Abstract
Background
Hip replacement using a hemiarthroplasty (HA) is a common surgical procedure in elderly patients with fractures of the femoral neck. Data from the Swedish Hip Arthroplasty Register suggest that there is a higher risk for revision surgery with the bipolar HA compared with the unipolar HA.
Purpose
In this study we analysed the reoperation and the dislocation rates for Exeter HAs in patients with a displaced femoral neck fracture, comparing the unipolar and bipolar prosthetic designs. Additionally, we compared the outcome for HAs performed as a primary intervention with those performed secondary to failed internal fixation.
Methods
We studied 830 consecutive Exeter HAs (427 unipolar and 403 bipolar) performed either as a primary operation for a displaced fracture of the femoral neck or as a secondary procedure after failed internal fixation of a fracture of the femoral neck. Cox regression analyses were performed to evaluate factors associated with reoperation and prosthetic dislocation. Age, gender, the surgeon’s experience, indication for surgery (primary or secondary) and type of HA (unipolar or bipolar) were tested as independent variables in the model.
Results
The prosthetic design (uni- or bipolar) had no influence on the risk for reoperation or dislocation, nor had the age, gender or the surgeon’s experience. The secondary HAs were associated with a significantly increased risk for reoperation (HR 2.6, CI 1.5–4.5) or dislocation (HR 3.3, CI 1.4–7.3) compared to the primary HAs. We found no difference in the risk for reoperation or dislocation when comparing Exeter unipolar and bipolar HAs, but special attention is called for to reduce the risk of prosthesis dislocation and reoperation after a secondary HA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hip replacement using a hemiarthroplasty (HA) is a common surgical procedure in elderly patients with fractures of the femoral neck, either as a primary operation for displaced fractures or as a secondary procedure after failed internal fixation. While the unipolar HA (Fig. 1) has a single articulation of the joint, the bipolar HA (Fig. 2) articulates at two different levels and this design is thought to be associated with less acetabular wear and an increased range of motion compared to the unipolar prosthesis. Theoretically, a bipolar HA is therefore expected to result in better hip function and an increased quality of life in patients with femoral neck fracture compared to a unipolar HA. For these patients the bipolar design could be a natural step between a unipolar HA and a total hip replacement (THR) and give better functional results without increasing the surgical trauma. However, the clinical advantages of the more costly bipolar HA are still unproven [1–5] and, moreover, recent data from the Swedish Hip Arthroplasty Register suggest that the bipolar design might be associated with an increased risk for reoperations [6].
We recently published a randomised controlled trial (RCT) including 120 patients comparing the Exeter unipolar and bipolar prostheses [5]. Although there was a significantly lower rate of acetabular erosion in the bipolar group, there were no significant differences in reoperation rate, hip function or quality of life. However, a statistical power analysis shows that it takes a large number of patients (at least 680) to verify a clinically important difference in reoperation rate.
Recurrent dislocations of the prosthesis are one major indication for revision surgery. Revision surgery due to dislocations is reported to occur in 35–50% of the patients suffering from a dislocated hip prosthesis [7–9]. According to the Swedish Hip Arthroplasty Register, dislocations are the most frequent reason for revision surgery after a HA [6]. However, dislocations treated only with a closed reduction are not reported in the Registry. Therefore, it is important not only to analyse the rate of open reoperations and revision surgery, but also the rate of dislocations treated by closed reduction. Furthermore, it is possible that the risk for dislocation and reoperation is associated with specific bipolar prosthetic brands rather than the bipolar design per se. To the best of our knowledge there is no previous adequately powered study analysing and comparing the reoperation and dislocation rates of the bipolar and unipolar designs.
The primary aim of this study was to analyse the total reoperation rate (including closed reductions of prosthesis dislocations) and dislocation rate of the Exeter unipolar and the bipolar HA in patients with a femoral neck fracture within the context of a large prospective cohort trial. The secondary aim was to compare the total reoperation and dislocation rates between patients operated upon with a HA as a primary procedure or as a secondary procedure after failed internal fixation. The null hypothesis was that the prosthetic design does not affect the risk for reoperation or dislocation.
The study was conducted in conformity with the Helsinki Declaration and was approved by the Regional Ethics Committee in Stockholm (reference no. 2006/1409-31/4 and 2007/1309-32).
Patients and methods
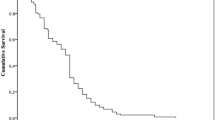
The study was conducted at the Department of Orthopaedics at Stockholm Söder Hospital between September 1, 2000 and December 31, 2006. Stockholm Söder Hospital is a public general hospital with a catchment area comprising 600,000 inhabitants. All patients treated since 1996 have been prospectively registered in a clinical audit database where all early complications (six weeks after surgery) are registered. During the study period a consecutive series of 830 HAs for a femoral neck fracture operated upon via an anterolateral surgical approach [10] were identified in the registry and included in the study. All individual patient records were studied up to December 31, 2009, or death, in order to find information about all late occurring dislocations and reoperations. Finally, the Swedish personal identification number was used to perform a search in the National Board of Health and Welfare’s national registry to find patients who had been treated elsewhere in Sweden for a dislocation or reoperation up to December 31, 2009. No such case was found. The median follow-up time was 3.1 (0–9.1) years for all cases and 4.8 (0–9.1) years for those who were still alive on December 31, 2009.
Baseline data for all patients included in relation to the type of HA are displayed in Table 1. The mean (range) age was 84 (56–99) years for women (n = 609) and 83 (62–98) years for men (n = 221). The indication for the HA procedure was a displaced femoral neck fracture (Garden III and IV) [11] in 676 patients (primary HA) and revision surgery after failed internal fixation of a femoral neck fracture in 154 patients (secondary HA). The prostheses used were a cemented unipolar (Exeter®, Howmedica, Malmö, Sweden) in 427 patients and a cemented bipolar (Exeter®, Howmedica, Malmö, Sweden) in 403. In all patients with a bipolar HA a 28-mm head with a Bicentric (Howmedica, Malmö, Sweden) or a Universal Head Replacement (Howmedica, Malmö, Sweden) was used. The standard anaesthesiology procedure was a spinal anaesthesia for all procedures, except for closed reduction of dislocated prosthesis which was generally performed under general anaesthesia.
Statistical analysis
A power analysis was performed to determine the sample size. We estimated that at least 680 hips (340 hips in each group) were required to detect a clinically important difference in the total reoperation rate of between 5% and 10%, with 80% power at a 95% significance level.
The Mann-Whitney U-test was used for scale variables in independent groups. Nominal variables were tested by the chi-square test or Fisher’s exact test. We used Cox regression to evaluate factors associated with prosthetic dislocation and reoperation. Age, sex, surgeon’s experience, indication for surgery and type of HA were tested as independent variables in the model. First, crude associations for each factor were studied in univariable models. Second, a multivariable model with all independent factors was used to study the adjusted associations. The associations are presented as hazard ratios (HRs) with 95% confidence intervals (CIs). The associations were tested using the Wald test and were considered significant for p < 0.05. All tests were two-sided. The statistical software used was PASW Statistics 18 and SamplePower 2.0 for Windows (SPSS Inc., Chicago, Illinois, USA).
Results
Reoperations (including closed reduction of prosthesis dislocations) were performed in 55 of the 830 hips, giving a total reoperation rate of 6.6%. Dislocation of the HA was the indication for reoperation in 24 of the 830 hips (2.9%) and reoperations for other reasons than dislocation were performed on 31 hips (3.7%). There was no significant difference in the total reoperation rate (7.3% and 6.0%; p = 0.3) or in the dislocation rate (2.8% and 3.0%; p = 0.9) between the unipolar and the bipolar Exeter HAs. The indication for surgery, primary or secondary, was the only factor associated with a significantly increased total risk for reoperation: 13% after a secondary HA compared to 5.2% after a primary HA (p = 0.001). Secondary HA was also associated with a significantly increased risk for dislocation compared to primary HA, at 6.5% and 2.1%, respectively (p = 0.004).
Since there was a trend using the bipolar HA more often in females, as well as in younger patient’s, Cox regression analyses were performed in order to evaluate and adjust for factors of importance for the total risk of reoperation and prosthetic dislocation. The multivariable regression analysis also showed that the indication for surgery was the only factor associated with a significantly increased total risk for reoperation, with HR 2.6 (CI 1.5–4.5) for secondary HA. Furthermore, the indication for surgery was also the only factor associated with a significantly increased risk for dislocation, with HR 3.3 (CI 1.4–7.3) for secondary HA. Age, gender, the surgeon’s experience and type of HA did not significantly affect the total reoperation rate or the dislocation rate (Tables 2 and 3).
Indications for the reoperations and the final outcome for all patients who underwent a reoperation are presented in Table 4. Out of 24 hips with a dislocation, 18 were initially successfully treated by closed reduction. Of the remaining six hips, three HAs were extracted in patients due to severe comorbidities. Two hips displayed incongruence of the joint on the post-reduction radiograph due to acetabular impingement (soft tissue and cement, respectively) and both were reduced openly. One was converted to a THR due to a failed closed reduction and persistent instability during open reduction. Recurrent dislocation occurred in 14 out of the 18 initially closed reduced hips (78%). Of these 14, in the end three HAs were extracted, two were converted to a THR and nine patients were treated with repeated (from two to six) closed reductions. The mean time to the first dislocation was 3.7 (range, 0–27) weeks, and in 21 of 24 (88%) the dislocation occurred within six weeks of surgery.
Deep infection resulting in reoperation occurred in 14 (1.7%) of the hips. In two patients the prosthesis was extracted primarily. Twelve patients were treated with debridement (one to seven times), plus antibiotics, but in the end five of these hips had the HA removed permanently due to persistent infection. Eleven (1.3%) patients sustained a periprosthetic fracture of the femur. Six of them were treated by open reduction and internal fixation, three had a femoral stem revision and in two hips a stem revision combined with insertion of an acetabular socket was performed. Acetabular erosion requiring revision surgery occurred in four hips (0.5%): two in patients with bipolar HA and two in patients with unipolar HA, all of them were revised to a THR. Acetabular fracture and prosthetic stem fracture each occurred in one patient respectively. In the first case the HA was extracted permanently due to acetabular protrusion and in the second a THR was performed after stem exchange.
Discussion
We found no differences in reoperation or dislocation rates between the Exeter unipolar and bipolar HAs, but the rates for reoperation or dislocation were increased for HAs performed as a secondary procedure after failed internal fixation compared to those performed as a primary treatment of a femoral neck fracture.
Our finding of no differences in reoperation and dislocation rates between uni- and bipolar HAs is in conformity with a recently published RCT including 120 patients from our department [5]. In that study there were no differences regarding complications (such as reoperations or dislocations), hip function (Harris hip score) or health related quality of life (EQ-5D) after one year. Others, such as Calder et al. [1] in a study on 250 patients, Cornell et al. [2] in a study including 48 patients, Davison et al. [3] reporting on 187 patients and finally Raia et al. [4] in a study including 115 patients, also failed to present differences in clinical outcome or surgical complications when comparing uni- and bipolar HAs in randomised studies. Subsequently, a Cochrane review from 2010 based on the seven studies published so far concluded that there is currently not enough evidence to support the use of either unipolar or bipolar prosthesis when performing an HA [12].
However, because reoperation or dislocation is still a relatively rare complication, a larger study cohort is needed to address these particular issues. Our power analysis indicated that at least 680 patients are needed to detect a clinically important difference, and none of the above studies included more than 250 patients. To the best of our knowledge, no other study has included a sufficient number of patients to gain enough statistical power to detect clinically relevant differences in reoperation and dislocation rates.
In contrast to our results, the annual report for 2007 from the Swedish Hip Arthroplasty Register indicated an increased risk for reoperations for bipolar HAs compared with unipolar HAs [6]. In the following reports for 2008 and 2009 different HA brands were analysed separately. In the 2008 annual report the Register stated that there was no difference in the reoperation rate between the Exeter uni- and bipolar designs [6]. This statement was updated and altered in the following 2009 report where an increased risk for reoperations with the Exeter bipolar prosthesis compared with the Exeter unipolar prosthesis was reported [6]. However, as previously mentioned, one limitation of the data from the Swedish Hip Arthroplasty Register is the absence of data on closed reductions due to prosthetic dislocations.
We found an increased risk for reoperation or dislocation for secondary HAs, performed after failed internal fixation, when compared with primary HAs. The same finding has been reported by Roberts and Parker [13] in a prospective cohort study on patients operated upon with an uncemented Austin-Moore HA. They found an increased risk for reoperations (12% versus 4%) and dislocations (4% versus 0.8%) in 100 patients with a secondary prosthesis as compared to 730 patients with a primary one. In contrast, we have reported previously in a prospective cohort study on 739 patients that there was no significant difference in the risk of dislocations between primary (5%) and secondary (8%) HAs [14]. However, in that study both antero- and posterolateral surgical approaches were used, as well as three different prosthetic designs. It is well known that a secondary procedure is more technically demanding than primary HA. The soft tissues are often compromised and the patients are frequently severely disabled with poor muscle function prior to the procedure. On the other hand, the secondary HA is usually an elective procedure in a well prepared patient. However, our results together with the fact that the reoperation rate is high after internal fixation of displaced femoral neck fractures [15] emphasise the importance of choosing the best primary operation, i.e. an arthroplasty, for patients fit enough for that procedure.
The bipolar design has a theoretical advantage of less wear on the acetabular cartilage. It has therefore been proposed as a more suitable alternative for more active patients with a longer life expectancy. However, the polyethylene cover of the inner surface of the bipolar head may run the risk of polyethylene wear causing synovitis and loosening of the stem. While several RCTs have failed to present convincing data on differences in clinical outcome between the unipolar and the bipolar designs [1–5] there are few studies which report on acetabular wear using a grading system. Baker et al. [16] introduced a grading system for acetabular erosion as judged from radiographs ranging from 0 (no erosion) to 3 (acetabular protrusion). They reported acetabular erosion in an RCT after three years in 21 of 32 patients (66%) operated upon using a unipolar cemented HA [16]. Thirteen of the 21 patients had only a grade 1 erosion. The same grading system was used in an RCT from our institution including 60 patients with Exeter bipolar HAs showing only 14% erosion (all grade 1) after four years [17]. In another RCT from our institution on 120 patients allocated to treatment with an Exeter uni- or bipolar HA we reported significantly less erosion in the bipolar (5%) group compared to the unipolar (20%) group after one year [5]. Moreover, there was a trend towards worse hip function and a lower quality of life (EQ-5D) among patients with acetabular erosion compared to those without it. These results indicate that the bipolar design may be advantageous for patients with a long life expectancy. However, in our study with a median follow-up of 3.1 to 4.8 years we could not detect any difference in reoperation rate due to acetabular wear (two in each group).
Our results of 6.6% reoperation and 2.9% dislocation rates conform well with other studies on HAs using an anterolateral surgical approach [1, 3, 18, 19]. Although the frequency of dislocation is relatively low when using an anterolateral surgical approach [14, 20], the percentage of patients with at least one recurrent dislocation after a first closed reduction of an HA is high, up to 50% [14, 18, 21], and revision surgery is reported to occur in 35–50% of the patients suffering from a dislocated hip prosthesis [7–9]. Furthermore, recurrent dislocations have a negative effect on the quality of life [22], cause additional hospital costs [23] and may contribute to an increased mortality rate [24].
One way of approaching the dislocation problems in these patients could be to use prostheses with constrained liners. However, even if these prostheses increase the stability, they might cause a limitation in the range of motion, increase the wear and have an increased component failure rate [25]. Another alternative is to use dual mobility sockets, a design where promising long-term results have been reported recently [26].
We found that 14 patients underwent at least one reoperation for infection, giving a deep infection incidence of 1.7%. This is in line with other studies on patients with femoral neck fractures [1, 16, 19]. However, owing to different definitions used in the literature there is a wide variation in the reported incidence of infections after hip arthroplasty.
None of the patients in this study were revised for aseptic loosening of the prosthesis. This is an expected finding in a cohort including old patients with a relatively short life expectancy and low functional demands, and corresponds well with results from the Swedish Hip Arthroplasty Register [6].
The bipolar prosthesis was used more often among females (not significant) and young patients. At our unit, a bipolar instead of a unipolar HA has previously been selected by some surgeons for patients with a longer life expectancy (such as females) because it is thought to cause less acetabular wear and thereby provide better hip function over time. We therefore used a multivariable regression analysis to adjust for these variables and others that could potentially cause a selection bias. A randomised study would be the best way to analyse the influence of the prosthesis design on the risk for reoperation or dislocation, but since such a large number of patients are needed for this particular issue, it is difficult to assess within the context of a conventional RCT. A large prospective cohort trial including consecutive patients and using regression analyses to correct for any selection bias, such as ours, is therefore a good and reliable approach.
One limitation of our study is that we lack a radiological follow-up to be able to determine acetabular wear. However, the clinical endpoint of significant acetabular wear, which is a reoperation, is included in the analysis.
Strengths of our study are the large number of consecutively entered patients, the relatively long follow-up period and the validation of reoperation and dislocation data via the Swedish National Board of Health and Welfare’s nationwide registry. Therefore, we have good reason to assume that our conclusions are valid for this patient cohort.
In summary, the bipolar prosthesis seems to have the advantage of causing less acetabular wear than the unipolar prosthesis, but there have been reports of a higher risk for reoperation for the bipolar design per se. In this large prospective cohort study we could not demonstrate any differences in the reoperation rate or dislocation rate when comparing unipolar and bipolar Exeter prostheses. Another important finding of the study was that there was an increased risk for reoperation or dislocation when using an HA as a secondary implant after failed internal fixation, which highlights the importance of choosing the correct primary operation for patients with displaced femoral neck fractures which in most cases is a primary arthroplasty.
References
Calder SJ, Anderson GH, Jagger C, Harper WM, Gregg PJ (1996) Unipolar or bipolar prosthesis for displaced intracapsular hip fracture in octogenarians: a randomised prospective study. J Bone Joint Surg Br 78:391–394
Cornell CN, Levine D, O'Doherty J, Lyden J (1998) Unipolar versus bipolar hemiarthroplasty for the treatment of femoral neck fractures in the elderly. Clin Orthop Relat Res 348:67–71
Davison JN, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, Gregg PJ (2001) Treatment for displaced intracapsular fracture of the proximal femur. A prospective, randomised trial in patients aged 65 to 79 years. J Bone Joint Surg Br 83:206–212
Raia FJ, Chapman CB, Herrera MF, Schweppe MW, Michelsen CB, Rosenwasser MP (2003) Unipolar or bipolar hemiarthroplasty for femoral neck fractures in the elderly? Clin Orthop Relat Res 414:259–265
Hedbeck CJ, Blomfeldt R, Lapidus G, Törnkvist H, Ponzer S, Tidermark J (2011) Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in the most elderly patients with displaced femoral neck fractures: a randomised, controlled trial. Int Orthop. doi:10.1007/s00264-011-1213-y
Swedish Hip Arthroplasty Register. Annual Reports. http://www.jru.orthop.gu.se/. Accessed 10 April 2011
Woo RY, Morrey BF (1982) Dislocations after total hip arthroplasty. J Bone Joint Surg Am 64:1295–1306
Li E, Meding JB, Ritter MA, Keating EM, Faris PM (1999) The natural history of a posteriorly dislocated total hip replacement. J Arthroplasty 14:964–968
Kotwal RS, Ganapathi M, John A, Maheson M, Jones SA (2009) Outcome of treatment for dislocation after primary total hip replacement. J Bone Joint Surg Br 91:321–326
Hardinge K (1982) The direct lateral approach to the hip. J Bone Joint Surg Br 64:17–19
Garden RS (1961) Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg 43-B:647–663
Parker MJ, Gurusamy KS, Azegami S (2010) Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev:CD001706. doi:10.1002/14651858.CD001706.pub4
Roberts C, Parker MJ (2002) Austin-Moore hemiarthroplasty for failed osteosynthesis of intracapsular proximal femoral fractures. Injury 33:423–426
Enocson A, Tidermark J, Törnkvist H, Lapidus LJ (2008) Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop 79:211–217
Lu-Yao GL, Keller RB, Littenberg B, Wennberg JE (1994) Outcomes after displaced fractures of the femoral neck. A meta-analysis of one hundred and six published reports. J Bone Joint Surg Am 76:15–25
Baker RP, Squires B, Gargan MF, Bannister GC (2006) Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am 88:2583–2589
Hedbeck CJ, Enocson A, Lapidus G, Blomfeldt R, Törnkvist H, Ponzer S, Tidermark J (2011) Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures: a concise four-year follow-up of a randomized trial. J Bone Joint Surg Am 93:445–450
Pajarinen J, Savolainen V, Tulikoura I, Lindahl J, Hirvensalo E (2003) Factors predisposing to dislocation of the Thompson hemiarthroplasty: 22 dislocations in 338 patients. Acta Orthop Scand 74:45–48
Frihagen F, Nordsletten L, Madsen JE (2007) Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ 335:1251–1254
Varley J, Parker MJ (2004) Stability of hip hemiarthroplasties. Int Orthop 28:274–277
Keene GS, Parker MJ (1993) Hemiarthroplasty of the hip—the anterior or posterior approach? A comparison of surgical approaches. Injury 24:611–613
Enocson A, Pettersson H, Ponzer S, Törnkvist H, Dalen N, Tidermark J (2009) Quality of life after dislocation of hip arthroplasty: a prospective cohort study on 319 patients with femoral neck fractures with a one-year follow-up. Qual Life Res 18:1177–1184
Sanchez-Sotelo J, Haidukewych GJ, Boberg CJ (2006) Hospital cost of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am 88:290–294
Blewitt N, Mortimore S (1992) Outcome of dislocation after hemiarthroplasty for fractured neck of the femur. Injury 23:320–322
Williams JT, Ragland PS, Clarke S (2007) Constrained liners for the unstable hip following total hip arthroplasty: a literature review. Int Orthop 31:273–277
Boyer B, Philippot R, Geringer J, Farizon F (2011) Primary total hip arthroplasty with dual mobility socket to prevent dislocation: a 22-year follow-up of 240 hips. Int Orthop. doi:10.1007/s00264-011-1289-4
Conflicts of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Enocson, A., Hedbeck, C.J., Törnkvist, H. et al. Unipolar versus bipolar Exeter hip hemiarthroplasty: a prospective cohort study on 830 consecutive hips in patients with femoral neck fractures. International Orthopaedics (SICOT) 36, 711–717 (2012). https://doi.org/10.1007/s00264-011-1326-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1326-3