Abstract
Purpose
The aim of our study was to evaluate the effect of the S3 (spatial subchondral support) humeral plate and to compare the clinical outcomes and complications after ORIF (open reduction and internal fixation) of proximal humeral fractures using either a S3 plate or a PHLP (proximal humeral locking plate).
Methods
A total of 144 patients with displaced unstable proximal humeral fractures were treated with either a S3 plate or a PHLP. Each patient had a follow-up at least for one year. We retrospectively collected the data and compared the shoulder functional outcome as well as complications of these two methods.
Results
During the one-year follow-up, the average Constant scores gradually improved for both groups. Patients treated with use of an S3 plate had better functional results at three and six months (P < 0.05). The one-year Constant score for all fracture types (Neer classified) were not significantly different between the S3 and PHLP group (P > 0.05). The complication rate was comparable between the two groups (P > 0.05).
Conclusions
The treatment using an S3 plate for displaced unstable proximal humeral fractures resulted in a good union rate and functional outcome, which is comparable to the PHLP treatment. The S3 humerus plate can be considered as an effective implant for ORIF of displaced unstable proximal humeral fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal humeral fractures are one of the most common fractures in the elderly population and account for 5 % of all fractures [1, 2]. As there is an increasing proportion of elderly people in the population [3], proximal humeral fractures present an increasing challenge to doctors. An epidemiology study has estimated that the number of patients with these fractures may be tripled by the year 2030 [4]. Thus, searching for an effective treatment for proximal humeral fractures is of great importance. The majority of these fractures are undisplaced or minimally displaced, which can be managed conservatively successfully [5]. As for the displaced unstable proximal humeral fractures, especially three- or four-part proximal humeral fractures, an operative treatment is necessary for achieving early functional recovery of the injured shoulder [6, 7]. However, selection of surgical devices and techniques remains controversial, and no method has been proved as the “gold standard” [8–10]. Quite a few studies had reported a variety of surgical devices and techniques including plate fixation, intramedullary nailing, hemiarthroplasty, reverse shoulder arthroplasty and so on, each of which has its advantages as well as its disadvantages [1, 7–9].
In recent years open reduction and locking plate fixation has gradually become the most commonly used method of surgical treatment for proximal humeral fractures [7, 8]. Throughout the literature, it provides anatomic reduction and stable fixation and results in a satisfactory functional outcome [9]. Meanwhile, clinically relevant complications including screw penetration, screw cutout, loss of reduction, avascular necrosis, and subacromial impingement have been frequently observed during follow-up, particularly in the presence of osteoporosis [1, 2, 5, 8, 9]. A complication rate of 34 % within one year postoperative has been observed based on a prospective, multicentre study [10]. In order to reduce the incidence of complications and improve the clinical efficacy some studies focused on a new plate design, namely, the S3 (spatial subchondral support) plate [2, 6, 11, 12]. The S3 plate is designed to be positioned 3 cm distal to the greater tuberosity; therefore subacromial impingement may be prevented theoretically [2]. Even so, the clinical evidence is insufficient to judge whether the S3 plate is a better choice for proximal humeral fractures.
The aim of our study was to evaluate the effect of the S3 humeral plate (DePuy, USA) and to compare the clinical outcomes after open reduction and internal fixation of proximal humeral fractures using either a S3 plate or a proximal humeral locking plate (Fig. 1).
Materials and methods
Study population
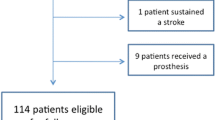
This was a retrospective case–control study which had been approved by our institutional review board. Between January 2010 and December 2013, 176 patients with displaced unstable proximal humeral fractures were treated with open reduction and internal fixation (ORIF) according to Neer criteria [13] in our hospital (a Level 1 trauma centre). All the patients included were aged at least 18 years of age and had provided informed consent prior to enrollment. Our exclusion criteria included pathological fracture or refracture, old fracture, open fracture, multiple fracture, concomitant plexus and/or nerve injuries. We also excluded patients with existing systemic disease having a relevant effect on fracture healing such as severe cardio-cerebral vascular diseases, paraplegia, multiple sclerosis, and relevant neurological disorders. Besides, patients were excluded if they were lost to follow-up. After these exclusions, a total of 144 patients with an equal number of fractures were included in this study and were divided into two groups according to the surgical methods. Of those, 75 patients were treated with ORIF with use of an S3 plate, while 69 used a proximal humeral locking plate (PHLP). All fractures were classified according to the Neer [13] classification. There were ten (13 %) two-part, 47 (63 %) three-part and 18 (24 %) four-part fractures in the S3 group, while in the PHLP group there were 17 (25 %), 32 (46 %) and 20 (29 %), respectively. The patient demographics and the characteristics of fractures are summarized in Table 1.
Surgical technique
All of the surgeries were performed under general anaesthesia. In both the S3 and PHLP groups, the patients were positioned in the supine or beach-chair position on a radiolucent operating table. In the S3 group, open reduction and internal fixation was performed using a deltopectoral or deltoid-splitting approach. The proximal humerus was exposed through a 12–14 cm incision. Fractures were reduced through traction and manipulation and then provisionally stabilized with use of Kirschner wires. After the fracture reduction had been confirmed under fluoroscopic imaging, a S3 humeral plate (DePuy, USA) was positioned approximately 3.0 cm distal to the greater tuberosity and just posterior to the bicipital groove. A 2.0-mm guide wire was placed through the central hole at the head of the plate which should be advanced slowly under fluoroscopic imaging until it reached within 2–3 mm of the subchondral bone. Using a 4-mm drill bit, it was then drilled and advanced through the F.A.S.T. Guide about 2–3 mm below the subchondral bone. The proximal plate pegs were placed into the humeral head through the peg holes and checked with fluoroscopy. The plate was then fixed to the humeral shaft using cortical screws. Tuberosity fractures were secured to the suture wire holes in the plate with use of non-absorbable sutures. A final fluoroscopy check was performed to assess the reduction and to verify correct screw placement. In the PHLP group, all of the patients were treated with a proximal humeral locking plate (General Care International, USA or Smith & Nephew, USA) which was placed proximally below the apex of the greater tuberosity to maintain reduction. The operative procedure for proximal humeral locking plate has been described in the literature [1, 7, 8, 10, 14, 15]. All patients were immobilized in a sling for four to six weeks postoperatively. Passive exercises were started within three days after surgery, while active range of motion exercises were started four weeks postoperatively.
Follow-up and clinical evaluations
All of the patients included in our study had a follow-up at least for one year. The mean follow-up was 17 months, ranging from 12 to 26 months. Follow-up evaluations of clinical outcome and complications were performed at 1.5, 3, 6, and 12 months after surgery. X-rays were taken in anteroposterior and lateral views at each time point to evaluate fracture healing, the placement of the plate and screws, and to assess the reduction. Shoulder function was assessed with use of the Constant score [16] at each follow-up. We retrospectively reviewed all radiographs and medical records to compare clinical outcomes, shoulder function and complications (e.g., avascular necrosis, screw perforations, loss of reduction, wound infection and subacromial impingement).
Statistical analysis
Data were collected independently by two reviewers, and then were entered into the SPSS software (version 18.0, statistical software for Windows, USA) for further analysis. We used a chi-square test for categorical variables (e.g., gender, classification of fracture and complications). An independent sample t-test was used for normally distributed continuous variables (e.g., age, operative time, blood loss, hospital stay and follow-up). For variables that were not normally distributed, the Mann–Whitney rank sum test was used. A P value less than 0.05 was regarded as statistically significant in this study.
Results
All the fractures in both groups achieved clinical union after one-year follow up. The average duration between injury and surgery was 2.2 (SD 2.0) days in the S3 group and 1.9 (SD 1.6) days in the PHLP group. The mean operative time was 97.4 (SD 24.5) minutes in the S3 group, while in the PHLP group it was 93.5 (SD 21.2) minutes without a significant difference. In addition, there was no significant difference in the blood loss for patients treated with either S3 or PHLP (Table 2).
During the one-year follow-up, the average Constant score improved for all groups (Fig. 2). The S3 group achieved a higher Constant score only at the three- and six-months follow-up time points compared to the PHLP group (P < 0.05). Patients in the S3 group experienced significantly less pain and better activities of daily living at the 1.5, three and six months follow-up time points compared to the patients in the PHLP group (p < 0.05). In addition, S3-treated patients had better range of motion at the three-month and six-month visit (p < 0.05). There was no significant difference in the level of strength between the two groups at all follow-up visits. At the final follow-up, the Constant scores were not significantly different in all items between the S3 group and the PHLP group (Table 3).
At the one-year follow-up, two-part fractures achieved the highest average Constant score in both groups (S3: 81.9 ± 7.5, PHLP: 77.4 ± 9.0), followed by three-part fractures (S3: 77.8 ± 9.5, PHLP: 77.2 ± 9.3), and four-part fractures had the lowest score (S3: 74.7 ± 12.0, PHLP: 76.2 ± 11.3). The one-year Constant score for all fracture types were not significantly different between the S3 and PHLP groups (Table 4, Fig. 3).
A total of 20 (26.7 %) complications were encountered throughout the one-year follow-up in the S3 group, while in the PHLP group there were 21 (30.4 %) and no significant difference was found between these two groups. The most common complication in the S3 group was displacement of the greater tuberosity (n = 5, 6.7 %). As to the PHLP group, loss of reduction leading to a varus deformity (n = 6, 8.7 %) was the most common complication. There were three (4 %) primary screw perforations and two (2.7 %) secondary screw perforations encountered in the S3 group compared to two (2.9 %) and four (5.8 %) in the PHLP group. Two patients (2.7 %) in the S3 group and three patients (4.3 %) in the PHLP group had humeral head necrosis. Three patients (4.3 %) in the PHLP group experienced subacromial impingement because the plate was positioned too far cranially. Complications in detail were summarized in Table 5.
Discussion
As far as we know, this is the first retrospective study comparing S3 humeral plate and proximal humeral locking plate in the treatment of displaced unstable proximal humeral fractures. The aim of this study was to evaluate the effect of the S3 humeral plate and to compare the clinical outcomes, shoulder function and complications of patients with proximal humeral fractures treated either with a S3 or PHLP plate.
In recent years, ORIF with use of a proximal humeral locking plate has become more preferred in treating proximal humeral fractures. However, whether this surgical device is beneficial to patients remains difficult to decipher [17, 18]. A few studies [2, 6] showed the initial results in treating proximal humeral fractures with use of the S3 plate. In these studies, the complication rate was as low as 3.7 %, while with use of a proximal humeral locking plate it was over 20 % according to earlier literature [1, 10, 19, 20]. Even so, the evidence is not enough to judge if the S3 plate performs superior to the proximal humeral locking plate in treating proximal humeral fractures.
In this retrospective study, all the fractures in both groups achieved clinical union after one year. In addition, the average Constant score improved for all groups during the one-year follow-up which confirmed that locking plates are effective implants for displaced unstable proximal humeral fractures. According to the results of the Constant score, the S3 group had better shoulder function at three- and six-month follow-up compared to the PHLP group. Furthermore, patients treated with an S3 plate experienced less pain and better activities of daily living at the 1.5, three and six months follow-up time points (Fig. 4). The reason for the different clinical outcomes between the S3 group and the PHLP group is still unknown. We speculate that the design of the S3 plate may be partly responsible. First, on the plate’s head we could use smooth locked pegs instead of screws to provide subchondral support in humeral head. This design can effectively prevent the screw perforation, especially for the elderly patients with osteoporosis [2, 6]. Second, the contoured undersurface matches the complex shape of the proximal humeral which could act as a reduction template helping doctors in restoring the natural anatomy. Huff et al. [12] conducted a biomechanics study comparing S3 plate and PHILOS plate on cadaveric humeri which showed that the S3 plate was stiffer than the PHILOS plate with varus and valgus bending, as well as in torsion. Third, the S3 plate was positioned just posterior to the bicipital groove, which was suggested to be used as a parameter for ideal plate positioning in proximal humeral fractures [21]. We figured that well-designed and better fixation might be helpful in reducing postoperative pain and benefit early functional rehabilitation, which might lead to a better clinical outcome.
Follow-up data of a 69-year-old female. a Pre-operative radiograph shows a displaced unstable proximal humeral fracture. b CT scan shows a three-part proximal humeral fracture (Neer classified). c Postoperative X-rays taken in anteroposterior and lateral views show a good reduction and proper placement of the S3 plate. d At the one-year follow-up, the patient had good shoulder function. The one-year Constant score was 91
In our study, the total complication rate in the S3 group was 26.7 % while in the PHLP group it was 30.4 % and there was no significant difference. The complication rate was similar to earlier studies [1, 10, 22–24]. The major complication of S3-treated patients was displacement of the greater tuberosity (n = 5, 6.7 %). This result was also noted in a previous biomechanics study. Rose et al. [12] conducted a biomechanical comparison between S3 plate and LCP (locking compression plate) in a cadaveric fracture model, the result of which showed that the S3 plate led to a significantly greater displacement of the greater tuberosity fragment. Of these five patients, two had a second operation to fix the displaced greater tuberosity with use of a mini-plate or compression screws and three immobilized in a sling for an additional six weeks. At the one-year follow-up, both of them achieved clinical union. None of the patients in the S3 group experienced subacromial impingement compared to three (4.3 %) in the PHLP group. This may be due to the designed position of the S3 plate which was proximately positioned 3.0 cm distal to the greater tuberosity, thus theoretically preventing subacromial impingement [2, 6, 11, 12].
Some potential limitations of this study need to be considered. This is a retrospective study and lack of randomization in design is associated with a higher level of evidence. This limitation may lead to a potential treatment allocation bias. Another limitation of this study is that the operations were performed by different surgeons. Although the surgical procedure and postoperative rehabilitation were standardised among the surgeons, the individual difference in the surgical technique as well as in postoperative management still exist. This may influence the clinical outcome. Furthermore, the one-year follow-up may be not enough to draw conclusions on final outcome and long-term complications.
In conclusion, both S3 plate and PHLP can be regarded as useful implants in treating displaced unstable proximal humeral fractures. The patients treated with use of an S3 plate result in a good union rate and functional outcome, which is comparable to the PHLP-treated patients. We suggest that the S3 humerus plate can be considered an additional choice for ORIF of proximal humeral fractures. Unfortunately, the evidence is insufficient to judge if it is superior to a proximal humeral locking plate. Considering the limited conclusions of this study, large multicentre randomized controlled trials with longer follow-up are needed to fully evaluate the role of S3 plate for proximal humeral fractures.
References
Konrad G, Hirschmuller A, Audige L, Lambert S, Hertel R, Sudkamp NP (2012) Comparison of two different locking plates for two-, three- and four-part proximal humeral fractures–results of an international multicentre study. Int Orthop 36:1051–1058
Gille J, Schulz AP, Queitsch C, Paech A, Jurgens C (2008) Initial results of the S3-humerus plate. Open Orthop J 2:133–136
Bahrs C, Stojicevic T, Blumenstock G, Brorson S, Badke A, Stockle U, Rolauffs B, Freude T (2014) Trends in epidemiology and patho-anatomical pattern of proximal humeral fractures. Int Orthop 38:1697–1704
Palvanen M, Kannus P, Niemi S et al (2006) Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res 442:87–92
Li YC, Zhao LY, Zhu L, Li J, Chen AM (2013) Internal fixation versus nonoperative treatment for displaced 3-part or 4-part proximal humeral fractures in elderly patients: a meta-analysis of randomized controlled trials. PLoS ONE 8:e75464
Stoddard JE, Pryce D, Potter D et al (2011) Early experience of managing proximal humerus fractures with the S3 plate. Should Elb 3:215–218
Duralde XA, Leddy LR (2010) The results of ORIF of displaced unstable proximal humeral fractures using a locking plate. J Shoulder Elb Surg 4:480–488
Sun JC, Li YL, Ning GZ et al (2013) Treatment of three-and four-part proximal humeral fractures with locking proximal humerus plate. Eur J Orthop Surg Traumatol 23:699–704
Maier D, Jaeger M, Izadpanah K et al (2014) Proximal humeral fracture treatment in adults. J Bone Joint Surg 96:251–261
Südkamp N, Bayer J, Hepp P et al (2009) Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate results of a prospective, multicenter, observational study. J Bone Joint Surg 91:1320–1328
Huff LR, Taylor PA, Jani J et al (2013) Proximal humeral fracture fixation: a biomechanical comparison of two constructs. J Shoulder Elb Surg 22:129–136
Rose DM, Sutter EG, Mears SC et al (2010) Proximal humeral fractures a biomechanical comparison of locking plate constructs in a cadaveric 3-part fracture model. Geriatr Orthop Surg Rehabil 1:73–77
Neer CS 2nd (1970) Displaced proximal humeral fractures. I. Classification and evaluation. J Bone Joint Surg Am 52:1077–1089
Lin T, Xiao B, Ma X et al (2014) Minimally invasive plate osteosynthesis with a locking compression plate is superior to open reduction and internal fixation in the management of the proximal humerus fractures. BMC Musculoskelet Disord 15:206
Sanders RJ, Thissen LG, Teepen JC et al (2011) Locking plate versus nonsurgical treatment for proximal humeral fractures: better midterm outcome with nonsurgical treatment. J Shoulder Elb Surg 20:1118–1124
Constant CR, Murley AG (1987) A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res 214:160–164
Clement ND (2013) Can we decipher indications and outcomes of the PHILOS plate for fractures of the proximal humerus? Int Orthop 37:1199–1200
Zhou ZB, Gao YS, Tang MJ, Sun YQ, Zhang CQ (2013) Reply to: can we decipher the indications and outcome of the PHILOS plate for fractures of the proximal humerus? Int Orthop 37:1201
Charalambous CP, Siddique I, Valluripalli K et al (2007) Proximal humeral internal locking system (PHILOS) for the treatment of proximal humeral fractures. Arch Orthop Trauma Surg 127:205–210
Koukakis A, Apostolou CD, Taneja T et al (2006) Fixation of proximal humerus fractures using the PHILOS plate: early experience. Clin Orthop Relat Res 442:115–120
Labronici PJ, e Albuquerque RP, Schott V, Pires RE, Belangero WD, Franco JS (2014) Proximal humeral fractures: an understanding of the ideal plate positioning. Int Orthop 38:2191–2195
Yang H, Li Z, Zhou F et al (2011) A prospective clinical study of proximal humerus fractures treated with a locking proximal humerus plate. J Orthop Trauma 25:11–17
Brunner F, Sommer C, Bahrs C et al (2009) Open reduction and internal fixation of proximal humerus fractures using a proximal humeral locked plate: a prospective multicenter analysis. J Orthop Trauma 23:163–172
Thanasas C, Kontakis G, Angoules A et al (2009) Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elb Surg 18:837–844
Acknowledgments
The authors would like to thank Nan Lu and Jing Li for the preparation of this manuscript.
Conflict of interest
The authors have declared that no conflict of interests exist.
Ethical approval
This is a retrospective study. For this type of study formal consent is not required.
Author information
Authors and Affiliations
Corresponding author
Additional information
Fan Zhang, Lei Zhu and Di Yang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, F., Zhu, L., Yang, D. et al. Comparison between the spatial subchondral support plate and the proximal humeral locking plate in the treatment of unstable proximal humeral fractures. International Orthopaedics (SICOT) 39, 1167–1173 (2015). https://doi.org/10.1007/s00264-015-2705-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2705-y