Abstract
Background
Hemiarthroplasty (HA) is an effective procedure for treatment of femoral neck fracture. However, it is debatable whether unipolar or bipolar HA is the most suitable implant.
Objective
The purpose of this study was to compare the causes of failure and longevity in both types of HA.
Materials and methods
We retrospectively reviewed 133 cases that underwent revision surgery of HA between 2002 and 2012. The causes of revision surgery were identified and stratified into early (≤ 5 years) failure and late (> 5 years) failure. Survival analyses were performed for each implant type.
Results
The common causes for revision were aseptic loosening (49.6%), infection (22.6%) and acetabular erosion (15.0%). Unipolar and bipolar HA were not different in causes for revision, but the unipolar group had a statistically significantly higher number of acetabular erosion events compared with the bipolar group (p = 0.002). In the early period, 24 unipolar HA (52.9%) and 28 bipolar HA (34.1%) failed. There were no statistically significant differences in the numbers of revised HA in each period between the two groups (p = 0.138). The median survival times in the unipolar and bipolar groups were 84.0 ± 24.5 and 120.0 ± 5.5 months, respectively. However, the survival times of both implants were not statistically significantly different.
Conclusions
Aseptic loosening was the most common reason for revision surgery after hemiarthroplasty surgery in early and late failures. Unipolar and bipolar hemiarthroplasty were not different in terms of causes of failure and survivorship except bipolar hemiarthroplasty had many fewer acetabular erosion events.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hemiarthroplasty (HA) is an effective procedure that is used mostly in treatment of hip fracture in elderly patients [1]. Numerous studies support HA as a treatment of choice due to the lower risk of reoperation, better functional recovery and lower total cost compared to internal fixation [2,3,4]. Apart from fracture treatment, HA was proposed to treat other conditions of hip disease including osteoarthritis and osteonecrosis, but the outcomes of these conditions were not as successful as in femoral neck fracture [5,6,7].
Conversion of failed HA was reported with a high rate of complications [8]. The difficulty in revision surgery depends on the mode of failure. In well-fixed HA with acetabular cartilage erosion, a simple procedure that includes standard acetabular cup replacement without a femoral stem change is an option [9], while either septic or aseptic loosening needs replacement of the femoral stem.
In most studies, the mode of failure was well described in primary total hip replacement [10,11,12,13]. The number of studies that determines the mode of failed HA is limited. Generally, the potential reasons for revision arthroplasty include patient-related, implant-related and surgical technique-related factors [14]. For the implant-related factors, the design of the HA implant can be divided into unipolar and bipolar prostheses. Theoretically, an additional articulation between the femoral head and polyethylene liner of bipolar HA should provide an increased range of motion and prevent acetabular erosion [15], but it can lead to a different mode of failure.
This study aimed to describe the reasons for revision of failed HA and compare the different modes of failure and survivorship between unipolar and bipolar prostheses.
Materials and methods
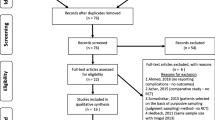
We retrospectively reviewed the data of 417 patients who underwent revision hip arthroplasty in Siriraj Hospital in Thailand between January 2002 and December 2012. Revision of failed total hip replacement (276 cases), conversion of resection arthroplasty (2 cases) and reconstruction after tumor resection (5 cases) were excluded. The remaining 134 revisions of failed HA were recruited. After reviewing the data, one patient with incomplete data was excluded. Finally, a total of 133 patients were included in the data analysis. Fifty-one and 82 of these patients underwent unipolar and bipolar HA, respectively. The data were retrieved from medical records, operative notes, discharge summaries, laboratory investigations and relevant imaging studies. This study was approved by our institutional review board.
The recorded demographic data of the patients included the age at index HA, age at revision surgery, body mass index (BMI), gender, side, primary diagnosis, type of HA, time from index HA to revision and the reason of revision surgery. The primary diagnoses were grouped into either hip fracture or non-hip fracture. Non-hip fracture was classified as failed fixation of hip fracture, primary osteoarthritis (OA), secondary OA (including developmental dysplasia of hip, posttraumatic OA and inflammatory arthritis) and osteonecrosis. The type of HA was classified based on the use of bone cement (cemented or cementless) and type of femoral head prosthesis (unipolar or bipolar). For each HA, the reason for failure was categorized into one of eight categories: aseptic loosening, periprosthetic fracture, periprosthetic joint infection, instability, acetabular erosion, osteolysis, unexplained pain or intraprosthetic dislocation. In the cases that had multiple reasons for the failure, the primary reason was selected by a joint decision of all authors.
Statistical analysis
The data were analyzed using SPSS version 18.0 (SPSS Inc., Chicago, Illinois). Numerical and categorical data were presented as mean ± standard deviation (SD) and percentage, respectively. The differences of data between the unipolar and bipolar groups were analyzed using the unpaired Student’s t test and Chi-squared test. We stratified the time to revision into two periods: early failure (≤ 5 years) and late failure (> 5 years). The reasons for revision of failed HA were classified based on this time period.
In the survival analysis, we used Kaplan–Meier curves to determine the survival of the implants. The starting point was the time of index HA, and the end point was the time of revision surgery. The differences of survival times between unipolar and bipolar HA groups were analyzed using the log-rank and Breslow tests. Statistical significance was determined by a p value less than 0.05.
Results
The mean ages of patients at index surgery and revision surgery were 52.7 ± 17.6 and 61.6 ± 15.1 years, respectively. The majority of the patients were female. Hip fracture was the most common index diagnosis. In a subgroup analysis, the unipolar group was older than the bipolar group (p < 0.001). Unipolar HA was used mainly for hip fracture treatment, while bipolar HA was used for either hip fracture or osteonecrosis treatment. The BMI and type of fixation were similar in both groups (Table 1).
This study found that the common causes for revision were aseptic loosening (49.6%), infection (22.6%) and acetabular erosion (15.0%) (Table 2). When considered by the type of implant, aseptic loosening (41.2%), acetabular erosion (27.5%) and infection (15.7%) were the leading causes of revision in the unipolar HA group. In the bipolar HA group, aseptic loosening (54.9%) and infection (26.8%) were the main causes of failure. The prevalence of acetabular erosion was significantly higher in the unipolar HA group compared to the bipolar HA (p = 0.002).
Based on a time period stratification, the main reasons for revision of HA in the early period were aseptic loosening (38.5%), infection (34.6%) and fracture (15.4%). In the late failure period, the common causes of failure were aseptic loosening (56.8%) followed by acetabular erosion (18.5%) and infection (14.8%) (Table 3). In the early period, 24 unipolar HA (52.9%) and 28 bipolar HA (34.1%) failed. In the late period, 27 unipolar HA (47.1%) and 54 bipolar HA (65.9%) failed. There was no significant difference in the number of revised HA in each period between the two groups (p = 0.138) (Table 4).
The most common causes of early failure for unipolar and bipolar HA were aseptic loosening and infection, respectively. For late failure of unipolar HA, aseptic loosening and acetabular erosion were the major causes. Likewise, aseptic loosening was also the main cause of late failure in bipolar HA (Table 4).
In unipolar HA, both types of stem fixation had no significantly difference in term of causes of failure. In bipolar HA, cementless bipolar HA was mostly failed from aseptic loosening but cemented bipolar HA was failed from infection (Table 5).
In the survival analysis, the Kaplan–Meier curve for all data is shown in Fig. 1. The overall median survival time was 108.0 ± 6.1 months (95% CI 96.0–120.0). To compare the survival time of each HA type, the survival curves of unipolar and bipolar HA are shown in Fig. 2. The median survival times of the unipolar and bipolar groups were 84.0 ± 24.5 and 120.0 ± 5.5 months, respectively; however, no significant differences in the survival times between the groups were found when analyzed using either the log-rank (p = 0.468) or Breslow tests (p = 0.105).
Discussion
Hemiarthroplasty is the implant of choice in treatment of femoral neck fracture in elderly patients. But it is still debatable whether unipolar or bipolar HA is suitable for these patients. A recent meta-analysis [16, 17] showed no statistical significance in the clinical outcomes between unipolar or bipolar HA. Most of the published studies were in developed countries that have fewer financial problems in their healthcare systems compared with developing countries. The use of implants in our country is usually not strictly evidence based but must be adapted to the economic situation. This can be inferred from the results which showed that 25% of bipolar HA was used in the treatment of osteonecrosis. This study provided the results of HA in a wider range of diseases than previous studies.
This study found that the median survival times for the unipolar and bipolar groups were 84.0 ± 24.5 and 120.0 ± 5.5 months, respectively, but the difference did not reach a statistically significant level. Kanto et al. [18] published a prospective randomized control study that compared functional outcomes and survivorship between unipolar and bipolar HA. They found no difference in functional outcomes except a higher dislocation rate in the unipolar group. Both implants had excellent survivorship at 8-year follow-ups. From these results, the longevity of the implants may not be related to the type of articulating surface but may relate to the fixation technique of the femoral stem. Many registry-based studies showed that a cementless fixation had poorer survivorship than cemented fixation in HA and total hip replacement [19,20,21].
The three most common reasons for revision hemiarthroplasty were aseptic loosening (49.6%), infection (22.6%) and acetabular erosion (15.0%). These were quite similar to the failure mode of total hip replacement except acetabular erosion which is a unique failure of HA [10, 13]. Bipolar articulation has the theoretical advantage of preventing acetabular erosion by reducing movement between the acetabular cartilage and prosthesis interface [22]. Some published studies contradict this using radiological examinations in patients who underwent bipolar HA implantation. They found that the movement between the femoral head of the prosthesis and the liner were diminished over time and acted like a unipolar HA. But several clinical studies including this study confirmed that bipolar HA has a lower rate of acetabular erosion compared with unipolar HA [17, 23, 24].
One case of bipolar HA in this study was revised because of dissociation of components. This is a rare complication of modular components but many cases were reported. Dissociation can occur at the moment of dislocation and as a complication during reduction. Polyethylene wear of the locking mechanism was thought to be the cause during dislocation but locking of the acetabular shell with the posterior rim of acetabular coupling with a twisting force during reduction could disengage the modular components [25, 26].
In the case of unipolar HA, aseptic loosening was the major cause in early failure. We thought that a poor cementing technique or the limitation of available sizes of implants possibly led to this problem. In late failure, acetabular erosion is an added major cause that should be a concern.
Cementless bipolar HA had more number of revision for aseptic loosening compare to cemented fixation. Osteoporotic bone of patients who had fracture may not good enough to maintain initial fixation when using cementless method. Other study from national registries also found the risk of revision was higher for cementless fixation [19, 20].
There are several limitations in this study. First, this study was a retrospective design that limited the acquisition of some data. Second, this study enrolled only revision cases. There was a selection bias to cases that were healthy enough to tolerate the revision procedure. Third, the sample size was small which caused a lack of power to identify the risk factors for failure in each group. Fourth, patients diagnosed with osteoarthritis and osteonecrosis should not represent a failure of implant use in the present study that is limited to femoral neck fracture.
Conclusion
Aseptic loosening is the most common reason for revision surgery after hemiarthroplasty surgery in both early and late failure. Unipolar and bipolar hemiarthroplasty were not different in terms of cause of failure and survivorship except bipolar hemiarthroplasty had many fewer acetabular erosion events.
References
Rogmark C, Leonardsson O (2016) Hip arthroplasty for the treatment of displaced fractures of the femoral neck in elderly patients. Bone Joint J. https://doi.org/10.1302/0301-620X.98B3
Parker MJ (2015) Hemiarthroplasty versus internal fixation for displaced intracapsular fractures of the hip in elderly men: a pilot randomised trial. Bone Joint J 97-B:992–996. https://doi.org/10.1302/0301-620X.97B7.35524
Frihagen F, Waaler GM, Madsen JE et al (2010) The cost of hemiarthroplasty compared to that of internal fixation for femoral neck fractures. Acta Orthop 81:446–452. https://doi.org/10.3109/17453674.2010.492763
Jiang J, Yang C-H, Lin Q et al (2015) Does arthroplasty provide better outcomes than internal fixation at mid- and long-term followup? A meta-analysis. Clin Orthop Relat Res 473:2672–2679. https://doi.org/10.1007/s11999-015-4345-3
Prieskorn D, Burton P, Page BJ, Swienckowski J (1994) Bipolar hemiarthroplasty for primary osteoarthritis of the hip. Orthopedics 17:1105–1111
Pellegrini VD, Heiges BA, Bixler B et al (2006) Minimum ten-year results of primary bipolar hip arthroplasty for degenerative arthritis of the hip. J Bone Joint Surg Am 88:1817–1825. https://doi.org/10.2106/JBJS.01879.pp
Muraki M, Sudo A, Hasegawa M et al (2008) Long-term results of bipolar hemiarthroplasty for osteoarthritis of the hip and idiopathic osteonecrosis of the femoral head. J Orthop Sci 13:313–317. https://doi.org/10.1007/s00776-008-1238-2
Warwick D, Hubble M, Sarris I, Strange J (1998) Revision of failed hemiarthroplasty for fractures at the hip. Int Orthop 22:165–168. https://doi.org/10.1007/s002640050233
Sierra RJ, Cabanela ME (2002) Conversion of failed hip hemiarthroplasties after femoral neck fractures. Clin Orthop Relat Res 399:129–139
Ulrich SD, Seyler TM, Bennett D et al (2007) Total hip arthroplasties: what are the reasons for revision? Int Orthop 32:597–604. https://doi.org/10.1007/s00264-007-0364-3
Clohisy JC, Calvert G, Tull F et al (2004) Reasons for revision hip surgery. Clin Orthop Relat Res 429:188–192. https://doi.org/10.1097/01.blo.0000150126.73024.42
Delaunay C, Hamadouche M, Girard J et al (2013) What are the causes for failures of primary hip arthroplasties in France? Clin Orthop Relat Res 471:3863–3869. https://doi.org/10.1007/s11999-013-2935-5
Iamthanaporn K, Chareancholvanich K, Pornrattanamaneewong C (2015) Revision primary total hip replacement: causes and risk factors. J Med Assoc Thai 98:93–99
Wroblewski BM (1984) Current trends in revision of total hip arthroplasty. Int Orthop 8:89–93
Alazzawi S, Sprenger De Rover WB, Brown J, Davis B (2012) The conversion rate of bipolar hemiarthroplasty after a hip fracture to a total hip arthroplasty. Clin Orthop Surg 4:117–120. https://doi.org/10.4055/cios.2012.4.2.117
Yang B, Lin X, Yin XM, Wen XZ (2015) Bipolar versus unipolar hemiarthroplasty for displaced femoral neck fractures in the elder patient: a systematic review and meta-analysis of randomized trials. Eur J Orthop Surg Traumatol 25:425–433. https://doi.org/10.1007/s00590-014-1565-2
Jia Z, Ding F, Wu Y et al (2015) Unipolar versus bipolar hemiarthroplasty for displaced femoral neck fractures: a systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res 10:8. https://doi.org/10.1186/s13018-015-0165-0
Kanto K, Sihvonen R, Eskelinen A, Laitinen M (2014) Uni- and bipolar hemiarthroplasty with a modern cemented femoral component provides elderly patients with displaced femoral neck fractures with equal functional outcome and survivorship at medium-term follow-up. Arch Orthop Trauma Surg 134:1251–1259. https://doi.org/10.1007/s00402-014-2053-1
Kannan A, Kancherla R, McMahon S et al (2012) Arthroplasty options in femoral-neck fracture: answers from the national registries. Int Orthop 36:1–8. https://doi.org/10.1007/s00264-011-1354-z
Gjertsen J-E, Lie SA, Vinje T et al (2012) More re-operations after uncemented than cemented hemiarthroplasty used in the treatment of displaced fractures of the femoral neck: an observational study of 11,116 hemiarthroplasties from a national register. J Bone Joint Surg Br 94:1113–1119. https://doi.org/10.1302/0301-620X.94B8.29155
Hailer NP, Garellick G, Kärrholm J (2010) Uncemented and cemented primary total hip arthroplasty in the Swedish hip arthroplasty register. Acta Orthop 81:34–41. https://doi.org/10.3109/17453671003685400
Giliberty RP (1983) Hemiarthroplasty of the hip using a low-friction bipolar endoprosthesis. Clin Orthop Relat Res 175:86–92
Hedbeck CJ, Blomfeldt R, Lapidus G et al (2011) Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in the most elderly patients with displaced femoral neck fractures: a randomised, controlled trial. Int Orthop 35:1703–1711. https://doi.org/10.1007/s00264-011-1213-y
Inngul C, Hedbeck CJ, Blomfeldt R et al (2013) Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in patients with displaced femoral neck fractures: a four-year follow-up of a randomised controlled trial. Int Orthop 37:2457–2464. https://doi.org/10.1007/s00264-013-2117-9
Georgiou G, Siapkara A, Dimitrakopoulou A et al (2006) Dissociation of bipolar hemiarthroplasty of the hip after dislocation. A report of five different cases and review of literature. Injury 37:162–168. https://doi.org/10.1016/j.injury.2005.09.014
Yuenyongviwat V, Iamthanaporn K, Hongnaparak T (2015) Spontaneous dissociation of bipolar hip hemiarthroplasty in a patient with nerve palsy: a case report and review of the literature. Int J Surg Case Rep 15:112–115. https://doi.org/10.1016/j.ijscr.2015.08.034
Acknowledgements
The authors wish to thank Siranart Kumpravat for the statistical analyses and to Glenn Shingledecker for reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Iamthanaporn, K., Chareancholvanich, K. & Pornrattanamaneewong, C. Reasons for revision of failed hemiarthroplasty: Are there any differences between unipolar and bipolar?. Eur J Orthop Surg Traumatol 28, 1117–1123 (2018). https://doi.org/10.1007/s00590-018-2176-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00590-018-2176-0