Abstract
Purpose
The purpose of this study was to evaluate the efficacy and safety of percutaneous pedicle screw fixation at the fractured vertebra in the treatment of thoracolumbar fractures.
Methods
Thirty-two consecutive patients were enrolled in the study. All patients received percutaneous pedicle screw fixation, and they were randomly divided into two groups to undergo either the placement of pedicle screws into the fractured vertebra (fractured group) or not (control group). The operation time and intra-operative blood loss were recorded. Oswestry disability index (ODI) questionnaire and visual analogue scale (VAS) as clinical assessments were quantified. Radiographic follow-up was defined by the vertebral body index (VBI), anterior vertebral body height (AVBH), and Cobb angle (CA).
Results
No significant difference was observed in the operation time and intra-operative blood loss between the two groups. Clinical results (VAS and ODI scores) showed no significant difference during all the follow-up periods. In the fractured group, there were better correction and less loss of AVBH and VBI compared with the control group. However, post-operative correction of the CA immediately after surgery and the correction loss at the final follow-up showed no significant difference between the two groups.
Conclusion
Percutaneous screw fixation combined with intermediate screws at the fractured vertebra could more effectively restore and maintain fractured vertebral height, and is an acceptable, minimally invasive surgical choice for patients with type A thoracolumbar fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The thoracolumbar (TL) region of the spine ranges by definition from T11 to L2 inclusively, and nearly 60–70 % of all traumatic spinal fractures occur in this region [1, 2]. The management of thoracolumbar fractures remains controversial, especially in patients without neurological deficit. Although nonoperative treatment has shown promising results, clinical research has demonstrated that surgical treatment provides better fracture reduction and long-term clinical outcomes [3]. Posterior short-segment pedicle instrumentation is most widely used for thoracolumbar fractures around the world because of its three-column fixation [4, 5]. However, traditional open approach can lead to persisting sequelae, such as muscular denervation, atrophy, and pain, mainly owing to extensive paraspinal muscles stripping [6, 7].
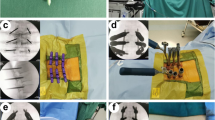
Intra-operative fluoroscopic image of the surgical procedure. (a) Lateral C-arm fluoroscopic image showing the needle reaching the boundaries of the pedicle. (b) Anterior-posterior C-arm fluoroscopic image showing the needle reaching the medial pedicle wall. (c) Insertion of the needle into the vertebra. (d) Insertion of the pedicle screws along the needle. (e) Image of inserting the rod. (f) Intra-operative fluoroscopic image confirming the correct placement of the percutaneous pedicle screw and rod
Pre-operative and post-operative films of a 33-year-old woman with L1 compressive fracture caused by falling from a height.(a), (b), (c) pre-operative films showing a kyphotic deformity and loss of the anterior vertebral body height. (d) Lateral film in the one week after surgery showing the significant improvement of anterior vertebral body height and kyphotic deformity. (e), (f) Lateral films in the six months and one year after surgery indicating no significant correction loss of CA and AVBH
A 28-year-old man with L2 fracture caused by falling from a height. (a), (b), (c) pre-operative films showing a kyphotic deformity and loss of the anterior vertebral body height. (d), (e), (f) Lateral films in the one week, six months, and one year after surgery. A screw breakage was shown in the level above the fractured vertebra in the figure (f)
Recently, minimally invasive percutaneous pedicle screw fixation has been introduced as an alternative approach for the treatment of thoracolumbar fractures, aiming to minimize soft tissue injury and peri-operative morbidity. Some authors [8–10] have proved that percutaneous pedicle screw fixation has some advantages, such as preservation of posterior musculature, less blood loss, shorter operative time, lower infection risk, less post-operative pain, shorter rehabilitation time as well as shorter hospital stay.
In most thoracolumbar fractures, the posterior column of the fractured vertebra remains intact and provides additional points of fixation. Since Dick performed biomechanical studies of pedicle screw fixation in fractured vertebrae in 1994, the technique has evolved, and it has been shown that pedicle screw fixation can achieve stronger fixation and less loss of reduction compared to conventional 4-screw fixation [11–13]. A series of recent biomechanical studies [14–16] confirmed that the addition of intermediate screws could significantly improve the stability of short-segment pedicle screw fixation and reduce the stress on each pedicle screw. To our knowledge, there were few randomized controlled clinical trials to compare the advantage of intermediate screw at the fractured vertebrae in percutaneous screw fixation.
The purpose of this prospective clinical trial was to evaluate the efficacy and safety of percutaneous pedicle screw fixation at the fractured vertebra in treatment of thoracolumbar fractures.
Material and methods
Patient population
This prospective randomized controlled study was conducted between June 2012 and June 2014 in the Department of Spinal Surgery, Liaocheng People’s Hospital, Shandong province, China. In this study, we enrolled 32 patients, who met the following inclusion criteria: age 18–60 years, single-level traumatic fracture of thoracolumbar region (T11-L2), AO type A and absence of neurological deficit, no fracture dislocations, and time to operation after trauma being less than one week. The exclusion criteria was as follow: pathologic or osteoporotic fracture, AO type A4, pregnancy, bilateral pedicle fracture, major fractures of other sites, comorbid injuries involving other major organ systems, or a history of previous spinal surgery.
The study was approved by the Ethics Committee of Liaocheng People’s Hospital and all patients provided written informed consent. Patients were randomly divided into two groups on the basis of the admission date to undergo either the placement of pedicle screws into the fractured vertebra (fractured group) or not (control group).
Surgical procedures
The surgery was performed as described by Wang [17].
All procedures were carried out under controlled general anesthesia with endotracheal intubation. Following induction of general anesthesia, each patient was positioned prone on a radiolucent operating table for spine surgery with chest, abdomen, and pelvis supported by gel pads to allow the spine in a hyperextension position and perform postural reduction. Fluoroscopic images were obtained in the ante-posterior (AP) and lateral planes to ensure that the pedicles could be adequately visualized. Landmarks for pedicle access were drawn on the skin. Entry points were chosen for the pedicles that were to be fitted with instrumentation. An approximately 10–20 mm incision was made at the skin entry point and extended into the underlying subcutaneous tissue. A guide wire was used to perforate the fascia, and a series of sequential dilators were used to dilate the fascia and separate the underlying paraspinal muscles down to the spine. The dilators were removed, and a pedicle pilot hole was made under C-arm fluoroscopic guidance using a tracked awl and a pedicle probe. The chosen pedicles were tapped, and then the appropriate screws were inserted. The axial angulation of the instrument was adjusted until the PAK needle was visualized within the boundaries of the pedicle on the AP view, but lateral to the medial pedicle wall. Bilateral pedicle screws were inserted into the pedicles above and below the fracture. Unilateral or bilateral pedicle screws were placed according to the integrity of the pedicle in the fractured vertebra. After the pedicle screws attached with extenders were inserted, a rod was sited using the special placement system. All steps of pedicle fixation were performed under C-arm fluoroscopic image guidance. A post-operative plain film was obtained to determine satisfactory fixation. The same group of doctors performed all operations. We utilized only one instrumentation technique without grafting fusion (Fig. 1).
Post-operative managements
Patients were routinely administered prophylactic antibiotics for 24 hours and encouraged to start out-of-bed activities with braces within one week post-operatively. However, excessive and heavy activities were forbidden for six months. All patients received mechanical thomboprophylaxis. The implant was routinely removed one to two years post-operatively to avoid the complication such as loose and breakage of pedicle screws. Following discharge from the hospital, all patients were clinically and radiologically assessed in the orthopaedic outpatient clinic every three months.
Observation index
The operation time and intra-operative blood loss were recorded. Functional outcome was assessed by Oswestry disability index (ODI) questionnaire. Back pain was quantified using a visual analogue scale (VAS). Radiographic evaluation consisted of anterior vertebral body height (AVBH), sagittal Cobb’s angle (CA), and vertebral body index (VBI). The AVBH of the injured vertebra and the normal vertebrae above and below the injured vertebra was measured. The percentage of AVBH was calculated as described [18]. The CA was measured between the superior endplate of the upper and the inferior endplate of the lower vertebrae. The VBI was assessed by the relation between the anterior and posterior wall height of the fractured vertebra. All the data were reviewed by an independent observer with no involvement in their treatment.
Statistical analyses
Statistical analyses were performed using the SPSS statistical package, Windows V17.0 (SPSS, Chicago, IL, U.S.A.). The two-sample t test, Chi square test, and ANOVA analysis were used for data analyses. Data were presented as the mean ± standard deviation (SD). For all analyses, a P value <0.05 was considered statistically significant.
Results
The study consisted of 32 consecutive patients, 26 male and six female, with a mean age of 37.7 years (range, 23–55 years). After randomization, the fractured group and control group included 16 patients respectively. Baseline demographic, fracture site and type, and cause of injury of patients in both groups are shown in Table 1. No significant differences were observed between the two groups. The injured vertebrae segments were T12 in three patients, L1 in 22 patients, and L2 in seven patients. Injuries were due to falling from a high height in 16 patients, traffic accidents in 15 patients, and struck by a heavy object in one patient.
Operation time and intra-operative blood loss
The operation time in the control and fractured groups was 54.3 ± 10.7 and 62.4 ± 11.8 min, and intra-operative blood losses were 46.1 ± 9.0 and 50.7 ± 12.0 ml, respectively. There was no significant difference of the operation time and intra-operative blood losses between the two groups (P > 0.05) (Table 2).
Clinical outcomes
Pre-operatively, VAS scores were 6.4 ± 1.8 and 6.9 ± 1.9 points in the control and fractured groups respectively, and these were significantly decreased in both groups during the post-operative period (P < 0.05). However, there was no significant difference of VAS score at the follow-up periods between the two groups (P > 0.05) (Table 3).
At one week, six months, and one year after surgery, ODI scores in both groups were more significantly improved than those before surgery (P < 0.05). However, no significant difference was observed between the control and fractured groups, which showed a similar change with VAS scores (Table 4).
Radiologic outcomes
Significant improvement from baseline in the sagittal Cobb’s angle (CA), vertebrae body index (VBI), and anterior vertebrae body height (AVBH) of the fractured vertebrae was observed in the control and fractured groups (P < 0.05). In the fractured group, the AVBH and VBI were significantly more improved than those of the control group at one week, six months, and one year after surgery (P < 0.05), whereas there was no significant difference of CA between both groups post-operatively (P > 0.05). During the follow-ups of the six months and one year after surgery, the correction losses of the AVBH of the fractured vertebra in the control and fractured groups were 7.1 ± 1.5 and 8.5 ± 1.5; 5.5 ± 1.5 and 6.2 ± 1.5, and those of VBI were 6.1 ± 1.8 and 6.9 ± 1.9, and 2.5 ± 1.3 and 3.2 ± 1.4, respectively, which showed significant difference of the AVBH and VBI between both groups (P < 0.05). However, the correction losses of the CA were 2.7 ± 1.2 and 2.9 ± 1.2 in the control group; 2.3 ± 1.5 and 2.6 ± 1.5 in the fractured group respectively, and there were no significant differences of correction loss (P > 0.05) (Tables 5 and 6).
Surgery-related complication
Only one screw breakage was observed at the one year follow up in the control group. The patient was treated conservatively until the implant was removed. However, he showed a favourable outcome at the last follow-up. There was no non-union and post-operative infection developed in both groups (Figs. 2 and 3).
Discussion
Minimally percutaneous methods of spinal fixation have been developed to avoid the soft tissue damage that comes with traditional open techniques, including muscular denervation, atrophy, and pain [19, 20]. Since Assaker [21] first reported on the application of percutaneous pedicle screw fixation in thoracolumbar trauma, many studies [17, 22–26] were conducted to compare the percutaneous pedicle screw fixation technique with the conventional open approach, which showed that the clinical, functional, and radiological outcomes of the minimally invasive technique were the same as those achieved using the open technique, with a significant reduction in blood loss, post-operative pain, and surgical time. A systematic review and meta-analysis of comparative studies [27] on the percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures showed that there was no difference in efficacy between percutaneous versus open pedicle screw fixation techniques, but the percutaneous approach was associated with shorter surgical time and hospital stay, less intra-operative blood loss and infection rate.
In our study, the intra-operative variables such as operation time (averaged 58.4 min) and blood loss (averaged 48.4 ml) were more favorable than those of open surgeries with short-segmental pedicle screw fixation reviewed in the previous reports [5, 28]. The average correction of Cobb angle and restoration of vertebral body height were comparable with those earlier reported open operations. In addition, the clinical and functional outcomes (VAS for back pain and ODI) were satisfactory, which were also comparable with those of open operations [8]. These facts indicated that percutaneous short-segment posterior stabilization could provide superior radiological and clinical outcome in patients with thoracolumbar fractures.
Traditional short-segment fixation involves pedicle screw placement only at the levels immediately adjacent to the fractured vertebra (one level above and one level below the fracture level). Some authors reported that short-segment pedicle screw instrumentation was not adequate to achieve and maintain the reduction of thoracolumbar fractures and associated with a high rate of failure [29, 30]. This prospective study evaluated the outcomes of 32 patients with monosegmental thoracolumbar fractures who were treated with either percutaneous short-segmental fixation combined with intermediate screws or conventional 4-screw fixation. In the current study, through use of a short-segment technique including fractured level, our radiologic results showed that the initial correction of AVBH from 55.1 ± 12.2 to 89.9 ± 7.7, VBI from 61.8 ± 9.4 to 91.4 ± 8.9 respectively, which were significantly better than those of the control group (AVBH from 55.9 ± 11.4 to 83.5 ± 9.0, VBI from 60.3 ± 10.6 to 85.7 ± 8.3). The correction losses of the AVBH and VBI at the last follow-up were 6.2 ± 1.5 and 3.2 ± 1.4 in the fractured group, 8.5 ± 1.5 and 6.9 ± 1.9 in the control group respectively, and statistical differences were observed between the two groups. However, the initial correction of CA in the fractured group was from 15.6 ± 4.0° to 3.0 ± 1.2° and the correction loss at the last follow-up was 2.6 ± 1.5°, and there was no statistical difference observed compared with the control group (correction from 16.1 ± 5.1° to 3.6 ± 1.4°, the correction loss 2.9 ± 1.2°). These results indicated that pedicle screw fixation at the fractured vertebra did not achieve greater correction of kyphotic angle compared to conventional 4-screw fixation; however, pedicle screw fixation more effectively restored the height of the fractured vertebra, which was similar to the previous study [31].
In this series, the operation time was 54.3 ± 10.7 minutes (control group) and 62.4 ± 11.8 minutes (fractured group) respectively, and no significant difference was observed between both groups. The intra-operative blood loss was (46.1 ± 9.0 vs 50.7 ± 12.0 ml). The results suggested that the use of intermediate screw on the fractured vertebra would not increase the operation time and the blood loss.
Instrumentation failure was observed in one case of the control group. The failure was one screw breakage above the fractured level in one 28-years old patient, which was found at the last follow up. In our opinion, the main reason of the breakage was the increase of stress on the pedicle screw. In our study, all percutaneous pedicle screws were inserted with the assistance of conventional fluoroscopy, and fortunately, there was no malposition of pedicle screws in the two groups. Despite that, we also recommended the use of navigation systems, which could increase the accuracy of percutaneous pedicle screw instrumentation and reduce the fluoroscopic time [32, 33].
There are some limitations to this study. First, this study focused on short-term results (1–12 months), and findings may not be indicative of long-term results, especially after the removal of implants. In addition, this study included a small patient population. Future studies, enrolling more patients and a long-time follow-up period, will be necessary to properly evaluate the usefulness of the technique.
In conclusion, data showed that percutaneous short-segmental fixation combined with intermediate screws could more effectively restore and maintain fractured vertebral height and also was associated with a decrease in the segmental kyphotic angle compared to conventional 4-screw fixation. Percutaneous pedicle screw fixation combined with fracture level screw is an acceptable, minimally invasive surgical choice for patients with type A thoracolumbar fractures.
References
Leucht P, Fischer K, Muhr G, Mueller EJ (2009) Epidemiology of traumatic spine fractures. Injury 40:166–172. doi:10.1016/j.injury.2008.06.040
Tian Y, Zhu Y, Yin B, Zhang F, Liu B, Chen W, Zhang Y (2016) Age- and gender-specific clinical characteristics of acute adult spine fractures in China. Int Orthop 40:347–353. doi:10.1007/s00264-015-3025-y
Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, Rommens PM, ten Duis HJ, Patka P (2006) Treatment of traumatic thoracolumbar spine fractures: a multicenter prospective randomized study of operative versus nonsurgical treatment. Spine 31:2881–2890. doi:10.1097/01.brs.0000247804.91869.1e
McLain RF (2006) The biomechanics of long versus short fixation for thoracolumbar spine fractures. Spine 31:S70–79. doi:10.1097/01.brs.0000218221.47230.dd
Verlaan JJ, Diekerhof CH, Buskens E, van der Tweel I, Verbout AJ, Dhert WJ, Oner FC (2004) Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine 29:803–814
Weber BR, Grob D, Dvorak J, Muntener M (1997) Posterior surgical approach to the lumbar spine and its effect on the multifidus muscle. Spine 22:1765–1772
Kramer M, Katzmaier P, Eisele R, Ebert V, Kinzl L, Hartwig E (2001) Surface electromyography-verified muscular damage associated with the open dorsal approach to the lumbar spine. Eur Spine J 10:414–420
Kim DY, Lee SH, Chung SK, Lee HY (2005) Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine 30:123–129
Grossbach AJ, Dahdaleh NS, Abel TJ, Woods GD, Dlouhy BJ, Hitchon PW (2013) Flexion-distraction injuries of the thoracolumbar spine: open fusion versus percutaneous pedicle screw fixation. Neurosurg Focus 35, E2. doi:10.3171/2013.6.FOCUS13176
Court C, Vincent C (2012) Percutaneous fixation of thoracolumbar fractures: current concepts. Orthopaedics Traumatology, Surgery Res: OTSR 98:900–909. doi:10.1016/j.otsr.2012.09.014
Mahar A, Kim C, Wedemeyer M, Mitsunaga L, Odell T, Johnson B, Garfin S (2007) Short-segment fixation of lumbar burst fractures using pedicle fixation at the level of the fracture. Spine 32:1503–1507. doi:10.1097/BRS.0b013e318067dd24
Gelb D, Ludwig S, Karp JE, Chung EH, Werner C, Kim T, Poelstra K (2010) Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech 23:293–301. doi:10.1097/BSD.0b013e3181af20b6
Dick JC, Jones MP, Zdeblick TA, Kunz DN, Horton WC (1994) A biomechanical comparison evaluating the use of intermediate screws and cross-linkage in lumbar pedicle fixation. J Spinal Disord 7:402–407
Anekstein Y, Brosh T, Mirovsky Y (2007) Intermediate screws in short segment pedicular fixation for thoracic and lumbar fractures: a biomechanical study. J Spinal Disord Tech 20:72–77. doi:10.1097/01.bsd.0000211240.98963.f6
Norton RP, Milne EL, Kaimrajh DN, Eismont FJ, Latta LL, Williams SK (2014) Biomechanical analysis of four- versus six-screw constructs for short-segment pedicle screw and rod instrumentation of unstable thoracolumbar fractures. Spine J 14:1734–1739. doi:10.1016/j.spinee.2014.01.035
Baaj AA, Reyes PM, Yaqoobi AS, Uribe JS, Vale FL, Theodore N, Sonntag VK, Crawford NR (2011) Biomechanical advantage of the index-level pedicle screw in unstable thoracolumbar junction fractures. J Neurosurg Spine 14:192–197. doi:10.3171/2010.10.SPINE10222
Wang H, Zhou Y, Li C, Liu J, Xiang L (2014) Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. J Spinal Disord Tech. doi:10.1097/BSD.0000000000000135
Mumford J, Weinstein JN, Spratt KF, Goel VK (1993) Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine 18:955–970
Mobbs RJ, Sivabalan P, Li J (2012) Minimally invasive surgery compared to open spinal fusion for the treatment of degenerative lumbar spine pathologies. J Clin Neurosci 19:829–835. doi:10.1016/j.jocn.2011.10.004
Smith JS, Ogden AT, Fessler RG (2008) Minimally invasive posterior thoracic fusion. Neurosurg Focus 25, E9. doi:10.3171/foc/2008/25/8/e9
Assaker R (2004) Minimal access spinal technologies: state-of-the-art, indications, and techniques. Joint Bone Spine 71:459–469. doi:10.1016/j.jbspin.2004.08.006
Vanek P, Bradac O, Konopkova R, de Lacy P, Lacman J, Benes V (2014) Treatment of thoracolumbar trauma by short-segment percutaneous transpedicular screw instrumentation: prospective comparative study with a minimum 2-year follow-up. J Neurosurg Spine 20:150–156. doi:10.3171/2013.11.SPINE13479
Lee JK, Jang JW, Kim TW, Kim TS, Kim SH, Moon SJ (2013) Percutaneous short-segment pedicle screw placement without fusion in the treatment of thoracolumbar burst fractures: is it effective?: comparative study with open short-segment pedicle screw fixation with posterolateral fusion. Acta Neurochir 155:2305–2312. doi:10.1007/s00701-013-1859-x
Jiang XZ, Tian W, Liu B, Li Q, Zhang GL, Hu L, Li Z, He D (2012) Comparison of a paraspinal approach with a percutaneous approach in the treatment of thoracolumbar burst fractures with posterior ligamentous complex injury: a prospective randomized controlled trial. J Int Med Res 40:1343–1356
Bronsard N, Boli T, Challali M, de Dompsure R, Amoretti N, Padovani B, Bruneton G, Fuchs A, de Peretti F (2013) Comparison between percutaneous and traditional fixation of lumbar spine fracture: intraoperative radiation exposure levels and outcomes. Orthopaedics Traumatology, Surgery Research: OTSR 99:162–168. doi:10.1016/j.otsr.2012.12.012
Li H, Yang L, Xie H, Yu L, Wei H, Cao X (2015) Surgical outcomes of mini-open Wiltse approach and conventional open approach in patients with single-segment thoracolumbar fractures without neurologic injury. J Biomed Res 29:76–82. doi:10.7555/jbr.29.20140083
Phan K, Rao PJ, Mobbs RJ (2015) Percutaneous versus open pedicle screw fixation for treatment of thoracolumbar fractures: Systematic review and meta-analysis of comparative studies. Clin Neurol Neurosurg 135:85–92. doi:10.1016/j.clineuro.2015.05.016
Heintel TM, Berglehner A, Meffert R (2013) Accuracy of percutaneous pedicle screws for thoracic and lumbar spine fractures: a prospective trial. Eur Spine J 22:495–502. doi:10.1007/s00586-012-2476-8
McLain RF, Sparling E, Benson DR (1993) Early failure of short-segment pedicle instrumentation for thoracolumbar fractures. A preliminary report. J Bone Joint Surg Am 75:162–167
Gurwitz GS, Dawson JM, McNamara MJ, Federspiel CF, Spengler DM (1993) Biomechanical analysis of three surgical approaches for lumbar burst fractures using short-segment instrumentation. Spine 18:977–982
Tian JW, Wang L, Xia T, Liu CY, Zhao QH, Dong SH (2011) Posterior short-segmental fixation combined with intermediate screws vs conventional intersegmental fixation for monosegmental thoracolumbar fractures. Orthopedics 34:e389–396. doi:10.3928/01477447-20110627-08
von Jako R, Finn MA, Yonemura KS, Araghi A, Khoo LT, Carrino JA, Perez-Cruet M (2011) Minimally invasive percutaneous transpedicular screw fixation: increased accuracy and reduced radiation exposure by means of a novel electromagnetic navigation system. Acta Neurochir 153:589–596. doi:10.1007/s00701-010-0882-4
Bourgeois AC, Faulkner AR, Bradley YC, Pasciak AS, Barlow PB, Gash JR, Reid WS Jr (2015) Improved accuracy of minimally invasive transpedicular screw placement in the lumbar spine with 3-dimensional stereotactic image guidance: a comparative meta-analysis. J Spinal Disord Tech 28:324–329. doi:10.1097/bsd.0000000000000152
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, K., Li, Z., Ren, X. et al. Effect of the percutaneous pedicle screw fixation at the fractured vertebra on the treatment of thoracolumbar fractures. International Orthopaedics (SICOT) 40, 1103–1110 (2016). https://doi.org/10.1007/s00264-016-3156-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-016-3156-9