Abstract
Purpose
Locked plate (LP) and retrograde intramedullary nail (RIN) are the most commonly used treatment options for periprosthetic femur fracture above total knee arthroplasty (TKA). Controversy still exists regarding which is better. Therefore we performed a meta-analysis to compare their clinical results.
Methods
A comprehensive search was conducted through PubMed, EMBase and the Cochrane Collaboration Library. Six comparative studies (265 patients) were included for the meta-analysis.
Results
No statistically significant differences were found between the LP group and RIN group in terms of six month union rate (OR, 1.19; 95 % CI, 0.52–2.69; P = 0.68), union time (WMD, 0.22; 95 % CI, −0.41 to 0.84; P = 0.50), operation time (WMD, 0.54; 95 % CI, −13.09 to 14.17; P = 0.94) or complication rate (OR, 0.79; 95 % CI, 0.22–2.91; P = 0.73). The LP fixation may have a relatively higher re-operation rate (OR, 5.17; 95 % CI, 1.02–26.27; P = 0.05) compared with RIN. The mean union time was 4.0 months in the LP group and 3.7 months in the RIN group.
Conclusion
This meta-analysis found no statistically significant difference in six month union rate, union time, operation time and complication rate between the LP group and RIN group. The RIN fixation may have a potential of lower re-operation rate compared with LP. The mean union time was 4.0 months in the LP group and 3.7 months in the RIN group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periprosthetic femur fracture above total knee arthroplasty (TKA) is a challenge for orthopaedic surgeons due to osteoporosis, limited bone available for fixation and the existence of a femoral component. The reported incidence of distal periprosthetic femur fractures above TKA was 0.3–5.5 % [1–3], and it is expected to be more common in an aging population.
In the management of periprosthetic femur fractures with stable prosthesis, previous studies have well demonstrated that non-operative treatment and traditional (non-locked) plate methods could not be satisfactory for relative high nonunion, complication and re-operation rates [4–7]. Modern treatment options including retrograde intramedullary nail and locked plate are significantly superior to conventional treatment methods, since they can provide better stability of fracture and protection of the blood supply [5]. While controversy over the optimal fixation strategy still exists in the orthopaedic community and literature. So we performed this meta-analysis to compare the superiority of these two implants for periprosthetic femur fractures above TKA.
Materials and methods
Search methods for identification of studies
A comprehensive search of all relevant randomized controlled trials (RCTs) and comparative studies was conducted through PubMed, EMBase and the Cochrane Collaboration Library, up to May 2015, with no language restriction. Key words used for search strategy included: total knee arthroplasty, femur fracture, locked plate, LISS, intramedullary nail, randomized controlled study and comparative study. Manual search of possibly related references were also conducted. Two investigators independently reviewed the titles, abstracts and full texts of all potentially relevant studies as recommended by the Cochrane Collaboration.
Study eligibility criteria
Studies were selected on the basis of the following criteria: (1) study design: randomized controlled trails or non-randomized comparative studies; (2) study population: patients with distal periprosthetic femur fractures above TKA of the ipsilateral limb; (3) intervention: including both locked plate (or Less Invasive Stabilization System [LISS]) and retrograde intramedullary nail; (4) follow-up time: six months at least; (5) outcome measurements: union rate, re-operation rate, surgical complications, operation time and union time. Studies were excluded if they failed to meet the above criteria.
Data extraction and methodological quality assessment
The following data were extracted from the included articles: authors, publication date, study design, participant characteristics, specific interventions and outcome measurements. Unreported data that are needed for this meta-analysis were obtained by communication with the first authors or corresponding authors though e-mail. The quality of included studies was assessed with the Newcastle-Ottawa scale.
Data analysis
This meta-analysis was performed with Review Manager software (RevMan 5.3) and the level of significance was set at P < 0.05. For dichotomous outcomes, odds ratio (OR) and 95 % confidence interval (CI) were calculated. For continuous outcomes, weighted mean difference (WMD) and 95 % CI were calculated. The size of heterogeneity across studies was estimated with I2 statistic and the chi-squared test. A P > 0.1 and an I 2 ≤ 50 % were considered of no statistical heterogeneity. Random effect model or fixed effect model were adopted depending on the heterogeneity of the included studies.
Results
Search results
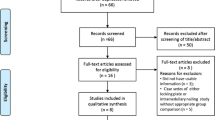
The initial search identified 670 references from the selected databases. Six hundred fifty-seven references were excluded by screening the abstracts and titles for duplicates, unrelated articles, case reports, systematic reviews and non-comparative studies. The remaining 13 studies underwent full text review. A further seven articles [5, 8–13] were excluded. The details of identifying relevant studies are shown in the flow chart of study selection process (Fig. 1). Six comparative studies (five English articles [14–18] and one German article [19]) including 265 patients (153 from LP group, 112 from RIN group) were finally selected for this meta-analysis.
Risk bias
Since no RCTs were reported on this issue, all of the six included studies were comparative studies. The characteristics of these included studies are summarized in Table 1. The Newcastle-Ottawa scale was used to assess the quality of the selected studies. All of the included studies scored 7–8 points, indicating relatively high quality (Table 2).
Meta-analysis results
Union rate
Two included studies [18, 19] failed to define the assessment time and criteria of fracture union. The other four studies [14–17] (n = 203 patients; 112 from LP group and 91 from RIN group) reported a union rate six months after operation by clinical and radiographic evaluation. So we just pooled these four studies in the meta-analysis. The incidence of fracture union was 87.5 % (98/112) in the LP group and 83.5 % (76/91) in the RIN group. The was no statistically significant difference in six month union rate between the LP group and RIN group (OR, 1.19; 95 % CI, 0.52–2.69; P = 0.68; fixed effect model) with low heterogeneity (P = 0.20; I 2 = 38 %) (Fig. 2). In these four studies, Kilucoglu et al. [14], Aldrian et al. [15] and Hou et al. [17] assessed the union rate at 6 months after surgery, while Horneff et al. [16] did so at 24 weeks. So a sensitivity analysis was conducted to further eliminate the heterogeneity by excluding Horneff et al.’s study [16]. No significant difference was found either (OR, 0.55; 95 % CI, 0.16–1.86; P = 0.34; fixed effect model) with no heterogeneity (P = 0.94; I 2 = 0 %) (Fig. 3), which was in line with our previous analysis. In these studies some patients diagnosed as nonunion at six months underwent revision surgeries. While others received conservative treatment. So the union rate of longer time observation could not be effectively assessed.
Union time
Time of union was reported in two studies [14, 17] (n = 52 patients; 33 from LP group and 19 from RIN group). The mean union time was 4.0 months in the LP group and 3.7 months in the RIN group. No statistically significant difference was detected between the two groups (WMD, 0.22; 95 % CI, −0.41 to 0.84; P = 0.50; fixed effect model) with no heterogeneity (P = 0.74; I 2 = 0 %).
Operation time
Operation time obtained in three studies [16, 17, 19] with a total of 133 patients (71 in the LP group and 62 in the RIN group) was analyzed. There was no statistically significant difference in operation time between the LP group and RIN group (WMD, 0.54; 95 % CI, −13.09 to 14.17; P = 0.94; fixed effect model) with no heterogeneity (P = 0.39; I 2 = 0 %).
Complications
The complication rate (including malunion, nonunion, infection, revision, fixation failure) reported in four studies [15, 17–19] with a total of 177 patients (110 in the LP group and 67 in the RIN group) was analyzed. There was no statistically significant difference in complication rate between the LP and RIN groups (OR, 0.79; 95 % CI, 0.22–2.91; P = 0.73; random effect model) with moderate heterogeneity (P = 0.10; I 2 = 52 %). A sensitivity analysis was conducted to further eliminate the heterogeneity by excluding Large et al.’s study [18], in which all seven patients (100 %) in the RIN group developed a malunion or nonunion. No significant difference was found either (OR, 1.37; 95 % CI, 0.57–3.30; P = 0.48; fixed effect model) with no heterogeneity (P = 0.92; I 2 = 0 %), which was consistent with our previous analysis.
Re-operation rate
The re-operation rate obtained in four studies [14–16, 19] with a total of 178 patients (93 in the LP group and 85 in the RIN group) was analyzed. The re-operation reasons included infection, nonunion, fixation failure, prosthesis loosening and refracture. The re-operation rate was not significantly different between the LP group and the RIN group (OR, 1.54; 95 % CI, 0.16–15.07; P = 0.71; random effect model) with high heterogeneity (P = 0.02; I 2 = 76 %) (Fig. 4). A sensitivity analysis was conducted to eliminate the heterogeneity by excluding one study [16], which showed a 40 % re-operation rate in the RIN group, obviously high than most other studies. The re-operation rate in the RIN group was nearly significantly lower than the LP group (OR, 5.17; 95 % CI, 1.02–26.27; P = 0.05; fixed effect model) with no heterogeneity (P = 0.81; I 2 = 0 %) (Fig. 5).
Discussion
With the improvement of surgical technique and prosthetic design, the number of TKA conducted every year is gradually increased. While periprosthetic femur fracture above TKA is also expected to be more common due to the aging population and increase of activity. The treatment of this complex fracture is still a tough challenging one for orthopaedic surgeons with relatively high complication and mortality rates [20–22]. Streubel et al. [21] conducted a study of 92 consecutive patients over 60 years with low-energy supracondylar femur fractures. The six month mortality rates of patients with periprosthetic femur fractures were significantly higher than those with non-periprosthetic supracondylar femur fractures (24 vs 13 %). Therefore, the research on treatment of this complicated fracture is essential.
A previous systematic review of 415 patients with periprosthetic femur fractures after TKA was conducted by Herrera et al. [5]. They compared the results of traditional treatment methods and modern treatment options. Their results showed RIN and LP fixation were superior to traditional treatment methods (non-operative treatment and non-locked plate fixation), which was widely accepted in the management of periprosthetic femur fractures after TKA [2, 23, 24]. But the comparison between LP and RIN groups was not performed, due to a relatively small number of patients treated with these two methods. Also no randomized controlled trials or non-randomized comparative studies were included. Since the incidence of periprosthetic femur fracture above TKA is relatively low and the application of these two treatment methods is relatively late, there are only several studies (no RCTs) focused on the comparison of these two methods. Several trials [9, 12] showed RIN could provide better stability and had lower failure rate. Nevertheless, some other surgeons [16, 18] preferred LP fixation. A consensus still could not be obtained. So we performed this meta-analysis to clarify whether there was any clinical difference between these two treatment options.
RIN is popular for its advantages of reserving fracture region unexposed and avoiding extensive soft tissue dissection. In some small-sized non-comparative cohort studies, Chettiar et al. [25] and Han et al. [26] reported a 100 % union rate in RIN fixation of periprosthetic supracondylar femur fractures. Bong et al. [12] compared the LISS and RIN for fixation of periprosthetic supracondylar femur fracture proximal to a TKA and reported that RIN could provide greater stability than LISS. But this research was performed on human cadaver femurs. Meneghini et al. [9] reported that although significant more screws were used for fixation of distal fragment, the failure rate of the locked plate system was twice that of intramedullary nail fixation. Their study was not included in the present analysis for a relatively short follow-up time (<6 months). In this meta-analysis, the LP group may have a relatively higher re-operation rate than RIN group (OR, 5.17; 95 % CI, 1.02–26.27; P = 0.05; fixed effect model) with no heterogeneity (P = 0.81; I 2 = 0 %) (Fig. 5), after excluding Horneff at al.’s study [16], which showed a 40 % re-operation rate in the RIN group, obviously higher than most other studies. Also, they reported a significantly longer operation time in the LP group compared with the RIN group (155.3 min vs 113.0 min; P < 0.01; SD = 129.3). The data of Horneff et al.’s study [16] was compiled from three different institutions and eight different surgeons; this might partly explain why some of their results were significantly different from other studies and why the standard deviation was too large (SD = 129.3). While in our analysis no statistically significant difference was found in the operation time between the LP group and RIN group (WMD, 0.54; 95 % CI, −13.09 to 14.17; P = 0.94). This was in agreement with most other included studies [17, 19].
With the introduction of minimally invasive technique and LISS, the LP system has become an ideal option for the treatment of periprosthetic femur fracture after TKA. It has the advantages of providing better fixation in osteoporotic patients and keeping blood supply largely intact. In the study of Kolb et al. [23], 23 consecutive periprosthetic femur fracture patients with a well-fixed femoral component were treated with LISS and all cases got union. However, their study had a small cohort size and was non-comparative, which could not delineate a superior fixation option from LP and RIN. LISS has overcome the disadvantage, requiring an open box femoral component and a relatively large distal fragment of retrograde intramedullary nail. And as Wick et al. [19] noted, LISS was superior to RIN in the management of periprosthetic femur fractures with a small distal fragment, which was also supported by most authors of the included studies [15–17]. Several classification systems [20, 27–30] were used to describe the periprosthetic femur fractures above TKA in the included studies. The Lewis and Rorabeck classification [27] was used in three studies [16, 18, 19]. All the fractures in their studies were Lewis and Rorabeck type II: displaced fractures with a stable prosthesis. The others adopted the Neer classification [29] (Kilucoglu et al. [14]: type 2 in 11 patients, type 4 in two patients and type 3 in one patient), the classification system of Su et al. [20] (Aldrian et al. [15]: 32 patients with a Su type I fracture [proximal to the femoral prosthetic component], and 54 patients with a Su type II fracture [originating at the anterior flange of the femoral prosthetic component]) and the Orthopaedic Trauma Association (OTA) classification [30] (Hou et al. [17]: 39 33A-type fractures, 3 32B-type fractures, and 10 32A-type fractures), respectively.
In the study of Large et al., all seven patients in the RIN group (three short nails and four long nails) developed a malunion or nonunion, compared with 20 % (5/25) malunion rate and 0 % nonunion rate in the LP group. In their retrospective study from 1995 to 2005, only seven patients underwent RIN fixation (three short nails and four long nails). Poor clinical results in the RIN group might be related to the lack of experience in nail surgery. In the presented study, no significant difference was found in six month union rate, union time and complication rate between these two groups before and after sensitivity analysis. This was consistent with the studies of Hou et al. [17] and Kilucoglu et al. [14]. The mean union time was 4.0 months in the LP group and 3.7 months in the RIN group.
There is the first meta-analysis that directly compared clinical results of LP and RIN for periprosthetic femur fractures above TKA. But there are also some limitations of this study. Since no randomized controlled trails or prospective studies were reported on this topic, all the included studies are comparative studies. The results must be interpreted with caution due to the natural defects of retrospective studies. And the number of included studies is relatively small. Large sample multi-centre randomized controlled trials are required in the future to verify the results of this meta-analysis.
Conclusions
In conclusion, this meta-analysis found no statistically significant difference in six month union rate, union time, operation time and complication rate between LP group and RIN group. The RIN fixation may have a potential of lower re-operation rate compared to LP. The mean union time was 4.0 months in the LP group and 3.7 months in the RIN group.
References
Dennis DA (2001) Periprosthetic fractures following total knee arthroplasty. Instr Course Lect 50:379
Bezwada HP, Neubauer P, Baker J, Israelite CL, Johanson NA (2004) Periprosthetic supracondylar femur fractures following total knee arthroplasty. J Arthroplast 19(4):453
Rorabeck CH, Taylor JW (1999) Periprosthetic fractures of the femur complicating total knee arthroplasty. Orthop Clin North Am 30(2):265
Sisto DJ, Lachiewicz PF, Insall JN (1985) Treatment of supracondylar fractures following prosthetic arthroplasty of the knee. Clin Orthop Relat Res (196):265
Herrera DA, Kregor PJ, Cole PA, Levy BA, Jonsson A, Zlowodzki M (2008) Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981–2006). Acta Orthop 79(1):22
Merkel KD, Johnson EW Jr (1986) Supracondylar fracture of the femur after total knee arthroplasty. J Bone Joint Surg Am 68(1):29
Moran MC, Brick GW, Sledge CB, Dysart SH, Chien EP (1996) Supracondylar femoral fracture following total knee arthroplasty. Clin Orthop Relat Res 324:196
Althausen PL, Lee MA, Finkemeier CG, Meehan JP, Rodrigo JJ (2003) Operative stabilization of supracondylar femur fractures above total knee arthroplasty: a comparison of four treatment methods. J Arthroplast 18(7):834
Meneghini RM, Keyes BJ, Reddy KK, Maar DC (2014) Modern retrograde intramedullary nails versus periarticular locked plates for supracondylar femur fractures after total knee arthroplasty. J Arthroplast 29(7):1478
Kancherla VK, Nwachuku CO (2014) The treatment of periprosthetic femur fractures after total knee arthroplasty. Orthop Clin North Am 45(4):457
Platzer P, Schuster R, Aldrian S, Prosquill S, Krumboeck A, Zehetgruber I, Kovar F, Schwameis K, Vecsei V (2010) Management and outcome of periprosthetic fractures after total knee arthroplasty. J Trauma 68(6):1464
Bong MR, Egol KA, Koval KJ, Kummer FJ, Su ET, Iesaka K, Bayer J, Di Cesare PE (2002) Comparison of the LISS and a retrograde-inserted supracondylar intramedullary nail for fixation of a periprosthetic distal femur fracture proximal to a total knee arthroplasty. J Arthroplast 17(7):876
Makinen TJ, Dhotar HS, Fichman SG, Gunton MJ, Woodside M, Safir O, Backstein D, Willett TL, Kuzyk PR (2015) Periprosthetic supracondylar femoral fractures following knee arthroplasty: a biomechanical comparison of four methods of fixation. Int Orthop
Kilucoglu OI, Akgul T, Saglam Y, Yazicioglu O (2013) Comparison of locked plating and intramedullary nailing for periprosthetic supracondylar femur fractures after knee arthroplasty. Acta Orthop Belg 79(4):417
Aldrian S, Schuster R, Haas N, Erhart J, Strickner M, Blutsch B, Wernhart S, Leitgeb J, Platzer P (2013) Fixation of supracondylar femoral fractures following total knee arthroplasty: is there any difference comparing angular stable plate fixation versus rigid interlocking nail fixation? Arch Orthop Trauma Surg 133(7):921
Horneff JG 3rd, Scolaro JA, Jafari SM, Mirza A, Parvizi J, Mehta S (2013) Intramedullary nailing versus locked plate for treating supracondylar periprosthetic femur fractures. Orthopedics 36(5), e561
Hou Z, Bowen TR, Irgit K, Strohecker K, Matzko ME, Widmaier J, Smith WR (2012) Locked plating of periprosthetic femur fractures above total knee arthroplasty. J Orthop Trauma 26(7):427
Large TM, Kellam JF, Bosse MJ, Sims SH, Althausen P, Masonis JL (2008) Locked plating of supracondylar periprosthetic femur fractures. J Arthroplast 23(6 Suppl 1):115
Wick M, Muller EJ, Kutscha-Lissberg F, Hopf F, Muhr G (2004) Periprosthetic supracondylar femoral fractures: LISS or retrograde intramedullary nailing? Problems with the use of minimally invasive technique. Unfallchirurg 107(3):181
Su ET, DeWal H, Di Cesare PE (2004) Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg 12(1):12
Streubel PN, Ricci WM, Wong A, Gardner MJ (2011) Mortality after distal femur fractures in elderly patients. Clin Orthop Relat Res 469(4):1188
Bhattacharyya T, Chang D, Meigs JB, Estok DM 2nd, Malchau H (2007) Mortality after periprosthetic fracture of the femur. J Bone Joint Surg Am 89(12):2658
Kolb W, Guhlmann H, Windisch C, Marx F, Koller H, Kolb K (2010) Fixation of periprosthetic femur fractures above total knee arthroplasty with the less invasive stabilization system: a midterm follow-up study. J Trauma 69(3):670
Nauth A, Ristevski B, Begue T, Schemitsch EH (2011) Periprosthetic distal femur fractures: current concepts. J Orthop Trauma 25(Suppl 2):S82
Chettiar K, Jackson MP, Brewin J, Dass D, Butler-Manuel PA (2009) Supracondylar periprosthetic femoral fractures following total knee arthroplasty: treatment with a retrograde intramedullary nail. Int Orthop 33(4):981
Han HS, Oh KW, Kang SB (2009) Retrograde intramedullary nailing for periprosthetic supracondylar fractures of the femur after total knee arthroplasty. Clin Orthop Surg 1(4):201
Rorabeck CH, Angliss RD, Lewis PL (1998) Fractures of the femur, tibia, and patella after total knee arthroplasty: decision making and principles of management. Instr Course Lect 47:449
Rorabeck CH, Taylor JW (1999) Classification of periprosthetic fractures complicating total knee arthroplasty. Orthop Clin North Am 30(2):209
Neer CS 2nd, Grantham SA, Shelton ML (1967) Supracondylar fracture of the adult femur. A study of one hundred and ten cases. J Bone Joint Surg Am 49(4):591
Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audige L (2007) Fracture and dislocation classification compendium—2007: orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma 21(10 Suppl):S1
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Li, B., Gao, P., Qiu, G. et al. Locked plate versus retrograde intramedullary nail for periprosthetic femur fractures above total knee arthroplasty: a meta-analysis. International Orthopaedics (SICOT) 40, 1689–1695 (2016). https://doi.org/10.1007/s00264-015-2962-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2962-9