Abstract
Background
The use of tension band wiring (TBW) for comminuted olecranon fractures is less recommendable these days. However, some experts preferentially apply TBW to comminuted fractures resulting in favorable outcomes. We here present the surgical technique using TBW with eyelet and absorbable pins for selected comminuted olecranon fractures and review the clinical and radiographic outcomes.
Methods
Twenty-four surgically treated patients with Colton Group 2C or 2D olecranon fractures in focus on the intermediate fragment (IMF) were enrolled. IMFs were primarily fixed with buried bioabsorbable poly-l-lactic acid pins followed by definitive fixation of the olecranon process with TBW with eyelet. The adequacy of the reconstructed notch was especially estimated by parameters on radiographs using digital imaging software.
Results
The average follow-up was 30 months (10 to 86 months). All 24 fractures achieved union, and the maintenance of the articular curvature was confirmed according to statistical analysis on radiographs. The average elbow flexion was 135.1° (range 100° to 145°), and the average elbow extension was − 4.8° (range − 20° to 10°). The mean Mayo Elbow Performance score was 97.3 points (range 80 to 100 points). No cases of pin migration, infection, nerve problem, heterotrophic ossification, or secondary osteoarthritis were observed.
Conclusions
For selected comminuted olecranon fractures, TBW with the eyelet pins and biodegradable pins could yield satisfactory clinical and radiographic outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tension band wiring (TBW) is a standard technique for displaced olecranon fractures. TBW forms a biomechanical construct which converts the triceps’ traction force into inter-fragmental compression [1]. Meanwhile, contoured locking plates fixation seems to be also favored in complex elbow fracture patterns and extensive comminution from the viewpoint of its inherent locking stability [2,3,4]. Which should be better chosen between two construct types in diverse circumstances is still controversial [5,6,7]. Recently, modified TBW method using eyelet pins has boost clinical and radiographic outcomes of olecranon fractures, thanks to the eyelet structure preventing the backing out of wires [8, 9]. We also have introduced eyelet pins to various types of olecranon fractures, and here we describe our own specific tactics to handle the selected comminuted olecranon fractures with TBW using eyelet pins. This article presents the clinical results of 24 patients with comminuted types involving intermediate fragments (IMF) [10, 11] which be able to surgically treat with combined TBW technique and bioabsorbable poly-l-lactic acid (PLLA) pins fixation.
Patients and methods
The review board of our hospital approved this study. Our strategic focus is placed on IMF of the trochlear notch. Despite the array of established classification for olecranon fractures, IMF is best expressed on the classification system introduced by Colton (Fig. 1) [12,13,14]. In this study, patients suffering the comminuted olecranon fracture belonging Colton 2C or 2D were to be enrolled, while excluding Colton Group 4. Pathological fractures, neurovascular injuries, open fractures, and cases with open growth plates were also excluded. We ultimately enrolled 24 patients (nine men and 15 women) with Colton 2C and 2D at average age of 63 years (range 23–86 years).
Colton classification for olecranon fractures [8]. Colton proposed that olecranon fractures could be divided into four groups. Among the four groups, the oblique group (Group 2) was further subcategorized into four stages, from a single oblique fracture (stage A) to an undisplaced intermediate fragment (IMF) (stage B), a single depressed IMF (stage C), and two or more IMFs (stage D). This figure is with permission from Copyright Clearance Center’s RightsLink ® service
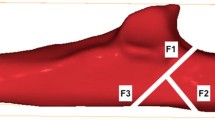
Surgery was performed with the patient in the lateral position under general anesthesia or supraclavicular brachial plexus block. The fracture was exposed using a posterior midline incision with a lateral convex curve. The proximal olecranon process with the triceps attached was turned over proximally. After the debridement of hematoma and interposed soft tissues, the impacted and comminuted IMFs were exposed. The IMFs were elevated so that the articular surfaces of IMFs adequately fit the trochlea of the humerus. If a bone defect was created by the elevation of IMFs, calcium hydroxyapatite ceramic (HA) (NEOBONE, Aimedic MMT Co., LTD., Tokyo, Japan) was filled up into the defect. IMFs were fixed with one or more buried PLLA pins (GRAND FIX, Gunze Medical Division, Tokyo, Japan) (1.5 mm diameter, 20–30 mm length), depending on each fragment size (Fig. 2). If the reduction of IMFs was piled up longitudinally, PLLA pins were planned to be transfixed into multiple fragments. The proximal olecranon process was repositioned and stabilized with the TBW system with eyelet (either Ring Pin, Teijin Nakashima Medical Co., Ltd., Okayama, Japan or Tension Band Pin System, Acumed, Hillsboro, OR, USA). One pair of eyelet pin was inserted into the intramedullary cavity along the long axis of the ulna, as dorsally as possible to escape from stabilized IMFs. Figure-of-eight wiring was tightened through the eyelet portion under the tendon of the triceps (Fig. 3). An arm splint was applied for 2 weeks postoperatively, followed by active range of motion (ROM) exercises. The clinical results were evaluated according to the Mayo Elbow Performance score (MEPS). Postoperative complications, hardware removal, and radiographic results were also reviewed. The number of IMFs, used PLLA pins and HA was recorded. To estimate whether over-compression occurred or not, the adequacy of reduction on the lateral view of the elbow joint was assessed by the maintenance of the articular curvature of the olecranon notch by using the following three parameters on the imaging software (Radiograph: Centricity, GE Healthcare Japan Corp., Tokyo, Japan, CT: AquariusNET, TeraRecon Inc., CA, USA): (A) the straight line distance between the tips of the olecranon process and the coronoid process, (B) the maximum antero-posterior diameter of the trochlea of the humerus, and (C) the length of the line drawn vertically from line A to the deepest part of the olecranon notch. B/A and C/A were calculated and defined as two types of value expressing the articular curvatures [15] (Fig. 4). We compared the measurements of B/A and C/A, respectively, immediately after surgery and at the final follow-up with the paired t test. An error level of less than 5% (p value, 0.05) was defined as statistically significant (SPSS Statistics, ver. 22, IBM Japan, Ltd., Tokyo, Japan).
The schemas of reconstruction and stabilization for comminuted trochlear notch in a virtual case with single–multi-intermediate fragments (IMFs). The left top figure (a) shows a lateral view of the proximal ulna with a single depressed IMF. The left bottom figure (b) demonstrates that the IMF was elevated so that its articular surface adequately fits the face of the trochlea of the humerus. If a bone defect was produced, calcium hydroxyapatite ceramic (HA) (NEOBONE, Aimedic MMT Co., LTD., Tokyo, Japan) was implanted as a bone substitute (black thick arrow). The IMF was fixed not to stick over the surface by two poly-l-lactic acid (PLLA) pins (GRAND FIX, Gunze Medical Division, Tokyo, Japan) (black thin arrow). The right top figure (c) shows antero-posterior view of the proximal ulna with two depressed IMFs. The right bottom figure (d) shows that IMFs were anatomically reconstructed with a total of four PLLA pins (black thin arrow) and one HA block (black thick arrow)
Radiographs of the elbow in sample case with double IMFs. a, b Anterio-posterior and lateral view of initial radiographs. c, d Two sagittal images (c: ulnar side and d: radial side) of reconstructed CT preoperatively best demonstrate Colton classification Group 2D olecranon fracture. e, f Anterio-posterior and lateral view of radiographs postoperative immediately. g, h Anterio-posterior and lateral view of radiographs postoperative at 14 months. Union was achieved at all fracture sites. The extension and flexion angles of the elbow were, respectively, − 3° and 140°, and Mayo Elbow Performance score was 100 points
Three parameters (A, B, and C) were set to assess the maintenance of the articular curvature of the olecranon notch. I The straight line distance (A) between the tips of olecranon process and coronoid process. II The maximum antero-posterior diameter (B) of the trochlea of the humerus. III The length (C) of the line drawn vertically from the line A to the deepest part of the olecranon notch. B/A and C/A were calculated and defined as two types of value expressing the articular curvatures
Results
All patients had unilateral involvement. Ten patients had Group 2C, and 14 had Group 2D fractures. Seven cases had an associated elbow dislocation. One case had an associated clavicle fracture on the ipsilateral side. The number of IMFs was single (i.e., Group 2C) in 10, double in 11, and triple in 3. Multiple IMFs were located transversely in 5 cases, longitudinally in no case, and irregularly arrayed in 9 cases. The average number of used PLLA pins was 2.0 in Group 2C and 2.8 in Group 2D. HA blocks were used in 21 cases. Ring Pin was used in 20 cases, and Tension Band Pin was chosen in 4 cases by surgeon’s preference. Additional Kirschner wire (K-wire) was applied to fix extra-articular comminuted fragment in 3 cases. Another TBW loop was added along the extra K-wire. At the final follow-up averaged 30 months (10 to 86 months), 22 patients had excellent and 2 had good results with a mean MEPS of 97.3 points (80 to 100 points). The average elbow flexion was 135.1° (100° to 145°), and the extension was − 4.8° (− 20° to 10°). Union around both IMFs and olecranon process was obtained in all fractures as judged by bridging trabecular bone. All IMFs did not demonstrate radiographic evidence of collapse or osteonecrosis. Regarding the maintenance of articular curvature, B/A at the final follow-up averaged 0.76 ± 0.06 compared to postoperative immediate values of 0.75 ± 0.07 (p = 0.39). And the final values of C/A averaged 0.45 ± 0.05 compared to postoperative average of 0.44 ± 0.04 (p = 0.11) (Table 1). These small differences were not statistically significant.
Surrounding PLLA pins, reactive line or radiolucent line was not recognized. Neither heterotrophic ossification nor early osteoarthritis was confirmed. There were no major complications such as infection, skin closure problems or nerve injury. Minor complications could be listed up as following problems. A prolonged bone union occurred in two cases and was successfully confirmed at 5 months and 12 months postoperatively, respectively. Subtle irritation at the knot of the soft wire in seven cases and at the tip of the eyelet in two ended up to hardware removal performed at average of 11 months (10 to 13 months). Removal was also conducted in five asymptomatic cases for comparison.
Discussion
TBW technique has been widely accepted and preferred for fixation of olecranon fractures. It is theoretically suitable for converting the triceps’ distractive force into compression [1]. The other advantages are low levels of technical demand, soft tissue damage, and cost. Classical two major drawbacks are (1) the tendency to slide back of K-wires and (2) the possibility of over-compression across comminuted fragments, both resulting in skin or subcutaneous irritation and failure of fixation. Recently, it would be safe to say that the former shortcoming is avoidable, because modified TBW method using eyelet pins with the structure of preventing the back out of wires has been developed and remarked favorable results in practical use [8, 9]. The latter concern has been a causative factor of the debate about which is superior between two major constructs, TBW or plate fixation in clinical settings. Locking plates seem to be practicable for comminuted fracture in favor of its mechanical strength and stability to maintain postoperative reduction [2,3,4]. However, absolute priority of those has yet to be established. In contrast to TBW, locking plates also have some opposite disadvantages that are derived from mechanical lack of the counteraction against the triceps’ tensile and the compressive force into fracture site, plus the longer operation time and high cost [5,6,7]. A few recent studies comparing the two fixation methods in similar materials report no significant clinical and functional difference [5,6,7, 16,17,18], and a certain study claims a slight worse extension of ROM and a longer time to union in plate group [5].
In 2009, Suresh described the unique idea that prior fixation of IMFs by lost K-wire technique can convert the comminuted olecranon fracture to a simple transverse one [11]. In consideration of impracticability of future MRI examination owing to buried stainless implants and eventual risk of perforation, we adopted for bioabsorbable PLLA pins instead of lost K-wire. This method using PLLA pins not only ensures a direct fixation of IMFs, but also provides no concern of a perforation into anywhere, once a PLLA material is absorbed.
In this study, we retrospectively reviewed the clinical and radiographic results of 24 patients with Colton Group 2C and 2D treated with combined TBW technique and PLLA pins fixation. As a result, this method was safely performed and successful in maintaining the articular curvature of the olecranon notch, leading to satisfactory clinical score. As an evidence of reliability on mechanical strength of PLLA pins, various bioabsorbable implants have generally been used in trauma and bone operations [19]. The previous reports describe that the modulus of elasticity is close to that of cortical bone, 200–260 MPa. Their flexural strength is 12–15 GPa. The strength can be maintained for approximately 4 months, which makes them safe for the fixation and healing of articular fragments [19, 20].
Intramedullary pin insertion might help the reduction of IMFs being maintained. In intramedullary pins condition, the compressive force produced by wire tensioning should be prone toward more dorsal than in anterior transcortical pinning, which might protect the IMF locating at anterior side from over-compression [21].
The present study had some limitations as it was based on a retrospective review. Comparative studies with the present TBW technique and locking plate fixation may be appropriate to verify the actual potential of the method. The follow-up period seemed to be short for proper evaluation of elbow arthritis rates and other late complications. Despite a small sample size, our case review suggests that the proposed method might be an encouraging treatment option for comminuted olecranon fractures with IMFs.
Conclusion
In selected comminuted olecranon fractures in focus on IMFs, TBW with the eyelet pins and the fixation of IMFs using absorbable pins could yield satisfactory clinical and radiographic outcomes.
References
Veillette CJ, Steinmann SP (2008) Olecranon fractures. Orthop Clin N Am 39:229–236
Siebenlist S, Torsiglieri T, Kraus T, Burghardt RD, Stöckle U, Lucke M (2010) Comminuted fractures of the proximal ulna—preliminary results with an anatomically preshaped locking compression plate (LCP) system. Injury 41:1306–1311
Niglis L, Bonnomet F, Schenck B, Brinkert D, Di Marco A, Adam P, Ehlinger M (2015) Critical analysis of olecranon fracture management by pre-contoured locking plates. Orthop Traumatol Surg Res 101(2):201–207
Erturer RE, Sever C, Sonmez MM, Ozcelik IB, Akman S, Ozturk I (2011) Results of open reduction and plate osteosynthesis in comminuted fracture of the olecranon. J Shoulder Elbow Surg 20(3):449–454
DelSole EM, Pean CA, Tejwani NC, Egol KA (2016) Outcome after olecranon fracture repair: does construct type matter? Eur J Orthop Surg Traumatol 26(2):153–159
Amini MH, Azar FM, Wilson BR, Smith RA, Mauck BM, Throckmorton TW (2015) Comparison of outcomes and costs of tension-band and locking-plate osteosynthesis in transverse olecranon fractures: a matched-cohort study. Am J Orthop (Belle Mead NJ) 44(7):E211–E215
Matar HE, Ali AA, Buckley S, Garlick NI, Atkinson HD (2014) Surgical interventions for treating fractures of the olecranon in adults. Cochrane Database Syst Rev 80(1):106–111
Kim JY, Lee YH, Gong HS, Lee SL, Lee SK, Baek GH (2013) Use of Kirschner wires with eyelets for tension band wiring of olecranon fractures. J Hand Surg Am 38(9):1762–1767
Takada N, Kato K, Fukuta M, Wada I, Otsuka T (2013) Minimally invasive tension band wiring technique for olecranon fractures. Tech Hand Up Extrem Surg 17(4):199–201
von Rüden C, Woltmann A, Hierholzer C, Trentz O, Bühren V (2011) The pivotal role of the intermediate fragment in initial operative treatment of olecranon fractures. J Orthop Surg Res 6:9
Suresh SS (2009) Management of comminuted olecranon fractures with precut K-wires and tension band wiring. Tech Hand Up Extrem Surg 13:82–84
Colton CL (1973) Fractures of the olecranon in adults: classification and management. Injury 5:121–129
Cabanela ME, Morrey BF (1993) Fractures of the proximal ulna and olecranon. In: Morrey BF (ed) The elbow and its disorders. WB Saunders, Philadelphia, pp 407–408
Benetton CA, Cesa G, El-Kouba Junior G, Ferreira AP, Vissoci JR, Pietrobon R (2015) Agreement of olecranon fractures before and after the exposure to four classification systems. J Shoulder Elbow Surg 24(3):358–363
Kamiya T, Mikami T, Tasase K (2005) Outcome of the comminuted olecranon fractures. J Jpn Soc Surg Elbow 12:123–124 (article in Japanese)
Schliemann B, Raschke MJ, Groene P, Weimann A, Wähnert D, Lenschow S (2014) Comparison of tension band wiring and precontoured locking compression plate fixation in Mayo type IIA olecranon fractures. Acta Orthop Bel 80:106–111
Tarallo L, Mugnai R, Adani R, Capra F, Zambianchi F, Catani F (2014) Simple and comminuted displaced olecranon fractures: a clinical comparison between tension band wiring and plate fixation techniques. Arch Orthop Trauma Surg 134(8):1107–1114
Ren YM, Qiao HY, Wei ZJ, Lin W, Fan BY, Liu J, Li A, Kang Y, Liu S, Hao Y, Zhou XH, Feng SQ (2016) Efficacy and safety of tension band wiring versus plate fixation in olecranon fractures: a systematic review and meta-analysis. J Orthop Surg Res 11(1):137
Matsusue Y, Nakamura T, Iida H, Shimizu K (1997) A long-term clinical study on drawn poly-l-lactide implants in orthopaedic surgery. J Long Term Eff Med Implants 7:119–137
Matsusue Y, Yamamuro T, Oka M, Shikinami Y, Hyon SH, Ikada Y (1992) In vitro and in vivo studies on bioabsorbable ultra-high-strength poly(l-lactide) rods. J Biomed Mater Res 26:1553–1567
Helm RH, Hornby R, Miller SW (1987) The complications of surgical treatment of displaced fractures of the olecranon. Injury 18:48–50
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Research involving human participants
This paper includes clinical and X-ray and CT image data of patients. All procedures performed in this retrospective study involving human participants were in accordance with the ethical standards of Yao Municipal Hospital research committee and with the 1964 Helsinki Declaration and its amendments or comparable ethical standards.
Informed consent
Although this study does not provide informed consent to all patients directly, it is a retrospective study, and it is a study dealing with anonymous data, so it was approved by the ethics committee of Yao Municipal Hospital (ethics examination application form number: 042219-59).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Okamoto, M., Namba, J., Kuriyama, K. et al. Surgical technique in tension band wiring method for selected comminuted olecranon fractures. Eur J Orthop Surg Traumatol 30, 237–242 (2020). https://doi.org/10.1007/s00590-019-02551-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-019-02551-y