Abstract
Introduction
It has been shown that the distance between the joint line (JL) and the fibular head is constant in both knees in a given individual. We analysed the influence of the JL level difference between the revised knee and the native knee from the functional outcomes after TKR revision.
Methods
This multicentre study assessed retrospectively a consecutive series of 177 revised total knee replacements. Patients with contralateral knees that had undergone previous major surgery or trauma were excluded. The JL level difference between both knees was measured on Knee’s AP standing X-rays and compared to the KSS Knee and Function scores at the final follow-up.
Results
Eighty-five cases were analysed at a mean of seven years follow-up. There was a significant increase in KSS Knee and Function scores after surgery. The average elevation of the JL was 2.2 mm (s.d. 2.66 mm) compared with the healthy contralateral knee. When the JL was elevated more than 4 mm this correlated with a decreased KSS Function score and decreased post-operative knee flexion.
Conclusions
Poorer functional results are significantly associated with an elevation in the JL compared to the contralateral healthy knee. In those patients with a suitable contralateral knee the JL level to restore can be assessed by the distance between the femoral condyle and the apex of the fibular head of the contralateral knee.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The significant increase of total knee replacement (TKR) raised the number of subsequent revision procedures needed. According to a recent study on 300,000 primary TKR, the revision rate was 4 % after five years and 8.9 % after nine years [1]. The revision of a total knee is a challenge. Rigorous pre-operative planning is essential and helps to anticipate difficulties that may occur during the operation such as skin and soft tissue cover, bone defects, ligament laxity and balancing, choice of the constraint and joint line level restoration [2].
Joint line (JL) restoration is one of the keys to a successful revision TKR as it impacts all the knee kinematics [3–6]. Knee ligament balancing and joint isometry may depend on restoration of the JL for a successful revision TKR [3–8]. These principles are based on established concepts proposed by Ludwig Burmester, a German mathematician of the nineteenth century, and adapted by Menschik establishing two isometric curves: one femoral and one tibial [9, 10]. If both ligament’s insertions are located on the Burmester’s curves and its fibres pass through the instantaneous centre of rotation of the knee, the ligament can be considered as isometric during the full range of movement of the knee (Fig. 1). The collaterals and cruciate ligaments follow this model (Fig. 1) [9, 10]. From a clinical viewpoint this means that the joint space remains isometric (same gap in flexion and extension) if the joint centre of rotation is constant (preservation of the JL) and the ligaments’ length remain constant in flexion and extension (fine ligaments balancing).
Isometric ligaments — Burmester curves described by Menschik. a: The fibers of the four ligaments (ACL/PCL, MCL and LCL) have their fibres passing through the instantaneous centre of rotation of the knee. b: The insertions (both proximal and distal) of the four ligaments (ACL/PCL, MCL and LCL) are on the Burmester curve (red line) c: The ligaments remain isometric during the full range of movement of the knee
Restoration of the JL based on the femoral condylar surfaces and the tibial plateau is usually less complicated in a primary TKR. However, bone loss due to implant failure or prior surgery may complicate it drastically. Menschik concept can allow to simplify the revision procedure. However, it is based on two essential pre-requisites; firstly the preservation of the centre of rotation and thus the JL level and secondly the presence of functional collateral ligaments. Where the latter are incompetent, e.g. by overstretching due to poor primary implant position or iatrogenic injury, then constrained implants need to be considered. However a precise JL level restoration remains mandatory.
Several radiological landmarks are described to measure the JL level: hip and ankle centres, femoral epicondyles, the anterior tibial tuberosity and the apex of the fibular head [7, 11–15]. However, the inter-individual variability of these markers is marked thus are not reliable in assessing the true level of the JL. However, it has been demonstrated that there is symmetry in the human skeleton [13]. Maderbacher et al. found that the mean difference of the distance between the JL and the fibular head apex (FH) between the two knees of a single individual was 0.0 mm (CI 95 % [−1.1,1.1]) regardless of gender, age and degree of osteoarthritis (intraclass correlation coefficient 0.98) [13]. We studied the influence of the JL level difference between the revised and the healthy knee measured by this technique, on revised TKR (RTKR) medium-term outcomes.
Our hypothesis was that functional outcomes are correlated to a difference between the revised and the native joint line level.
Materials and methods
A multicentre study involving a consecutive series of 347 RTKR was performed between 2000 and 2010 in five University Hospitals.
Study cohort
Of the 347 cases, 74 had died, 69 were lost to follow-up and 27 were patients undergoing unicompartmental knee revisions, then 177 patients corresponding to 177 RTKR were reviewed. All patients reviewed with a standing AP radiograph of both knees were included. Fourteen patients with trauma injury as well as patients with surgical replacement (79) or severe osteoarthritis (28 Kellgren Lawrence grade 4) of the contralateral knee were excluded. Arthroscopy was not considered as exclusion criteria. The study cohort therefore comprised 85 patients. Patient specific data collected included age, American Society of Anesthesiology score (ASA), body mass index (BMI), failure mode (aseptic or septic), symptoms (loosening, instability, pain), the surgical approach used for revision, the ligaments status, the bone loss (Anderson Orthopedic Research Institute Classification), the revised components (tibial, femoral, both), the type of implants and the use of bone grafts, wedges or trabecular cone.
Radiological analysis
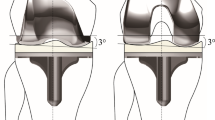
Radiological analysis was done on calibrated standardized AP standing’s X-rays of both knees performed at the last follow-up. An independent blinded observer measured the JL level both on the healthy and the revised side on two separate occasions with an interval of 30 days. The JL was defined as the distance between the tangent to the lower edge of the femoral condyle bone or implant and the parallel passing through the apex of the fibular head (Fig. 2). The outcome used was the mean of the two measurements. The difference of measure between the revised side (revised JL) and the healthy side (native JL) corresponded to the JL level difference. The JL was therefore restored ([absolute difference] < 4 mm), raised (revised JL - native JL ≥ + 4 mm) or lowered (revised JL - native JL ≥ − 4 mm) after revision according to data from Fornalski and Martin [16, 17].
Functional outcomes
The International Knee Society (KSS) score separated into Knee and a Function scores (100 points each) was used as the functional outcome assessment. It was compared pre-operatively and at the final follow-up. The range of motion (flexion and extension) of the operated knee was also measured pre-operatively and at final follow-up.
Statistical method
We investigated if there was a correlation between the calculated joint line level difference and the KSS score measured at the final follow-up. The verification of the normality of the distributions of quantitative variables was performed by the method of Shapiro-Wilk. Man-Whitney (unpaired) or Wilcoxon (matched series) nonparametric tests were used to compare the distributions of quantitative variables that do not follow a normal distribution. Kruskal Wallis nonparametric tests were performed to compare the distributions of quantitative variables with more than two categories that do not follow the normal distribution and the Friedman test was used for paired data. ANOVA tests were performed to compare KSS score, range of motion and JL level according to bone loss. To assess inter and intra-observer variations of the measurement technique intraclass correlation coefficients were calculated. The search for correlations between quantitative variables was performed by Spearman test. The significance threshold selected for all the statistical analysis was 0.05. Statistical analysis was performed by the Biostatistics department of Limoges University Hospital using the XLSTAT® software (v.2015, Addinsoft, Paris, France).
Results
The demographics, symptoms, surgical approach, and implants used are reported in Table 1.
The intra and inter-observers agreement (intraclass correlation coefficients) of the measurements were respectively 0.94 and 0.98.
Table 2 shows the mean JL level and the mean JL level difference.
The mean JL level was 15.2 mm (s.d. 2.9 mm, CI 95 %: 14.6 to 15.9) on the healthy side and 17.4 mm (s.d. 3.1 mm, CI 95 %: 16.8 to 18.1) on the revised side. The revised JL level was elevated by a mean of 2.2 mm (s.d. 2.7 mm, CI 95 %: 1.6 to 2.8) which was statistically significant (p <0.001). The JL level difference was not altered by the use of wedges or bone graft (p = 0.61), the thickness of polyethylene (p = 0.23), the ligaments status (p = 0.06), the septic status (p = 0.57) or the need of a tibial tubercle osteotomy (p = 0.48) and the type of implant (p = 0.55). For the posterior stabilized and rotary hinge implants, the JL level difference was 1.9 mm (s.d. 2.7 mm, CI 95 %: 1.2 to 2.8) and 2.4 mm (s.d. 2.5 mm, CI 95 %: 1.5-3.3) respectively. Bone loss Anderson type I, IIa and IIb did not interfere with JL level difference (p = 0.12). For major bone loss, Anderson type III, the JL level difference was 2.9 (s.d. 2.3 CI 95 % 1.7 to 3.9) which was statistically significant (p = 0.031).
As defined, successful JL restoration was obtained in 56 cases. JL level was raised and lowered in 25 and four cases respectively.
Table 3 shows the KSS outcome scores according to the JL difference.
Pre-operative mean Knee and Function KSS scores were 51 (s.d.12, CI 95 %: 48–54) and 46 (s.d.12, CI 95 %: 44–49). Post-operative scores were 75 (s.d. 14, CI 95 %: 71–78) and 65 (s.d.16, CI 95 %: 62–70). The mean differences of 24 (s.d. 15) and 19 (s.d. 13) points were statistically significant (p <0.001).
There was a weak but statistically significant correlation between KSS Function score and the JL difference (Spearman coefficient = −0.416, p = 0.047) (Fig. 3). This was not demonstrated with regard to the KSS Knee score.
The mean flexion was 98° (s.d.19°, CI 95 %: 93–102) pre-operatively and 103° (16°, CI 95 %: 96–104) at final follow-up. There was a mean fixed flexion deformity 2° (s.d. 5°, CI 95 % 1–3) before revision and 3° (s.d. 7°, CI 95 %: 1–5) at final follow-up. This was not statistically significantly different.
Similarly there was a weak but statistically significant correlation between the JL difference and post-operative flexion (Spearman coefficient = −0.468, p = 0.013), not demonstrated with regards to the extension.
Patients with a 4 mm or more elevation of the revised JL had a statistically reduced post-operative KSS Function score: 59 (s.d. 16) vs 68 (s.d. 14) (p = 0.027) and flexion: 92° (s.d. 20°) vs 106° (s.d. 11°) (p = 0.014).
Patients with an Anderson type III also had statistically reduced KSS Function score 58 (s.d. 14, CI 95 %: 53–62) but without impairment of their range of motion.
Tibial tubercle osteotomy was associated with a poorer post-operative KSS Function score (−8 points) and poorer flexion (−13°) compared to revised knees without a tibial tubercle osteotomy (Table 3). There was no difference between septic and aseptic RTKR with respect to age at the time of revision, ASA score and BMI. Septic RTKR was associated with a significantly shorter time before revision (p = 0.042) and lower mean pre-operative flexion (92° (s.d. 20°, CI 95 %: 89–95)) compared to aseptic RTKR (104° (s.d.13°, CI 95 %: 101–105)). The final follow-up KSS Function score was significantly better in aseptic revision. Patients revised for sepsis had significantly more post-operative fixed flexion deformity than aseptic revisions (Table 3). However linear regression analysis failed to show the influence of both tibial tubercle osteotomy and septic status on the KSS/JL association (1.2, p = 0.11 ; 1.4, p = 0.08).
Discussion
This study has shown that elevation of the native JL in a revision TKR above 4 mm is associated with a worse post-operative function at a mean follow-up of seven years. In particular the KSS Function score and post-operative flexion decreases with elevation of the JL. Elevation of the JL directly affects the extensor apparatus by lowering the patella [1, 4, 19]. It may also create an impingement between the patella and the polyethylene insert or tibial plateau itself. Therefore, JL alteration is likely responsible for inferior clinical results as well as reduced long-term survival [6, 17, 18].
Several studies already described a negative influence on the clinical results of primary or revised TKR if the JL was elevated. However, depending on the report and the measurement method, less favourable results were shown if the joint line level was elevated more than 4, 5 or 8 mm [3, 6, 17–20]. Bieger et al. found a statistical difference in post-operative KSS score between restored JL assessed by femoral ratio method (164 vs 138; p < 0.0001), but this difference was not shown when using the Figgie measurement method (162 vs 152; p = 0.09) [21]. This emphasizes the difficulties to compare the results of the different studies and the importance of the assessment method chosen [21].
Worse KSS Function results and significant JL elevation were also found for major bone loss (Anderson type III). Actually in the case of major bone loss and/or collateral ligament failure, rotating hinge implants are the only reliable solution to obtain a reconstructed stable knee. Nevertheless, it does not intrinsically restore the knee JL at the anatomical level and the complexity of the procedure associated with bone loss can explain both the worse KSS score and the rise of the JL level. Finally, joint line elevation can occur due to excess femoral bone resection (or loss) or by inserting thicker polyethylene (or tibial wedge) to tension ligaments. However, if in the first case it’s often an assessment error of the surgeon; in the second case it’s a deliberate choice based on a compromise to treat soft tissue lesions without using constraint implant. Furthermore, our result showed a tendency to JL elevation after RTKR and as JL elevation is correlated with poor outcomes, when balancing the knee, we advocate the use of femoral distal wedge that will distalize the femoral component and prevent JL elevation.
Once it is agreed that the JL level should be restored to the anatomical position, the method for achieving this is disputed. Several bony landmarks have been proposed. The lower pole of the patella is not a reproducible marker because of its mobility and the possible contracture of the patellar tendon [12, 22, 23]. The distance to the anterior tibial tuberosity which varies from 10 mm to 32 mm, and the distance to the medial epicondyle from 23 mm to 35 mm [12, 21–23].
The apex of the FH can range from 4 to 29 mm to the JL depending on the studies [12, 14, 22, 23]; we found the range was 8 mm to 22 mm. Servien et al. studied 200 normal knees MRI measurement and found a range from 4 to 22 mm (mean 14.11, s.d. 3.04). They stated that this wide variation, independent of patient size, was too large to validate the FH as a reliable landmark [23]. Luyckx et al. found a FH mean of 15.1 (s.d. 3.7) with wide variation and a poor correlation (r = 0.13) to the femoral width. However, Servien and Luyckx did not study if symmetry exists between both knees. Havet et al. performed 25 bilateral knee FH measurements and calculated the difference. No statistically significant difference was noted between the mean values but the differences were higher to the defined limits in too many cases to validate it. However, they did not used scaled X-rays, which may have impaired their results.
With each method significant inter-individual anatomical variations do not produce a reliable JL level from an absolute value. To overcome this Rajagopal et al. [24] studied ratios and showed that that the distance between the joint line level and the trans-epicondylar axis was constant regardless of sex and size of the individual and was equal to one third of the intercondylar distance [24]. In the same meaning Iacono and Luyckx assess the importance of the adductor tubercle as a bony landmark for the ratio technique [14, 25].
Using the symmetry of the human skeleton, as Maderbacher et al. we have overcome the inter-individual variation using the contralateral healthy knee JL level. Furthermore, a huge advantage in assessing the JL via the fibular head is the fact that this landmark can be easily identified during surgery. Major femur or tibia bone loss can make it difficult to find their related bony landmarks and so impaired the measurements even when using a ratio technique.
Our study has several limitations. First, the number of patients lost to follow-up is significant. The methodology requires a healthy contralateral knee with radiological images taken under reproducible and standardized conditions; and even measurement bias can persist. Furthermore, we report that bone loss is associated with an increased joint line, which could confound the conclusions, as the severity of bone loss could affect the functional outcomes, rather than the JL elevation itself. Due to the limited number of patients some of our statistical analysis may be underpowered. So even if no influence was found on the linear regression analysis, tibial tubercle osteotomy as well as the septic status may be confounders impairing the outcomes rather than the JL elevation itself. Also our study does not provide support for the planned restoration of the joint line using this radiological technique results in better functional outcomes compared to other methods. To confirm this would require a randomized controlled trial comparing this technique to a control group where joint line restoration is calculated by a different technique. Moreover our results are correlations without proven cause and effect. It may be possible that functional results and JL elevation varies in the same way but according to other factors. This emphasizes the need of further better designed studies.
In conclusion, in revision TKR, the joint line level to restore can be assessed by means of fibular head/JL distance measured on X-rays taken of the contralateral healthy knee. In this retrospective multi-centre study elevation of the joint line above 4 mm, measured by this technique, correlated with poor functional outcome and decreased range of motion. In suitable patients this method of assessing the joint line level may be useful in revision TKR.
References
Dy CJ, Marx RG, Bozic KJ, Pan TJ, Padgett DE, Lyman S (2014) Risk factors for revision within 10 years of total knee arthroplasty. Clin Orthop Relat Res 472:1198–1207
Gustke KA (2005) Preoperative planning for revision total knee arthroplasty: avoiding chaos. J Arthroplasty 20(S2):37–40
Bellemans J (2004) Restoring the joint line in revision TKA: does it matter? Knee 11:3–5
Khakharia S, Scuderi GR (2012) Restoration of the distal femur impacts patellar height in revision TKA. Clin Orthop Relat Res 470:205–210
Selvarajah E, Hooper G (2009) Restoration of the joint line in total knee arthroplasty. J Arthroplasty 24:1099–1102
Porteous AJ, Hassaballa MA, Newman JH (2008) Does the joint line matter in revision total knee replacement? J Bone Joint Surg (Br) 90:879–884
Victor J, Bellemans J (2006) Physiologic kinematics as a concept for better flexion in TKA. Clin Orthop Relat Res 452:53–58
Hofmann AA, Kurtin SM, Lyons S, Tanner AM, Bolognesi MP (2006) Clinical and radiographic analysis of accurate restoration of the joint line in revision total knee arthroplasty. J Arthroplasty 21:1154–1162
Menschik A (1974) Mechanics of the knee joint, part I (author’s transl). Z Für Orthop Ihre Grenzgeb 112:481–495
Menschik A (1975) Mechanics of the knee joint, part II, the final rotation (author’s transl). Z Für Orthop Ihre Grenzgeb 113:388–400
Maderbacher G, Keshmiri A, Schaumburger J, Springorum H-R, Zeman F, Grifka J et al (2014) Accuracy of bony landmarks for restoring the natural joint line in revision knee surgery: an MRI study. Int Orthop 38:1173–1181
Mason M, Belisle A, Bonutti P, Kolisek FR, Malkani A, Masini M (2006) An accurate and reproducible method for locating the joint line during a revision total knee arthroplasty. J Arthroplasty 21:1147–1153
Maderbacher G, Keshmiri A, Zeman F, Grifka J, Baier C (2014) Assessing joint line positions by means of the contralateral knee: a new approach for planning knee revision surgery? Knee Surg Sports Traumatol Arthrosc 23:3244–3250. doi:10.1007/s00167-014-3157-4
Luyckx T, Beckers L, Colyn W, Vandenneucker H, Bellemans J (2014) The adductor ratio: a new tool for joint line reconstruction in revision TKA. Knee Surg Sports Traumatol Arthrosc 22:3028–3033
Havet E, Gabrion A, Leiber-Wackenheim F, Vernois J, Olory B, Mertl P (2007) Radiological study of the knee joint line position measured from the fibular head and proximal tibial landmarks. Surg Radiol Anat 29:285–289
Fornalski S, McGarry MH, Bui CNH, Kim WC, Lee TQ (2012) Biomechanical effects of joint line elevation in total knee arthroplasty. Clin Biomech (Bristol, Avon) 27:824–829
Martin JW, Whiteside LA (1990) The influence of joint line position on knee stability after condylar knee arthroplasty. Clin Orthop Relat Res 259:146–156
Partington PF, Sawhney J, Rorabeck CH, Barrack RL, Moore J (1999) Joint line restoration after revision total knee arthroplasty. Clin Orthop Relat Res 367:165–171
Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH (1986) The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am 68:1035–1040
Babazadeh S, Dowsey MM, Swan JD, Stoney JD, Choong PFM (2011) Joint line position correlates with function after primary total knee replacement: a randomised controlled trial comparing conventional and computer-assisted surgery. J Bone Joint Surg (Br) 93:1223–1231
Bieger R, Huch K, Kocak S, Jung S, Reichel H, Kappe T (2014) The influence of joint line restoration on the results of revision total knee arthroplasty: comparison between distance and ratio-methods. Arch Orthop Trauma Surg 134:537–541
Laskin RS (2002) Joint line position restoration during revision total knee replacement. Clin Orthop Relat Res 404:169–171
Servien E, Viskontas D, Giuffrè BM, Coolican MRJ, Parker DA (2008) Reliability of bony landmarks for restoration of the joint line in revision knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 16:263–269
Rajagopal TS, Nathwani D (2011) Can interepicondylar distance predict joint line position in primary and revision knee arthroplasty? Am J Orthop (Belle Mead NJ) 40:175–178
Iacono F, Raspugli GF, Filardo G, Bruni D, Zaffagnini S, Bignozzi S et al (2015) The adductor tubercle: an important landmark to determine the joint line level in revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 22:3034–3038. doi:10.1007/s00167-013-2809-0
Acknowledgments
The authors are very grateful to Professor Bonnevialle (Toulouse University Hospital, France), Professor Mertl (Amiens University Hospital, France), Professor Rouvillain (Fort de France University Hospital, France), Professor Bizot (Angers University Hospital, France), Dr Dalmay (Amiens University Hospital) for contributing as investigators to this work.
The authors are very grateful to Professor Simon Donell (Norfolk & Norwich University Hospital, UK) and to Mr Max Gibbons (Nuffield Orthopedic Centre, Oxford, UK) for providing language help and proof reading of the article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Level of evidence: Retrospective study, level IV.
All authors were fully involved in the study and preparation of the manuscript and the material within has not been and will not be submitted for publication elsewhere.
Rights and permissions
About this article
Cite this article
Clavé, A., Le Henaff, G., Roger, T. et al. Joint line level in revision total knee replacement: assessment and functional results with an average of seven years follow-up. International Orthopaedics (SICOT) 40, 1655–1662 (2016). https://doi.org/10.1007/s00264-015-3096-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-3096-9