Abstract
Purpose
Restoring the joint line (JL) improves clinical and functional outcome in total knee arthroplasty (TKA). Therefore, anatomical landmarks to approximate the JL have been published. So far, the natural deviation of the JL 90° to the mechanical tibial axis has not been considered. Thus, we designed this study to: (1) determine the natural JL of knees in healthy persons in respect to the mechanical tibial axis, (2) validate and double-check intra-operative bony landmarks already been published in respect to the natural JL and (3) find possible correlations between distances from bony landmarks to the JL and femoral and tibial width.
Methods
Eighty MRI scans of knees of healthy persons were examined by two independent observers. Distances from the tip of the fibular head (FH), the medial (ME) and lateral (LE) epicondyles and the adductor tubercle (AT) to the JL within the medial and lateral compartment were measured. Further, we determined the orientation of the JL in respect to the mechanical axis of the tibia. Interobserver correlations were calculated. Differences were analyzed using Student’s t test. Linear regression models were calculated to analyze correlations.
Results
Interobserver correlation was excellent. Mean JL deviation was 4.2° varus. Distance between the FH, ME, LE and AT to the JL within the medial compartment was 12.2, 33.9, 33.4 and 45.4 mm, respectively. Within in the lateral compartment, distances were 15.3, 31.0, 30.6 and 42.3 mm to the JL. Strong correlation was found between femoral width and distances from the AT, ME and LE to the JL.
Conclusion
In TKA, the JL is usually altered due to the classic resection technique, which does not respect the natural deviation of the JL. Estimating the natural JL by adding absolute values to bony landmarks, as proposed in the literature, is not recommended. According to our data, the JL can be best estimated by adding the calculated value: 6.40 + (width femur [mm] × 0.49) to the AT.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Despite anticipated changes in the philosophy surrounding total knee arthroplasty (TKA), restoring the joint line (JL) of the natural knee remains one of the major goals. Changes of the JL, whether elevated or descended, is associated with poor outcome, as the craniocaudal position of the patella and tibiofemoral kinematic and joint stability are altered [1–5]. Restoring the JL is reproducible in primary surgery when the natural anatomy of the knee joint is present. In the so-called measured resection technique in particular, the original JL can be preserved [5]. However, difficulties appear in revision surgery when both cartilage and bone have already been removed in prior surgeries [4, 6]. The JL can be rebuilt relative to the existing TKA but carries the risk of reconstructing a JL that was already altered in primary surgery. Therefore, anatomical landmarks to reconstruct the JL were published: for the fibular head (FH), a distance to the JL of 10 mm is reported [7, 8]. Stiehl and Abott [9] investigated the distal femoral anatomy and found a mean distance from the medial and lateral (epi)condyle to the JL of 30.8 and 25.3 mm, respectively. Iacono et al. [10] showed a mean distance from the adductor tubercle to the JL of 48.7 mm.
In general the natural JL is not orthogonal to the tibial mechanical axis but in 87 ± 3° varus to it [11, 12]. In the event of performing a so-called “classic alignment technique” in TKA, the proximal tibia is cut normally (90°) to the tibial mechanical axis and the femur is cut normally (90°) to the femoral mechanical axis. In case of performing a so-called “anatomical alignment technique,” the natural JL of some degrees of varus is respected in both cuts in the distal femur and the proximal tibia. Nowadays, the classic resection is typically performed. In revision surgery, when long stems are used, the proximal tibia must be cut normally to the mechanical tibial axis so that straight stems can be inserted. However, the classic resection technique, when using symmetric implants, is particularly associated in varus knees, with an increased resection of the medial femoral compartment in comparison with the lateral femoral compartment and vice versa for the tibial bone: this creates a slightly valgisated JL in relation to the tibial mechanical axis, theoretically of an average of 3°. Thus, the JL is preserved in the medial and distalised in the lateral compartment.
Reviewing recent publications, the natural JL deviation to the mechanical tibial axis has not been considered when assessing distances from anatomic landmarks to the JL or determining pre- to postoperative JL changes after TKA. Thus, we designed this study to: (1) determine the JL of knees in healthy persons in respect to the mechanical tibial axis, (2) validate and double check published reports of intra-operative bony landmarks in respect to the natural JL and (3) find possible correlations between distances from bony landmarks to the JL and femoral and tibial width.
Methods
Eighty magnetic resonance imaging (MRI) scans (Philips Healthcare Ingenia 1.5 T, Siemens Magnetom Avanto 1.5 T and Siemens Magnetom Espree 1.5Tesla) of knees undergoing routine diagnosis following acute meniscal or cruciate ligament trauma were examined. No MRIs were solely performed for this study. According to our local ethical committee, no approval was necessary. Only knees with intact cartilage were included. MRI scans of patients >30 years of age were only included in this study if these patients had a recently performed arthroscopy that found no cartilage damage or osteoarthritis. Knees with osteochondral lesions, osteoarthritis, prior knee surgery other than recent arthroscopy with confirmed intact cartilage, deviations of the leg axis (anatomic femorotibial angle <173 or >175°) or immature skeletons were excluded. In order to analyse gender differences, male and female patients were included. All measurements were independently performed by two observers (GM, CB).
MRI measurements
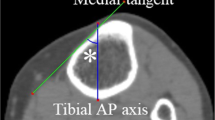
All measurements were performed using the AGFA Healthcare IMPAX Software (53227 Bonn, Germany) using T1-weighted coronal, axial and sagittal planes. In all three planes, the anatomical landmarks [tip of the FH, medial epicondyle (ME), lateral epicondyle (LE), adductor tubercle (AT), most distal point of the medial (MFC) and lateral (LFC) femoral condyle] and the femoral and tibial anatomic/mechanical axis were identified. The JL was defined as the line connecting the MFC and LFC (Fig. 1).
Femoral and tibial axes and Joint Line. The tibial mechanical axis is defined by connecting the midpoint of the tibial spines with a point determined as the centre of the tibial shaft. For the femoral mechanical axis a line from the midpoint of the distal femur to the midpoint of the centre of the shaft was drawn. The angle between the femoral and mechanical axes was measured. The articulation site between the femur and the tibia was determined by identifying the most distal point of the medial femoral condyle (MFC) and most distal point of the lateral femoral condyle (LFC) (see dots). The Joint Line was defined by connecting the MFC and LFC
A line perpendicular to the anatomical axis of the tibia (imitating the classic resection technique) was drawn at the level of the most proximal tip of the FH [13–16]. To determine the distance from the FH to the JL in either the medial or the lateral compartment, measurements from the perpendicular line at the level of the FH to the MFC (FHMFC) and to the LFC (FHLFC) were performed. The width of the proximal tibia was measured from the most medial and lateral osseus border. Next, orientation of the JL in comparison with the mechanical tibial axis was investigated. Therefore, the mediolateral distance between the MFC and LFC was measured and the difference between the FHMFC and the FHLFC via subtraction calculated. Via a trigonometric function, the degree in varus of the JL in comparison with the perpendicular line to the mechanical tibial axis could be calculated: sinAlpha = (FHMFC − FHLFC)/(distance MFC to LFC).
As all legs were well aligned and had no varus or valgus malalignment (femorotibial angle 173–175°), the line perpendicular to the tibial mechanical axis was parallelised and placed exactly on the ME, LE and AT. Accuracy of this parallelised line was double checked by comparing it with the line in 174° of valgus to the anatomical femoral axis, whereby only a difference of ± 1° was permitted. The shortest perpendicular distances from the line through the AT to the MFC and LFC (ATMFC, ATLFC), from the ME (Fig. 2) to the MFC and LFC (MEMFC, MELFC) and the distance from the LE to the MFC and LFC (LEMFC, LELFC) were measured to investigate distances from bony femoral landmarks to the JL, again considering both the medial and lateral compartments.
Distance from the medial epicondyle (ME) to the Joint line. A line perpendicular to the mechanical axis of the tibia was parallelised and placed on the medial epicondyle. The distance between the parallelised line and the MFC (yellow dot) was measured and defined as the distance between the medial epicondyle to the JL within the medial compartment (MEMFC). In this case we measured 28.8 mm. The same procedure was repeated in order to obtain the distance from the medial epicondyle to the lateral compartment (MELFC). In this case we measured 24.3 mm. The angle between the mechanical femoral axis and the parallelised line was measured. In this case we found 6°
All measured distances (FHMFC, FHLFC, MEMFC, MELFC, LEMFC, LELFC, ATMFC and ATLFC) were compared with proposed values in the literature. The distance between the ME and LE was measured to determine femoral width. To account for the different knee ratios, absolute measurements of ATMFC, ATLFC, LEMFC, LELFC, MEMFC and MELFC were divided by femoral width; FHMFC and FHLFC were divided by tibial width.
Statistical methods
To assess interobserver correlations, intraclass correlation coefficients [ICC (3,1), absolute agreement] were calculated. Due to the good agreement between both raters, we calculated mean values of both measurements for further analyses. Continuous data are presented as mean and range or as mean and standard deviation (SD). Differences to a constant and between male and female patients were analysed using Student’s t test. Linear regression models were calculated to analyse correlations between tibial and FHMFC and FHLFC and between distal femoral width and MEMFC, MELFC, LEMFC, LELFC, ATMFC and ATLFC. A two-sided P value of ≤0.05 was considered to indicate statistical significance. All analyses were performed using IBM SPSS Statistics 21.0.0.1 and R (version 3.0.1).
Results
We examined 80 knees in patients with an average age of 29.6 years (40 male patients). Interobserver correlation was excellent for all measurements: 0.93 for FHLFC, 0.83 for FHMFC, 0.99 for tibial width, 0.99 for femoral width, 0.88 for MEMFC, 0.89 for MELFC, 0.86 for LEMFC, 0.92 for LELFC, 0.94 for ATMFC and 0.91 for ATLFC.
Joint line
Mean JL deviation in respect to the line perpendicular to the tibial mechanical axis was 4.2° varus (4.1 in male vs. 4.3 in female patients, p = 0.46). The distance from the perpendicular line to the mechanical axis of the tibia showed a mean difference between FHMFC and FHLFC of 3.1 (range 1.1-6.2) mm. We found no differences between the knees of male and female patients and no correlation between FHMFC and FHLFC and proximal tibial or distal femur width.
Proximal tibia
The average width of the tibia was 74.5 mm (range 61.0–86.9), with a significant difference (p < 0.001) between male and female patients: 79.3 (SD 4.1) vs. 69.7 (SD 4.0), respectively.
Fibular head
FHMFC was 12.2 mm [range 3.2–19.5; male 12.6 (SD 3.2) vs. female 11.8 (SD 3.3) patients; p = 0.24)] Mean FHLFC distance was 15.3 mm [range 6.0–22.; male 15.8 (SD 2.9) vs. female 14.9 (SD 3.3) patients; p = 0.18). Table 1. There was no significant correlation between tibial width and FHMFC (p = 0.21) or FHLFC (p = 0.23).
We found a significant difference of an average of 2.2 mm for the FHMFC and 5.3 mm for the FHLFC (both p < 0.001) in comparison with the proposed distance of 10 mm from the FH to the JL (Table 2 and Fig. 4).
Distal femur
The average width of the distal femur was 79.9 (range 66.0–95.7) mm, with a significant difference (p < 0.001) between male and female patients [84.8 (SD 5.1) vs. 74.9 (SD 4.9)] (Table 1).
Medial femoral epicondyle
The MEMFC was 33.9 mm (range 26.5–42.8), with a significant difference (p < 0.001) between male and female patients [35.7 (SD 3.0) vs. 32.1 (SD 2.4)]. The MELFC was 31.0 mm (range 22.9–39.0), with a significant difference (p < 0.001) between male and female patients of 32.7 (SD 3.1) vs. 29.2 (SD 2.7) (Table 1). There was a strong correlation (Fig. 3) between width of the distal femur and MEMFC (R 2 = 0.46, B = 0.32, p < 0.001) and MELFC (R 2 = 0.42, B = 0.31, p < 0.001), and we found a mean difference of 3.1 mm (p < 0.001) for the MEMFC compared with the proposed value of 30.8 mm reported in the literature for the distance from the ME to the JL. There was no difference between MELFC and the proposed value of 30.8 mm reported in the literature [mean difference 0.2 (p ∼0.69)] (Table 2 and Fig. 4).
Regression of distances in millimetres to femoral bony landmarks (ME, LE, AT), to the joint line (JL) separately for the medial and lateral compartments (MFC, LFC) to the femoral width. Additionally, values were separated for male (black dots) and female (grey dots) patients. All regressions showed significance (p<0.001). ME medial epicondyle, LE lateral epicondyle, AT adductor tubercle
Distances (mm) between the fibular head (FH), medial epicondyle (ME), lateral epicondyle (LE) and adductor tubercle (AT), respectively, within the medial (FHMFC, MEMFC, LEMFC, ATMFC) and lateral (FHLFC, MELFC, LELFC, ATLFC) compartment. Red lines show the proposed values between the landmark and the joint line (JL) that could be found in the literature (FH to JL ∼10 mm [7], ME to JL=30.8 mm [9], LE to JL=25.3 [18] and AT to JL=48.7 [10]. FHMFC distance from the femoral head to the medial femoral compartment, MEMFC distance from the medial epicondyle to the medial femoral compartment, LEMFC distance from the lateral epicondyle to the medial femoral component, ATMFC distance from the adductor tubercle to the medial femoral component
Lateral femoral epicondyle
The LEMFC was 33.4 mm (range 19.4–42.8), with a significant difference (p < 0.001) between male and female patients [35.4 (SD 3.1) vs. 31.4 (SD 3.1)]. The LELFC was 30.6 mm (range 16.6–42.6), with a significant difference (p < 0.001) between male and female patients [32.5 (SD 3.4) vs. 28.6 (SD 3.4)] (Table 1). There was a strong correlation (Fig. 3) between width of the distal femur and LEMFC (R 2 = 0.35, B = 0.31, p < 0.001) and LELFC (R 2 = 0.25, B = 0.28, p < 0.001). There is a significant difference (p < 0.001) between our measurements concerning the LEMFC and LELFC (mean 8.1 vs. 5.3) and the proposed value of 25.3 mm distance between the lateral epicondyle in literature (Table 2 and Fig. 4).
Adductor tubercle
The ATMFC was on average 45.4 mm (range 37.7–54.8), with a significant difference (p < 0.001) between male and female patients [47.9 (SD 4.1) vs. 42.8 (SD 3.0)]. The ATLFC was 42.3 mm (range 34.3–52.4), with a significant difference (p < 0.001) between male and female patients [44.8 (SD 4.1) vs. 39.8 (SD 3.3)]. (Table 1). There was a strong correlation between width of the distal femur and ATMFC (R 2 = 0.61, B = 0.49, p < 0.001) and distal femur and ATLFC (R 2 = 0.57, B = 0.48, p < 0.001). Compared with the proposed value in the literature of 48.7 mm between the AT and the JL, we found a significant difference (−3.3 mm for ATMFC and −6.4 mm for ATLFC) (Table 2 and Fig. 4).
Calculations
Regarding created regressions, distances from bony landmarks (AT, ME, LE) to the JL in both the medial and lateral compartments were calculated using the following formulas:
Mean deviations between calculated and actual values were 1.87 (SD 1.50) for MEMFC, 2.03 (SD 1.55) for MELFC, 2.18 (SD 2.00) for LEMFC, 2.41 (SD 2.32) for LELFC, 2.21 (SD 1.59) for ATMFC and 2.32 (SD 1.78) for ATLFC.
Discussion
The JL as described here refers to the articulation site between the medial and lateral femur and the proximal tibia. In anteroposterior radiographs, the JL is usually approximated by connecting the most distal point of the medial and lateral femur, with the knowledge that the condylar cartilage as the most distal condylar point is not included. As this forms a line between the medial and lateral condyles, the tibiofemoral joint it is referred to as the JL. Regarding the 3D kinematics of the knee, the decreasing curvature radius of the condyles—in which medial and lateral sizes are different—indicates anatomic differences between medial and lateral articulating sites of the proximal tibia, which have different slopes. As such, due to the complex motion of femoral rotation and translation during flexion might rather be called the joint plane. As surgical restoration of this plane is highly complex, we focussed on the proximal–distal orientation of the JL (Fig. 1).
Martin et al. [3] reported an increase in midflexion laxity when the JL was shifted 5 mm proximally and anteriorly while it was tightened when it was lowered and set 5 mm posteriorly in TKA. Several groups [5, 17] found poorer clinical and functional outcome after TKA if the JL was elevated >8 mm. These results highlight the importance of restoring the JL in TKA.
To the best of our knowledge, this is the first study to respect the natural JL (with a varus deviation) for distance measurements in the knee. We found an average deviation of the JL of ∼4° varus to an orthogonal line to the tibial mechanical axis. This is also reported in previous studies in which 87 ± 3° varus was found [11, 12]. As we excluded any knees with deviation in the femorotibial axis—a notable restriction—we did not include the full range of anatomical differences in the proximal JL. The mean absolute difference of 3.1 (range value 1.1–6.2) mm in our study between the medial and lateral compartment was calculated on the level of the most distal femoral points of the MFC and LFC. Consequently, determining absolute distances from the most medial and lateral tibial borders to the JL would have resulted in even higher values than those presented here.
In this study, MRI scans were made with different systems. However, as standardised protocols were used, measurements could be compared. We included young patients in our analysis, as cartilage becomes thinner in older patients without showing significant lesions. In comparison with the study by Servien et al. [7], whose patients had an average age of 37.9 years, the average age of our patients was 29.6 years. All patients >30 years in this study additionally had an arthroscopy, as cartilage or bone damage would have notably changed the measurements; all knees were normal in terms of cartilage condition. A limitation of our study is that the mechanical tibial and femoral axes were not determined in full-leg radiographs but in conventional MRI scans of the knees. For the tibial mechanical axis, the midpoint of the tibial spines was connected with a point determined as the centre of the tibial shaft. For the femoral mechanical axis, a line from the midpoint of the distal femur to the midpoint of the centre of the shaft was drawn. According to Issa et al. [16], this method is reliable for assessing the femorotibial angle in conventional radiographs in comparison to full-leg radiographs. As a significant limitation, our MRI scans were performed without weight bearing, which can influence the measured tibiofemoral angle, as the condition of the surrounding knee ligaments is not respected. Alternatively, measurements could have been performed in full-leg MRI, as they are for rotational investigations. However, in our attempts, due to reduced quality of those images, we found no advantage in relation to accuracy. All measurements were performed by two independent orthopaedic surgeons (GM, CB) and showed excellent interobserver correlation. In our opinion, this emphasises the good reproducibility of the femorotibial angle or the bony and cartilaginous landmarks investigated in our study.
The average distance from the FH to the JL within the medial compartment (FHMFC) was ∼12.2 mm (range 3.2–19.5) and to the JL within the lateral compartment (FHLFC) was about 15.3 mm (range 6.0–22.0). This distance was randomly determined, with no correlation to tibial width. Regarding the wide range in FHLFC measurements of 6–22 mm, setting the JL ∼10 mm above the FH, as described in the literature [7], cannot be recommended, as it would not take into consideration the original JL and may lower or raise it to a considerable extent. In previous publications, only the distance between the FH and the JL within the lateral compartment were calculated. Our results concerning the average FHLFC are roughly comparable with all those measurements [7, 14]. However, it must be considered that there is an average difference of >3 mm (range ∼ 1–6 mm) between medial and lateral compartments.
For the distal femur, the MEMFC was 33.9 mm (range 26.5–42.8) and the MELFC was 31.0 mm (range 22.9–39.0). Griffin et al. [18], in an MRI study of 104 knees, found a distance from the ME to the JL of 27.4 mm; however, they did not measure the ME but the lower-lying sulcus. Servien et al. [7] measured the sulcus, not the ME, when assessing the distance from the ME to the JL, reporting an average of 28.3 mm. In cadaver studies, Stiehl and Abott [9] found a distance from the ME to the JL of 30.8 mm, with Liu et al. [19] reporting a distance of ∼34.0 mm. The reason for these diverging results might be found in the underlying anatomy of the ME, which consists of a ridge surrounding a central sulcus with a mean diameter of 11.4 mm [18]. Some authors measured the sulcus, whereas others tried to measure the prominent epicondyle, which forms a curved ridge rather than a peak.
The LEMFC was 33.4 mm (range 19.4–42.8) and the LELFC 30.6 mm (range 16.6–42.6). Griffin et al. found a distance of 24.3 mm [18], Serien et al. of 23.0 mm [7] and Stiehl and Abott of 25.3 mm [9]. The different results reported by Serien et al. and Griffin et al. might be attributable to the differences in their measuring technique: First they always measured the most distal point of the LE, whereas we looked for the most prominent aspect of the LE in the axial slices and the midpoint of the insertion of the lateral ligament. Second they measured orthogonal to a tangent of the most distal point of the ME and LE; we measured orthogonal to the mechanical axis of the femur. However, the excellent interobserver correlation between the two observers in our study indicates that there is a certain range of interpretation for the exact location of the LEs.
The average distance from the AT to the most distal point of the MFC (ATMFC) was 45.4 mm, with a wide range of 37.7–54.8. The average ATLFC was 42.3 mm (range 34.3–52.4); we found no comparable MRI study for this measurement. Iacono et al. [10] investigated 110 standard knee radiographs, measuring the distance from the AT to the most distal bony border of the medial femoral condyle, reporting an average of 48.7 mm, which, unexpectedly, is more than in our measurements. As they did not respect the additional cartilage when measuring to the bony distal femoral condyle, we would expect a shorter average distance from the AT to the JL in their measurements in comparison with our results. However, their results were not based on exact specification of X-ray scaling. Keeping in mind the usual magnification error of X-rays of ∼10 %, this would result in a mean distance of 43.9 mm in ATMFC. The difference can be explained by the fact that they did not measure the cartilage.
We also investigated ratios between femoral and tibial width and distances of the ME and LE, FH and the AT to the JL separately for medial and lateral compartments. There was no significant correlation between tibial width and FHMFC (p = 0.21) or FHLFC (p = 0.23). This indicates there is no relationship between fibular position and the femorotibial joint.
In contrast, we found a strong correlation between distal femoral width and MEMFC (R 2 = 0.46, B = 0.32, p < 0.001), MELFC (R 2 = 0.42, B = 0.31, p < 0.001), LEMFC (R 2 = 0.25, B = 0.31, p < 0.001) and LELFC (R 2 = 0.25, B = 0.28, p < 0.001). The best correlation was found between distal femoral width and ATMFC (R 2 = 0.61, B = 0.49, p < 0.001) as well as the ATLFC (R 2 = 0.57, B = 0.48, p < 0.001). Iacono et al. [10] also investigated the ratios between femoral width and bony landmarks, reporting an excellent correlation for the AT (r = 0.83) and femoral width similar to our results (ATMFC R 2 = 0.61). However, they had a far lower correlation coefficient (r = 0.52) for the ME than we had (MEMFC R 2 = 0.46). The reason for this could be the difficulty detecting the ME in conventional X-rays, as it is superimposed by surrounding bony structures. Those authors stated that the JL is best estimated by calculating the ratio to the femoral width using the following formula: distance from the AT to the JL = 0.543 × femoral width. The average difference between the measured and estimated distance from the AT to the JL was ±2.7 mm. However, as noted above, it is not clear whether or not they used scaled X-rays. If not, the calculation should be used with care.
Conclusion
Restoring the JL improves clinical and functional outcome in TKA [3, 5, 17] and should therefore be aspired to. In primary TKA, when classic resection of the proximal tibia and distal femur 90° to the mechanical axis is performed, the JL is mandatorily changed. We found a varus JL deviation of 4.2° in relation to the orthogonal line to the mechanical tibial axis. In classic varus knees, therefore, the JL is usually medially preserved and laterally lowered due to lateral femoral underresection and tibial overresection. In contrast, when anatomical resection is performed, the JL can be theoretically restored. However, when using stems in primary or revision TKA, the classic resection technique is necessary because of implant restrictions. In revision surgery, when the original JL should be estimated by the residual structures in the knee, according to our data, no bony structure is reliable.
Distances in the FH, ME and LE or AT to the JL show a wide variance. Hence, adding 10 mm to the FH or reducing ∼30 mm to the ME or ∼25 mm to the LE or 49 mm to the AT should be avoided, as this can mislead a surgeon and significantly change the JL.
According to our data, the best way to estimate the JL is to calculate it via the femoral width using the following formula: distance ATMFC = 6.40 + (width femur [mm] × 0.49). Using a calliper, the calculated distance can be measured from the AT to the medial compartment. The average difference between the measured and estimated distance from the AT to the JL is ±2.2 mm. Alternatively, the JL can be estimated using formulas for ATLFC, MEMFC, MELFC, LEMFC and LELFC.
References
Singerman R, Davy DT, Goldberg VM (1994) Effects of patella alta and patella infera on patellofemoral forces. J Biomech 27:1059
Singerman R, Heiple KG, Davy DT et al (1995) Effect of tibial component position on patellar strain following total knee arthroplasty. J Arthroplasty 10:651
Martin JW, Whiteside LA (1990) The influence of joint line position on knee stability after condylar knee arthroplasty. Clin Orthop 259:146
Laskin RS (2002) Joint line position restoration during revision total knee replacement. Clin Orthop Relat Res 404:169–171
Figgie HE III, Goldberg VM, Heiple KG, Moller HS III, Gordon NH (1986) The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am 68:1035–1040
Partington PF, Sawhney J, Rorabeck CH et al (1999) Joint line restoration after revision total knee arthroplasty. Clin Orthop 367:165
Servien E, Viskontas D, Giuffre BM, Coolican MRJ, Parker DA (2008) Reliability of bony landmarks for restoration of the joint line in revision knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 16:263–269
Jawhar A, Wasnik S, Scharf HP, Roehl H (2013) Fibula head is a useful landmark to predict the location of posterior cruciate ligament footprint prior to total knee arthroplasty. Int Orthop [Epub ahead of print]
Stiehl JB, Abott BD (1995) Morphology of the transepicondylar axis and its application in primary and revision total knee arthroplasty. J Artroplasty 10:185–189
Iacono F, Lo Presti M, Bruni D, Raspugli GF, Bignozzi S, Sharma B, Marcacci M (2013) The adductor tubercle: a reliable landmark for analysing the level of the femorotibial joint line. Knee Surg Sports Traumatol Arthrosc 21(12):2725–2729
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surgery Am 69(5):745–749
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? the concept of constitutional varus. Clin Orthop Relat Res 470(1):45–53
Jawhar A, Shah V, Sohoni S, Scharf HP (2013) Joint line changes after primary total knee arthroplasty: navigated versus non-navigated. Knee Surg Sports Traumatol Arthrosc 21:2355–2362
Havet E, Gabrion A, Leiber-Wackenheim F, Vernois J, Olory B, Mertl P (2007) Radiological study of the knee joint line position measured from the fibular head and proximal tibial landmarks. Surg Radiol Anat 29(4):285–289
Lee HJ, Lee JS, Jung HJ, Song KS, Yang JJ, Park CW (2011) Comparison of joint line position changes after primary bilateral total knee arthroplasty performed using the navigation-assisted measured gap resection or gap balancing techniques. Knee Surg Sports Traumatol Arthrosc 19(12):2027–2032
Issa SN, Dunlop D, Chang A, Song J, Prasad PV, Guermazi A, Peterfy C, Cahue S, Marshall M, Kapoor D, Hayes K, Sharma L (2007) Full-limb and knee radiography assessments of varus-valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis Rheum 57(3):398–406
Partington PF, Sawhney J, Rorabeck CH et al (1999) Joint line restoration after revision total knee arthroplasty. Clin Orthop 367:165–171
Griffin FM, Math K, Scuderi GR, Insall JN, Poilvache PL (2000) Anatomy of the epicondyles of the distal femur: MRI analysis of normal knees. J Arthroplasty 15:354–359
Liu F, Yue B, Gadikota HR, Kozanek M, Liu W, Gill T, Rubish HE, Li G (2010) Morphology of the medial collateral ligament of the knee. J Orthop Surg Res 5:69
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maderbacher, G., Keshmiri, A., Schaumburger, J. et al. Accuracy of bony landmarks for restoring the natural joint line in revision knee surgery: an MRI study. International Orthopaedics (SICOT) 38, 1173–1181 (2014). https://doi.org/10.1007/s00264-014-2292-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-014-2292-3