 studies. One analysis [19], which included only patients who had undergone shoulder arthroplasty, synthesized the clinical, laboratory, and histologic criteria, including serum ESR and CRP, frozen section histology, and culture results of the pre-operative synovial fluid aspirate, intra-operative tissue and synovial fluid specimens as a gold standard. Detailed information on individual studies is summarized in Table 1.
Quality assessment and publication bias
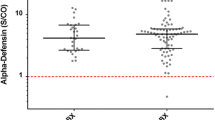
Two of our researchers evaluated the methodological quality of all studies, using the QUADAS-2 tool. The QUADAS-2 assessments (Fig. S2) indicated that the studies included in this meta-analysis were of good quality. By assessing funnel plot asymmetry based on the Deeks tests, we found no evidence of significant publication bias for alpha-defensin (p = 0.16>0.1). The results are presented in Fig. 1.
Diagnostic value of alpha-defensin for PJI
We performed a pooled analysis of the 11 studies, the diagnostic sensitivity and specificity, diagnostic odds ratio, and positive/negative likelihood ratios for alpha-defensin were calculated.
As shown in Fig. 2, the pooled diagnostic sensitivity and specificity of alpha-defensin for PJI were 0.96 (95% CI, 0.87 to 0.99) and 0.95 (95% CI, 0.91 to 0.97), respectively. We detected high between-study heterogeneity, as the corresponding I2 statistics for sensitivity and specificity value were 88.98 (95% CI, 83.75 to 94.21) and 96.50 (95% CI, 95.32 to 97.67). The pooled diagnostic odds ratio (Fig. 3) was 422.72 (95% CI, 83.22 to 2147.30). The pooled positive likelihood ratio and negative likelihood ratio were 19.19 (95% confidence interval [CI], 9.72 to 37.91) and 0.05 (95% confidence interval [CI], 0.01 to 0.15), respectively. The area under the SROC (AUSROC) was 0.99 (95% confidence interval [CI], 0.97 to 0.99) (Fig. 4).
Threshold value of alpha-defensin
Five of the studies we included chose the same value, 5.2 mg/l (1.0S/CO), as the threshold. The other six analyzed different preset cut-offs, or no cut-off. The diagnostic odds ratio of the five studies that used the same threshold was 701.97 (95% CI, 125.82 to 3916.49); the corresponding positive likelihood ratio and negative likelihood ratio were 23.18 (95% CI, 8.91 to 60.29) and 0.03 (95% CI, 0.01 to 0.10), respectively (Table 2).
Subgroup analyses
As the I2 statistics (>75%) illustrated significant between-study heterogeneity in this study, it was necessary to perform a subgroup analysis to find the potential source. According to the characteristics table, eight of the studies used the same alpha-defensin immunoassay (CD Diagnostics), which was used in the laboratory, while three studies that adopted a lateral flow test (Zimmer Inc.), which was conducted intraoperatively. We analyzed the diagnostic accuracy outcomes of these two groups. When applying the alpha-defensin immunoassay, the pooled diagnostic odds ratio was 996.98 (95% CI, 139.80 to 7109.74); the positive likelihood ratio and negative likelihood ratio were 27.73 (95% CI, 11.33 to 67.84) and 0.03 (95% confidence interval [CI], 0.01 to 0.11), respectively. The corresponding indexes when using a lateral flow test were 30.82 (95% confidence interval [CI], 8.09 to 117.44), 6.84 (95% confidence interval [CI], 2.65 to 17.67), and 0.22 (95% confidence interval [CI], 0.09 to 0.52) (Table 2).
Extra subgroup analyses of diagnostic accuracy were conducted with site of arthroplasty (only hip and knee, including shoulder or elbow) and study design (prospective or retrospective) as independent variables (see Table 2). The primary data are insufficient for us to perform a similar analysis on the effects of prosthesis age.
Evaluation of clinical utility
Using the likelihood ratio, we constructed a Fagan nomogram to calculate the post-test probability of periprosthetic joint infection (Fig. 5). The nomogram was based on a likelihood ratio of 19.0 for a positive alpha-defensin result and a likelihood ratio of 0.05 for a negative one. When a pre-test probability of 0.2 (i.e., a 20% prevalence of infection in patients undergoing revision arthroplasty) was assumed, a positive alpha-defensin result from synovial fluid (red line) predicted an 83% probability of a PJI diagnosis, and a negative alpha-defensin result (purple line) predicted a 1% probability of a PJI diagnosis.
Discussion
As we mentioned earlier, the diagnosis of PJI has been puzzling surgeons since arthroplasty was first applied in orthopedics. Researchers have attempted to diagnose this disease by using various methods, including (1) a local inflammatory index, such as synovial fluid leukocyte count [30] and periprosthetic tissue histology [31]; (2) systematic measures of inflammation, such as serum C-reactive protein level [32], erythrocyte sedimentation rate, and IL-6 level [33]; and (3) radiographic tests, radiographs, nuclear medicine imaging, magnetic resonance imaging(MRI), computed tomography (CT), and positron emission tomography [5]. However, similar to clinical symptoms and signs, laboratory findings and imaging studies are non-specific. Given the lack of an optimum threshold value and widely approval criteria, PJI is still a major challenge to diagnose [4]. Given this issue, the Musculoskeletal Infection Society (MSIS) published a new definition of PJI (Table S1) in 2011, which combined clinical data and laboratory tests and sought to give doctors a rough indication of diagnosis [18]. In addition, some scientists have attempted to use serum and synovial fluid biomarkers to diagnose the joint infection, and the results of many studies have shown that biomarkers in synovial fluid are more reliable than those in serum [21, 34, 35]. Alpha-defensin from synovial fluid, a synovial biomarker that could be used as a new pre-operative and intra-operative tests for diagnosis, has become increasingly reported.
The pooled estimation of the 11 studies included here indicated the strong sensitivity and specificity of alpha-defensin to identify PJI, as the pooled sensitivity and specificity were 0.96 (95% confidence interval [CI], 0.87 to 0.99) and 0.95 (95% CI, 0.91 to 0.97), respectively. Moreover, the Fagan nomogram revealed that alpha-defensin was very good at predicting and ruling out PJI. Positive likelihood ratios >10 and negative likelihood ratios <0.1 have been noted to provide convincing diagnostic evidence, whereas those of >5 and <0.2 provide strong diagnostic evidence. The positive likelihood ratio and negative likelihood ratio of alpha-defensin were 19.19 (95% confidence interval [CI], 9.72 to 37.91) and 0.05 (95% confidence interval [CI], 0.01 to 0.15), respectively. This finding demonstrated that a positive (or negative) result for alpha-defensin indicates a greatly increased (or decreased) likelihood of infection in patients undergoing revision surgery on a failed hip or knee arthroplasty, or even shoulder arthroplasty.
Given that the results were highly inconsistent across studies, we performed a subgroup analysis, focusing on the threshold and test techniques. When calculating the correlation between logit sensitivity and specificity caused by using different thresholds with a mixed model, the correlation coefficient was 0.73 with a p value of 0.53; we considered that there was no significant threshold effect contributing to the between-study heterogeneity. We could also draw this conclusion because no shoulder-like ROC plane curve was observed. As a new method used to detect PJI, there is no consensus about the most accurate threshold for alpha-defensin. Among the studies included in this analysis, five set 5.2 mg/L as the cut-off, and the other six set different cut-offs. Although the diagnostic odds ratio, positive likelihood ratio, and negative likelihood ratio of the five studies that used the same threshold were all higher than the pooled ones, we were unable to draw the conclusion that 5.2 mg/l (1.0S/CO) is the optimum threshold, since not enough studies set other different cut-offs for us to make a comparison. When analyzing groups that used different techniques (alpha-defensin immunoassay and lateral flow test), we found significant variation in the diagnostic index. We therefore conclude that the techniques used on the specimens can affect diagnostic accuracy. Specifically, the lateral flow test might be inferior to the alpha-defensin immunoassay. More evidence is needed to assess the value of these two methods.
Compared with the other diagnostic methods mentioned previously, using alpha-defensin as a biomarker has some advantages. One is that it maintains its high diagnostic accuracy for PJI even in the setting of antibiotic administration. Shahi et al. [36] performed a comparison between patients who were treated with antibiotics and those who were not treated before diagnostic workup. They found that the alpha-defensin test maintained its concentration and sensitivity for PJI under the antibiotic setting. Another advantage is that its precision is not influenced by the site of arthroplasty [19, 29]. Although eight studies involved only patients undergoing hip and knee replacement and three studies included some other joint arthroplasties, the pooled analysis index showed no significant difference. Moreover, the novel Synovasure periprosthetic joint infection (PJI) lateral flow test device that was used in three studies [27,28,29] is now commercially available. It features easy use and quick results (10 min), which means that it can be performed intraoperatively. This advantage might make testing for alpha-defensin relatively acceptable.
The strengths and potential limitations of this study should be acknowledged. This study is the first meta-analysis focused on the utility of alpha-defensin for the diagnosis of PJI. We included all relevant studies, and these used the same MSIS criteria as the reference standard except for one. The demographic characteristics of the patients in these studies, such as the age and sex ratio, were similar, which could reduce the heterogeneity to some degree. One limitation of this analysis is that several studies [21,22,23,24] were reported by a single team (that of Carl Deirmengiant), whose group instructed a single company to perform the relevant test, there might have been a certain amount of crossover among the patients included and a conflict of interest, as well. In addition, few studies conducted long-term follow-ups to detect low-grade infection in patients with negative culture results, and the presence of such low-grade infection may increase false negativity.
Conclusion
Our results revealed the strong potential value of alpha-defensin, but more research remains to be performed to determine the optimum threshold. Although we were able to define a threshold from the SROC, it is not reliable as the technical level of every laboratory differs greatly. Only when more studies with larger sample size have been conducted could we then recommend a threshold to maximize the sensitivity and specificity. Given that the validity of this biomarker for the diagnosis of PJI is a strong match with the results of the MSIS criteria, alpha-defensin from synovial fluid is highly reliable at predicting a diagnosis of PJI and is precise at ruling out this diagnosis. Thus, this new biomarker from synovial fluid should be considered an essential adjunct to the difficult diagnosis of PJI.
References
Parvizi J, Pawasarat IM, Azzam KA, Joshi A, Hansen EN, Bozic KJ (2010) Periprosthetic joint infection: the economic impact of methicillin-resistant infections. J Arthroplast 25:103–107. https://doi.org/10.1016/j.arth.2010.04.011
Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, Vail TP, Rubash HE, Berry DJ (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468:45–51. https://doi.org/10.1007/s11999-009-0945-0
Trampuz A, Osmon DR, Hanssen AD, Steckelberg JM, Patel R (2003) Molecular and antibiofilm approaches to prosthetic joint infection. Clin Orthop Relat Res 414:69–88. https://doi.org/10.1097/01.blo.0000087324.60612.93
Del Pozo JL, Patel R (2009) Clinical practice. Infection associated with prosthetic joints. N Engl J Med 361:787–794. https://doi.org/10.1056/NEJMcp0905029
Nodzo SR, Bauer T, Pottinger PS, Garrigues GE, Bedair H, Deirmengian CA, Segreti J, Blount KJ, Omar IM, Parvizi J (2015) Conventional diagnostic challenges in periprosthetic joint infection. J Am Acad Orthop Surg 23(Suppl):S18–S25. https://doi.org/10.5435/jaaos-d-14-00385
Trampuz A, Piper KE, Jacobson MJ, Hanssen AD, Unni KK, Osmon DR, Mandrekar JN, Cockerill FR, Steckelberg JM, Greenleaf JF, Patel R (2007) Sonication of removed hip and knee prostheses for diagnosis of infection. N Engl J Med 357:654–663. https://doi.org/10.1056/NEJMoa061588
Ryu SY, Greenwood-Quaintance KE, Hanssen AD, Mandrekar JN, Patel R (2014) Low sensitivity of periprosthetic tissue PCR for prosthetic knee infection diagnosis. Diagn Microbiol Infect Dis 79:448–453. https://doi.org/10.1016/j.diagmicrobio.2014.03.021
Morbach H, Schneider P, Schwarz T, Hofmann C, Raab P, Neubauer H, Duren C, Beer M, Girschick HJ (2012) Comparison of magnetic resonance imaging and 99mTechnetium-labelled methylene diphosphonate bone scintigraphy in the initial assessment of chronic non-bacterial osteomyelitis of childhood and adolescents. Clin Exp Rheumatol 30:578–582
Lehrer RI, Ganz T (1992) Defensins: endogenous antibiotic peptides from human leukocytes. CIBA Found Symp 171:276–290 discussion 290-273
Wyatt MC, Beswick AD, Kunutsor SK, Wilson MJ, Whitehouse MR, Blom AW (2016) The alpha-defensin immunoassay and leukocyte esterase colorimetric strip test for the diagnosis of periprosthetic infection: a systematic review and meta-analysis. J Bone Joint Surg Am 98:992–1000. https://doi.org/10.2106/jbjs.15.01142
Xie K, Qu X, Yan M (2016) Procalcitonin and alpha-defensin for diagnosis of periprosthetic joint infections. J Arthroplast. https://doi.org/10.1016/j.arth.2016.10.001
Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151(264–269):w264
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ (Clin Res Ed) 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Glas AS, Lijmer JG, Prins MH, Bonsel GJ, Bossuyt PM (2003) The diagnostic odds ratio: a single indicator of test performance. J Clin Epidemiol 56:1129–1135
Altman DG, Bland JM (2003) Interaction revisited: the difference between two estimates. BMJ (Clin Res Ed) 326:219
Fagan TJ (1975) Letter: Nomogram for Bayes theorem. N Engl J Med 293:257. https://doi.org/10.1056/nejm197507312930513
Parvizi J, Zmistowski B, Berbari EF, Bauer TW, Springer BD, Della Valle CJ, Garvin KL, Mont MA, Wongworawat MD, Zalavras CG (2011) New definition for periprosthetic joint infection: from the Workgroup of the Musculoskeletal Infection Society. Clin Orthop Relat Res 469:2992–2994. https://doi.org/10.1007/s11999-011-2102-9
Frangiamore SJ, Saleh A, Grosso MJ, Kovac MF, Higuera CA, Iannotti JP, Ricchetti ET (2015) alpha-defensin as a predictor of periprosthetic shoulder infection. J Shoulder Elb Surg 24:1021–1027. https://doi.org/10.1016/j.jse.2014.12.021
Bingham J, Clarke H, Spangehl M, Schwartz A, Beauchamp C, Goldberg B (2014) The alpha defensin-1 biomarker assay can be used to evaluate the potentially infected total joint arthroplasty. Clin Orthop Relat Res 472:4006–4009. https://doi.org/10.1007/s11999-014-3900-7
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J (2014) Diagnosing periprosthetic joint infection: has the era of the biomarker arrived? Clin Orthop Relat Res 472:3254–3262. https://doi.org/10.1007/s11999-014-3543-8
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Parvizi J (2014) Combined measurement of synovial fluid alpha-Defensin and C-reactive protein levels: highly accurate for diagnosing periprosthetic joint infection. J Bone Joint Surg Am 96:1439–1445. https://doi.org/10.2106/jbjs.m.01316
Deirmengian C, Kardos K, Kilmartin P, Cameron A, Schiller K, Booth RE Jr, Parvizi J (2015) The alpha-defensin test for periprosthetic joint infection outperforms the leukocyte esterase test strip. Clin Orthop Relat Res 473:198–203. https://doi.org/10.1007/s11999-014-3722-7
Deirmengian C, Kardos K, Kilmartin P, Gulati S, Citrano P, Booth RE Jr (2015) The alpha-defensin test for periprosthetic joint infection responds to a wide spectrum of organisms. Clin Orthop Relat Res 473:2229–2235. https://doi.org/10.1007/s11999-015-4152-x
Bonanzinga T, Zahar A, Dutsch M, Lausmann C, Kendoff D, Gehrke T (2016) How reliable is the alpha-defensin immunoassay test for diagnosing periprosthetic joint infection? A prospective study. Clin Orthop Relat Res. https://doi.org/10.1007/s11999-016-4906-0
Frangiamore SJ, Gajewski ND, Saleh A, Farias-Kovac M, Barsoum WK, Higuera CA (2016) Alpha-defensin accuracy to diagnose periprosthetic joint infection-best available test? J Arthroplast 31:456–460. https://doi.org/10.1016/j.arth.2015.09.035
Kasparek MF, Kasparek M, Boettner F, Faschingbauer M, Hahne J, Dominkus M (2016) Intraoperative diagnosis of periprosthetic joint infection using a novel alpha-defensin lateral flow assay. J Arthroplast. https://doi.org/10.1016/j.arth.2016.05.033
Suda AJ, Tinelli M, Beisemann ND, Weil Y, Khoury A, Bischel OE (2017) Diagnosis of periprosthetic joint infection using alpha-defensin test or multiplex-PCR: ideal diagnostic test still not found. Int Orthop 41:1307-1313. https://doi.org/10.1007/s00264-017-3412-7
Sigmund IK, Holinka J, Gamper J, Staats K, Bohler C, Kubista B, Windhager R (2017) Qualitative alpha-defensin test (Synovasure) for the diagnosis of periprosthetic infection in revision total joint arthroplasty. Bone Joint J 99-b:66–72. https://doi.org/10.1302/0301-620x.99b1.bjj-2016-0295.r1
Christensen CP, Bedair H, Della Valle CJ, Parvizi J, Schurko B, Jacobs CA (2013) The natural progression of synovial fluid white blood-cell counts and the percentage of polymorphonuclear cells after primary total knee arthroplasty: a multicenter study. J Bone Joint Surg Am 95:2081–2087. https://doi.org/10.2106/jbjs.l.01646
Bauer TW, Hayashi R (2012) The role of the pathologist in diagnosing periprosthetic infection. Surg Pathol Clin 5:67–77. https://doi.org/10.1016/j.path.2011.10.001
Milone MT, Kamath AF, Israelite CL (2014) Converting between high- and low-sensitivity C-reactive protein in the assessment of periprosthetic joint infection. J Arthroplast 29:685–689. https://doi.org/10.1016/j.arth.2013.09.015
Ettinger M, Calliess T, Kielstein JT, Sibai J, Bruckner T, Lichtinghagen R, Windhagen H, Lukasz A (2015) Circulating biomarkers for discrimination between aseptic joint failure, low-grade infection, and high-grade septic failure. Clin Infect Dis Off Publ Infect Dis Soc Am 61:332–341. https://doi.org/10.1093/cid/civ286
Shahi A, Parvizi J (2016) The role of biomarkers in the diagnosis of periprosthetic joint infection. EFORT Open Rev 1:275–278. https://doi.org/10.1302/2058-5241.1.160019
Alvand A, Rezapoor M, Parvizi J (2017) The role of biomarkers for the diagnosis of implant-related infections in orthopaedics and trauma. Adv Exp Med Biol 971:69–79. https://doi.org/10.1007/5584_2017_11
Shahi A, Parvizi J, Kazarian GS, Higuera C, Frangiamore S, Bingham J, Beauchamp C, Valle CD, Deirmengian C (2016) The alpha-defensin test for periprosthetic joint infections is not affected by prior antibiotic administration. Clin Orthop Relat Res 474:1610–1615. https://doi.org/10.1007/s11999-016-4726-2
Acknowledgments
No funding supported this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Yuan, J., Yan, Y., Zhang, J. et al. Diagnostic accuracy of alpha-defensin in periprosthetic joint infection: a systematic review and meta-analysis. International Orthopaedics (SICOT) 41, 2447–2455 (2017). https://doi.org/10.1007/s00264-017-3647-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-017-3647-3