Abstract
Purpose
The purpose of this study was to investigate the possible association between single nucleotide polymorphisms (SNPs) rs1800629 (TNF-α -308) and rs361525 (TNF-α -238) of the tumour necrosis factor (TNF)-α gene and susceptibility to osteoarthritis (OA) in the Han Chinese population.
Methods
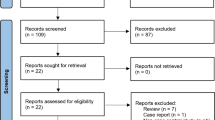
The TNF-α -308 and -238 genotypes were determined by TaqMan assay in 200 OA cases and 305 controls. Odds ratios (ORs) for OA and 95 % confidence intervals (CIs) from unconditional logistic regression models were used to evaluate relative risks.
Results
The frequencies of the allele ‘A’ of rs1800629 were 16 % and 8.85 % in OA cases and in controls, respectively, and thus the -308A allele had a 1.9612-fold (95 % CI = 1.3323–2.8869, P < 0.001) increased risk for OA as compared to the -308G allele. However, no significant differences were found in the genotype and allele frequencies for rs361525 between OA and HC groups.
Conclusions
In the Han Chinese population, the allele ‘A’ of TNF-α -308 may increase the risk for OA, whereas TNF-α -238 polymorphisms do not play a role in OA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a common age-related disease leading to restrictions in daily activities of the elderly, characterised by the destruction of articular cartilage of synovial joints and secondary osteophyte formation [1]. Over the years, there has been strong evidence to suggest an association between joint inflammation and the progression of structural changes in OA [2, 3]. Tumour necrosis factor (TNF)-α, a proinflammatory cytokine, plays an important role in local immune response to invading organisms by initiating a cascade of reactions that culminates into inflammatory response to eliminate the invading organisms [4]. Previous studies had found that levels of TNF-α were elevated in the synovial fluid, synovial membrane, subchondral bone and cartilage [5, 6]. Therefore, TNF-α is considered to play an important role in the pathophysiology of OA [5].
The polymorphisms in the TNF-α promoter appear to play a role in the altered TNF-α gene expression [7–9], and thus the TNF-α promoter polymorphisms may serve as markers of susceptibility to OA. One study [10] observed that rs1800629 (TNF-α -308) single nucleotide polymorphism (SNP) in the TNF-α gene increased the risk for OA in a Korean population, however, another study failed to find the association of this SNP with OA in Western Mexico or the Turkish population [6, 11]. Meanwhile, no significant association between rs361525 SNP (TNF-α -238) and individual susceptibility to OA in a Western Mexico population was found [6]. However, the association of these two SNPs with OA in a Chinese population is unknown. Here, we performed a relatively large-scale case–control study to clarify the potential association between these two SNPs and OA patients from East China.
Methods
Subjects
A total of 200 Han patients with OA from East China were included. The two diagnostic criteria of OA were: (1) any symptom or sign of OA and (2) radiographic findings with Kellgren-Lawrence grade 2 or more. Patients with other forms of arthritis, autoimmune disease, or drug dependence were excluded. For comparison, 305 Han healthy controls (HC) matching in sex, age, and area of residence were recruited. Written informed consent was obtained from each participant involved in this study. Detailed clinical data were recorded and blood samples were collected from all subjects.
Genetic analysis
Genomic DNA was collected from peripheral blood leucocytes in accordance with standard phenol-chloro-form procedures. ALL samples were genotyped for the TNF-α rs1800629 and rs361525 polymorphisms via TaqMan® 5’allelic discrimination technology using a predesigned SNP genotyping assay provided by Applied Biosystems, following manufacturer’s instructions. The resulting data were processed and analysed by the Sequence Detector System 2.0 software (Applied Biosystems, CA). For quality control, random cases (15 %) were processed twice in separate runs. Results were 100 % concordant.
Statistical analysis
To identify the Hardy-Weinberg equilibrium of SNP for OA patients and healthy controls, Fisher’s exact test was performed. The test was also performed to examine genotype and allele frequency for rs1800629 or rs361525 between OA patients and healthy controls. OR with 95 % adjusted by age and gender was estimated in order to identify the role of rs1800629 or rs361525 in OA. All analyses were performed using SPSS 19.0 (SPSS, Inc., Chicago, IL, USA).
Results
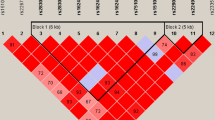
As shown in Table 1, the allele and genotype distributions for rs1800629 and rs361525 in the OA patients and HC did not deviate significantly from the Hardy-Weinberg equilibrium. The distribution of allele ‘A’ of TNF-α -308 in the OA group was significantly higher than that in the HC (p < 0.001, OR 1.9612, 95%CI 1.3323–2.8869), while no significant differences were found in the genotype frequencies for TNF-α -238 between OA patients and HC.
Discussion
In this study, we investigated the relationship between TNF-α gene polymorphisms and individual susceptibility to OA in the Han Chinese population.
The TNF-α gene is located in the central major histocompatibility complex and encodes an important proinflammatory cytokine named TNF-α. Over the years, there has been strong evidence that in OA, TNF-α is one of the most important mediators which alters the balance of cartilage matrix degradation and repair, leading finally to cartilage breakdown [12].
In our study, we found that the allele ‘A’ of TNF-α -308 may increase the risk for OA in the Han Chinese population, which is consistent with the recent results from Korea [10], but not replicated in a Western Mexico or Turkish population [6, 11]. However, rs361525 SNP (TNF-α -238) did not modulate to the susceptibility and did not contribute to the phenotype of OA in the Han Chinese population, which is consistent with the results from the Western Mexico population [6].
As the minor allele frequency of allele ‘A’ of TNF-α -308 or -238 did not differ significantly among ethnicities, the differences of the ethnic group should not contribute to these inconsistent findings. It should be noted here that the studies of Munoz-Valle et al. [6] and Sezgin et al. [11], in which the OA patients/HC were only 50/100 and 151/84, respectively involved small sample sizes. This made it difficult to detect the genotype AA of TNF-α -308 or -238, whose percentage is only about 7 %, leading to the potential of false results. On the other hand, the TNF-α gene and the human leucocyte antigen (HLA) class II/III region, in which some SNPs such as rs7775228 and rs10947262 were identified associated with susceptibility to knee OA [13, 14], are in a linkage disequilibrium state in the chromosome 6p21.3 region. Therefore, positive results shown in the study of Han et al. and our own study may be due to the linkage disequilibrium of the proximal susceptible SNPs. Further genetic research on the relationship between all SNPs in this chromosome region and OA is needed.
In conclusion, our initial research shows that in the Han Chinese population, the allele ‘A’ of TNF-α -308 may increase the risk for OA, whereas TNF-α -238 polymorphisms do not play a role in OA patients. More association studies with larger numbers of participants are needed to confirm the present findings.
References
Reynard LN, Loughlin J (2012) Genetics and epigenetics of osteoarthritis. Maturitas 71(3):200–204. doi:10.1016/j.maturitas.2011.12.001
Hoff P, Buttgereit F, Burmester GR, Jakstadt M, Gaber T, Andreas K, Matziolis G, Perka C, Rohner E (2013) Osteoarthritis synovial fluid activates pro-inflammatory cytokines in primary human chondrocytes. Int Orthop 37(1):145–151. doi:10.1007/s00264-012-1724-1
Pelletier JP, Martel-Pelletier J, Abramson SB (2001) Osteoarthritis, an inflammatory disease: potential implication for the selection of new therapeutic targets. Arthritis Rheum 44(6):1237–1247. doi:10.1002/1529-0131(200106)44:6<1237::aid-art214>3.0.co;2-f
Janeway C, Travers P, Walport M, Capra J (1999) Immunobiology: the immune system in health and disease. Garland Publishers, New York
Kapoor M, Martel-Pelletier J, Lajeunesse D, Pelletier JP, Fahmi H (2011) Role of proinflammatory cytokines in the pathophysiology of osteoarthritis. Nat Rev Rheumatol 7(1):33–42. doi:10.1038/nrrheum.2010.196
Munoz-Valle JF, Oregon-Romero E, Rangel-Villalobos H, Martinez-Bonilla GE, Castaneda-Saucedo E, Salgado-Goytia L, Leyva-Vazquez MA, Illades-Aguiar B, Alarcon-Romero LD, Espinoza-Rojo M, Parra-Rojas I (2012) High expression of TNF alpha is associated with -308 and -238 TNF alpha polymorphisms in knee osteoarthritis. Clin Exp Med. doi:10.1007/s10238-012-0216-3
Kroeger KM, Carville KS, Abraham LJ (1997) The -308 tumor necrosis factor-alpha promoter polymorphism effects transcription. Mol Immunol 34(5):391–399
Wilson AG, Symons JA, McDowell TL, McDevitt HO, Duff GW (1997) Effects of a polymorphism in the human tumor necrosis factor alpha promoter on transcriptional activation. Proc Natl Acad Sci USA 94(7):3195–3199
Uglialoro AM, Turbay D, Pesavento PA, Delgado JC, McKenzie FE, Gribben JG, Hartl D, Yunis EJ, Goldfeld AE (1998) Identification of three new single nucleotide polymorphisms in the human tumor necrosis factor-alpha gene promoter. Tissue Antigens 52(4):359–367
Han L, Song JH, Yoon JH, Park YG, Lee SW, Choi YJ, Nam SW, Lee JY, Park WS (2012) TNF-alpha and TNF-beta polymorphisms are associated with susceptibility to osteoarthritis in a Korean population. Korean J Pathol 46(1):30–37. doi:10.4132/KoreanJPathol.2012.46.1.30
Sezgin M, Barlas IO, Ankarali HC, Altintas ZM, Turkmen E, Gokdogan T, Sahin G, Erdal ME (2008) Tumour necrosis factor alpha -308G/A gene polymorphism: lack of association with knee osteoarthritis in a Turkish population. Clin Exp Rheumatol 26(5):763–768
Sellam J, Berenbaum F (2010) The role of synovitis in pathophysiology and clinical symptoms of osteoarthritis. Nat Rev Rheumatol 6(11):625–635. doi:10.1038/nrrheum.2010.159
Shi D, Zheng Q, Chen D, Zhu L, Qin A, Fan J, Liao J, Xu Z, Lin Z, Norman P, Xu J, Nakamura T, Dai K, Zheng M, Jiang Q (2010) Association of single-nucleotide polymorphisms in HLA class II/III region with knee osteoarthritis. Osteoarthr Cartil/OARS Osteoarthr Res Soc 18(11):1454–1457. doi:10.1016/j.joca.2010.07.009
Nakajima M, Takahashi A, Kou I, Rodriguez-Fontenla C, Gomez-Reino JJ, Furuichi T, Dai J, Sudo A, Uchida A, Fukui N, Kubo M, Kamatani N, Tsunoda T, Malizos KN, Tsezou A, Gonzalez A, Nakamura Y, Ikegawa S (2010) New sequence variants in HLA class II/III region associated with susceptibility to knee osteoarthritis identified by genome-wide association study. PLoS One 5(3):e9723. doi:10.1371/journal.pone.0009723
Acknowledgments
This study was supported by grants from the Shanghai Municipal Health Bureau Program, China (No. 2010164), National Key Constructive Disciplines of China (No.T0303), and the Cultivation Program of “Advanced Reserve Expert”, General Practice of Traditional Chinese Medicine, the Key Disciplines of Traditional Chinese Medicine, State Administration of Traditional Chinese Medicine in "Twelfth Five-Year" Plan, Shanghai University of Traditional Chinese Medicine, China. The authors wish to thank Dr. Zhongzheng Zhu, Dr. Jianpeng Li, Dr. Yuxiang Jiang and Dr. Yan Zhou for excellent technical assistance.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Bin Ji and Jixiang Shi contributed equally to the work.
Rights and permissions
About this article
Cite this article
Ji, B., Shi, J., Cheng, X. et al. Association analysis of two candidate polymorphisms in the Tumour Necrosis Factor-α gene with osteoarthritis in a Chinese population. International Orthopaedics (SICOT) 37, 2061–2063 (2013). https://doi.org/10.1007/s00264-013-1931-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-013-1931-4