Abstract
Purpose
Hemiarthroplasty (HA) is generally considered to be the treatment of choice in the most elderly patients with a displaced fracture of the femoral neck. However, there is inadequate evidence to support the choice between unipolar HA or bipolar HA. The primary aim of this study was to analyse the outcome regarding hip function and health-related quality of life (HRQoL) in patients randomised to either a unipolar or bipolar HA. The secondary aim was to analyse the degree of acetabular erosion and its influence upon outcome.
Methods
One hundred twenty patients with a mean age of 86 years and an acute displaced fracture of the femoral neck were randomly allocated to treatment by either unipolar or bipolar HA. Outcome measurements included hip function (Harris Hip Score, HHS), HRQoL (EQ-5D) and acetabular erosion. The patients were summoned at four and 12 months for follow-up.
Results
There were no significant differences between the groups regarding complications. The HHS scores were equal at both follow-ups, but there was a trend towards better HRQoL in the bipolar HA group at four months, EQ-5D index score 0.62 vs 0.54 (p = 0.06). Twenty percent of the patients in the unipolar HA group displayed acetabular erosion at the 12-month follow-up compared to 5% in the bipolar HA group (p = 0.03), and there were trends towards worse hip function and HRQoL among patients with acetabular erosion compared to those without: HHS scores 70.4 and 79.3, respectively (p = 0.09), and EQ-5D index scores 0.48 and 0.63, respectively (p = 0.13).
Conclusion
Unipolar HA and bipolar HA appeared to produce equivalent clinical outcomes after one year, but the significantly higher incidence of acetabular erosion in the unipolar HA group may imply that bipolar HA should be the preferred treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The surgical treatment of patients with a femoral neck fracture should be based on the patient’s age, walking ability, comorbidities and life expectancy [1]. Internal fixation (IF) or different types of hip arthroplasties are the available treatment modalities.
In patients with undisplaced fractures (Garden I-II) [2], IF is uncontroversial with an acceptable rate of fracture healing complications and a good outcome regarding function and the health-related quality of life [3]. Internal fixation is also considered to be the treatment of choice in young patients with displaced fractures (Garden III-IV) [4].
In elderly patients suffering from a displaced femoral neck fracture, a cemented hip arthroplasty, compared to IF, has been shown to reduce the reoperation rate and give better hip function and HRQoL [5–7]. In the healthy, active elderly with a long life expectancy, a total hip arthroplasty (THA) is probably the best treatment [6–8] while a hemiarthroplasty (HA) is generally considered to be sufficient for the most elderly patients with lower functional demands and a shorter life expectancy.
There are two different types of HA: unipolar and bipolar. The theoretical advantage of the bipolar HA is a reduction of acetabular wear due to the dual-bearing system. On the other hand, a potential disadvantage is the risk of polyethylene wear that may contribute to mechanical loosening over time and there is also a risk of inter-prosthetic dissociation in certain bipolar HAs necessitating open reduction [9]. However, dissociation appears to be rare in modern bipolar surgical systems.
In a recent international survey sent to 442 orthopaedic surgeons, 94–96% preferred a hip arthroplasty for a patient aged 80 years or more with a Garden type III or IV fracture. The choice was a unipolar HA in 60% and a bipolar HA in 32–33% [4]. However, the choice between a unipolar and a bipolar HA is controversial and difficult to make. In the most recent Cochrane review of this topic [10], there are seven randomised controlled trials (RCTs) comparing unipolar HA with bipolar HA. In three of the trials the now outdated Austin Moore prosthesis was used [11]. The evaluation of the remaining four trials using cemented stems [12–15] resulted in the conclusion that there is inadequate evidence to support or reject the use of a bipolar prosthesis and that further trials are required.
The primary aim of this study was to analyse the outcome regarding hip function and HRQoL after a displaced femoral neck fracture in the most elderly lucid patient randomised to either a unipolar or bipolar HA. The secondary aim was to analyse the degree of acetabular erosion and its influence upon outcome. To the best of our knowledge, this is the first RCT that systematically analyses acetabular erosion after unipolar HA and bipolar HA using a modern hemiarthroplasty with identical stems in both groups.
Patients and methods
One hundred and twenty patients with an acute displaced femoral neck fracture (Garden III and IV) [2] after a fall were entered in to the study. The inclusion criteria were age more than 80 years, absence of severe cognitive dysfunction (more than three correct answers on a ten-item mental test, i.e. the short portable mental status questionnaire (SPMSQ) [16], independent living status (i.e. not institutionalised) and independent walking capability with or without walking aids. Patients with pathological fractures and displaced fractures older than 48 hours and patients with rheumatoid arthritis or osteoarthritis were not included. After clearance by an anaesthetist, the patients were randomised (opaque sealed-envelope technique, independently prepared) to a cemented unipolar HA or a cemented bipolar HA.
Surgical intervention
All operations in both groups were performed by one of 16 surgeons, all specialists in orthopaedic surgery and experienced in both procedures. Both procedures were performed using an anterolateral approach, a modified Hardinge approach [17], with the patient in the lateral decubitus position. The implant used was the Exeter®-stem (modular) with a unipolar head (Unipolar head®; Stryker Howmedica, Malmö, Sweden; Fig. 1) or a bipolar head (UHR®; Stryker Howmedica, Malmö, Sweden; Fig. 2). The unipolar head was available in dimensions from 41 to 56 mm and the bipolar heads in 44 to 72 mm. In the most frequently used sizes, the increment for the unipolar head was 1.5 mm and for the bipolar head 1.0 mm. The diameter of the inner head of the bipolar prosthesis was 28 mm. All patients were given low-molecular-weight heparin (dalteparin sodium) preoperatively and for at least ten days postoperatively. Cloxacillin 2 g was given preoperatively, followed by two additional doses during the first 24 hours.
Patients in both groups were mobilised with full weight bearing as tolerated. The patients were carefully informed about mobilisation techniques. They were allowed to sit on a high chair immediately after surgery and to abandon the crutches at their own convenience. After six weeks there were no restrictions.
Primary assessment and follow-up
The primary assessment included an assessment of cognitive function according to the short portable mental status questionnaire (SPMSQ) [16] and of general health according to the ASA classification [18]. The patients were interviewed regarding living conditions, walking ability, activities of daily living (ADL) status [19], previous hip function and HRQoL according to the EuroQol-5D (EQ-5D) [20] as assessed during the last week before the fracture (recall). Perioperative data, i.e. intraoperative blood loss, need for blood transfusions, and duration of surgery were recorded.
The patients were summoned at four (mean 4.2, SD 0.7) and 12 (mean 12.6, SD 1.3) months for a clinical and radiographic examination. Two patients in the bipolar HA group had a primary unipolar HA because the acetabulum was smaller than the smallest available bipolar head. However, in the outcome analysis all patients remained in the primary randomisation group according to the intention-to-treat principle.
Hip complications, general complications, ADL status, living conditions, hip function (Harris Hip Score, HHS) [21] and EQ-5D were assessed. All clinical variables except hip motion were assessed by an unbiased observer (a research nurse not involved in the surgery or clinical decisions). The research nurse was not blinded to the type of surgical intervention.
Methods
The patient’s general physical health status was assessed by the attending anaesthetist according to the American Society of Anesthesiologists (ASA) classification [18].
The patient’s cognitive function was assessed with the short portable mental status questionnaire (SPMSQ) [16] and only patients without severe cognitive dysfunction, i.e. over three correct answers on the ten-item test, were included.
The Katz ADL index [19] status is based on an evaluation of the functional independence or dependence of patients in bathing, dressing, using the toilet, transferring, continence and feeding. ADL index A indicates independence in all six functions and index B independence in all but one of the six functions. Indexes C–G indicate dependence in bathing and at least one more function.
Living conditions were categorised as independent (living in one’s own home or in housing for the elderly) or as institutionalised (living in a nursing home).
Hip complications such as dislocation, periprosthetic fracture, deep infection and acetabular erosion were recorded. Deep wound infection was defined as an established infection beneath the fascia requiring surgical revision. Radiographs were analysed with regard to acetabular erosion by a radiologist blinded to the clinical outcome. Acetabular erosion was graded according to the criteria of Baker et al. [8] as grade 0 (no erosion), grade 1 (narrowing of articular cartilage, no bone erosion), grade 2 (acetabular bone erosion and early migration), and grade 3 (protrusio acetabuli).
Postoperative general complications (pressure sores and cardiac, pulmonary, thromboembolic or cerebrovascular complications) and new fractures of the lower extremity during the follow-up were recorded.
The Harris hip score [21] assesses hip function in four categories: pain (0–44), function (0–47), absence of deformity (0–4) and range of motion (0–5). The maximum score possible is 100.
The HRQoL was rated using the EQ-5D [20]. An EQ-5D index score of 0 indicated the worst possible health status and a value of 1 indicated best possible health status.
Sample size
A power analysis based on a previous study with similar inclusion criteria [22] indicated that a sample size of 120 patients would provide a power of 90% to identify a five-point difference in the HHS score.
Statistical methods
The statistical software used was SPSS 17.0 for Windows. The Mann-Whitney U-test was used for scale variables and ordinal variables in independent groups. Nominal variables were tested by the chi-square test or Fisher’s exact test. The Wilcoxon signed-ranks test was used to compare the EQ-5D before fracture and at follow-ups. All tests were two-sided. The results were considered significant at p < 0.05 and as trends at 0.05 ≥ p ≤ 0.2.
Ethical approval
The study was conducted in accordance with the Helsinki Declaration, all patients gave their informed consent to participate and the protocol was approved by the local Ethics Committee.
Results
A flow-chart for all patients included is displayed in Fig. 3. Only one patient was lost to the final follow-up.
Baseline data for randomisation groups are shown in Table 1. The overall mean age was 86.4 (range 80–100) years with 76% of the patients being female. The proportion of males was slightly higher in the bipolar group, 30% compared to 18% in the unipolar group. The mean prefracture EQ-5D index score for all patients was 0.81 and 30% used some form of walking aid. Ninety-seven percent of the patients were independent in ADL function or dependent in only one function and 96% were assessed as ASA 2 or 3.
Perioperative data and surgical outcome
There were no differences in the duration of surgery, intraoperative blood loss or need for blood transfusions on comparing the randomisation groups (Table 2).
In the unipolar HA group there were three (5%) hip complications: two prosthetic dislocations and one deep infection. In the bipolar HA group there were six (10%) hip complications: one prosthetic dislocation, two deep infections and three periprosthetic fractures. All hip complications necessitated reoperations, and data on the nine patients undergoing additional surgery are displayed in Table 3. The differences in complication and reoperation rate between the groups were not significant (p = 0.30). The subsequent outcome was uneventful for all but two of the reoperated patients: patient number 68, who had a revision with an uncemented Lubinus MP II due to a periprosthetic fracture with an HHS score at 12 months of 33, and patient number 82, who underwent extraction of the prosthesis due to a deep infection and had an HHS score of 58 at 12 months.
General complications
The number of general complications apart from mortality did not differ between groups. In the unipolar group there were two patients with pressure sores, two with pneumonia and one with a cardiac complication. In the bipolar group there was one patient with DVT and one patient with pulmonary embolisation. In total, five patients sustained additional fractures involving the opposite lower limb before the 12-month follow-up: in the unipolar group, one trochanteric fracture and one femoral neck fracture, and in the bipolar group, two patients with a trochanteric fracture and one with a femoral neck fracture. The overall one-year mortality rate was 17% (20/120): 12% (7/60) in the unipolar HA group and 22% (13/60) in the bipolar HA group (p = 0.14) (Fig. 3). The mortality rate was significantly higher among male patients, 35% (10/29), compared to 11% (10/91) among female patients (p = 0.003).
Functional outcome and HRQoL
Hip function according to the HHS was similar at both follow-ups (Table 4).
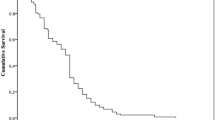
The HRQoL (EQ-5D index score) is displayed in Fig. 4. There was a trend to a better quality of life in the bipolar HA group at four months (p = 0.06) while the difference at 12 months was not significant.
In the unipolar HA group the EQ-5D index score decreased from 0.80 (SD 0.22) before the fracture to 0.54 (SD 0.29) at four months. At 12 months the score was 0.60 (SD 0.30). The values at both follow-ups were significantly lower than before the fracture (p < 0.001 for both comparisons).
In the bipolar HA group the HRQoL (EQ-5D index score) decreased from 0.81 (SD 0.21) before the fracture to 0.62 (SD 0.30) at four months. At 12 months the score was 0.63 (SD 0.28). The values at both follow-ups were significantly lower than before the fracture (p < 0.001 for both comparisons).
There were no differences in ADL or living conditions between the groups at any of the follow-ups. At four months, 71% (42/59) in the unipolar HA group and 71% (40/56) in the bipolar HA group (p = 0.99) were categorised as index A or B and at 12 months, 74% (39/53) and 78% (36/46) (p = 0.59), respectively. At four months, 90% (53/59) in the unipolar HA group and 91% (51/56) in the bipolar HA group (p = 0.62) were still living independently and at 12 months, 96% (51/53) and 98% (45/46), respectively (p = 0.64).
Acetabular erosion
At the final follow-up after 12 months, 93 of the 99 (94%) available patients had an assessable radiographic examination: 49 out of 53 (93%) in the unipolar HA group and 44 out of 46 (96%) in the bipolar HA group. Ten out of 49 patients (20%) in the unipolar HA group displayed acetabular erosion compared to two out of 44 (5%) in the bipolar HA group (p = 0.03). Neither one of the two patients in the bipolar HA group treated with a unipolar HA displayed any signs of acetabular erosion. Excluding these two patients from the analysis gives a rate of acetabular erosion of 5% (two out of 42) in the bipolar HA group and the difference between groups is still significant (p = 0.03). In the unipolar group the acetabular erosion was grade 1 in eight patients and grade 2 in two patients. In the bipolar group one patient had a grade 1 erosion and one a grade 2 erosion.
There was a trend towards worse hip function among patients with acetabular erosion (n = 12) at 12 months compared to those without (n = 81), HHS scores 70.4 and 79.3, respectively (p = 0.09), and also a trend towards a lower quality of life, EQ-5D index scores 0.48 and 0.63 respectively (p = 0.13). The same pattern was seen for ADL function: only 58% (7/12) of the patients with acetabular erosion were categorised as index A or B and at 12 months compared to 79% (64/81) of those without erosion (p = 0.12).
Acetabular erosion occurred more frequently among patients with BMI < 24 kg/m2 (n = 48) compared to those with BMI > 24 kg/m2 (n = 37), 21% (10/48) and 5% (2/37), respectively (p = 0.04). Eight patients had missing values for BMI.
Discussion
The results of our study did not demonstrate any differences regarding complications, hip function and HRQoL in elderly patients with a displaced fracture of the femoral neck randomised to either a unipolar HA or a bipolar HA. However, after one year signs of acetabular erosion were already significantly more frequent after the unipolar HA than the bipolar HA, 20% vs 5%. Furthermore, acetabular erosion appeared to have a negative effect on functional outcome and HRQoL. Overall, the outcome in both groups was good considering the old (mean age 86 years) and frail study population.
Our overall results displaying no differences in complications, hip function and HRQoL are in conformity with the previous four RCTs comparing cemented unipolar HA with cemented bipolar HA. In 1988, Cornell et al. [12] reported no differences in functional outcome in a small study including 48 patients with a six-month follow-up. In 1996, Calder et al. [15] published the results of a study including 250 patients, all aged 80 years or more, with a 1.5–2-year follow-up. A higher proportion of patients returning to their preinjury condition was found in the unipolar HA group, but no other differences were found. In 2001, Davison et al. [13] presented the results from the same study for the 187 patients aged 65–79 years with a minimum two-year follow-up. No differences between randomisation groups were reported, but the interpretation is limited by the fact that 18% of the patients were lost to follow-up. Finally, in 2003, Raia et al. [14] reported the results of a study including 115 patients randomised to a more modern cemented unipolar HA or bipolar HA with identical stems. At the one-year assessment there were no significant differences between the groups in terms of surgical complications, functional outcome or HRQoL according to the SF-36. In our study there was a trend towards better HRQoL according to the EQ-5D at four months in the bipolar HA group, but the difference in favour of the bipolar HA was more limited at the 12-month follow-up and not significant. The EQ-5D index score of 0.63 at 12 months for the bipolar HA group was equal to what we previously reported for patients treated with a bipolar HA [23] and, as expected, both groups reported a significant deterioration in their quality of life compared to before the fracture.
We found an increased rate of acetabular erosion after the unipolar HA compared to the bipolar HA, 20% vs 5%. Moreover, the fact that there was a trend towards worse hip function and lower HRQoL among patients with acetabular erosion at one year may predict a future deterioration that will be more pronounced in the unipolar group. It is difficult to compare these findings with those of previous RCTs as none of the latter, at least as far as can be surmised from the papers, included a systematic radiological follow-up including an assessment of acetabular erosion based on a grading system [8]. However, there are two other studies reporting acetabular erosion based on a systematic radiological follow-up and using the same grading system as our study. Baker et al. [8] reported acetabular erosion in 21 out of 32 patients treated with a unipolar HA after a mean follow-up of 39 months, giving an overall rate of acetabular erosion of 66%. The erosion was assessed as grade 1 in 13 patients, grade 2 in eight and grade 3 in two patients. These results are in sharp contrast to those of a previous RCT from our institution with only 14% acetabular erosion, all grade 1, in patients treated with a bipolar HA (the same prosthesis as in this study) after a mean of 48 months [23]. Considering the advanced age of the study population in our study, mean 86 (range 80–100) years, and a mortality rate of 17% after one year, it is uncertain whether this increased rate of acetabular erosion after the unipolar HA will result in a substantial deterioration in hip function and quality of life during the patients' remaining life time. However, the expected mean survival of an 80-year-old Swedish woman and man in Sweden is, 9.5 and 7.8 years, respectively [24]. These figures indicate that even in this very old population some of the patients will probably experience problems due to acetabular erosion, while it is less likely that the wear of polyethylene in the bipolar head would result in symptomatic loosening of the prosthesis.
There are studies on earlier designs of the bipolar prosthesis showing that the bipolar HA functions as a unipolar HA a few months (3–12) after surgery [25, 26], but the results of our study, displaying a significantly higher rate of acetabular erosion in the unipolar HA group, indicate that there is a real advantage in favour of the bipolar design, which is most probably due to the function of the dual-bearing system. In the most frequently used sizes the increment for the unipolar head was 1.5 mm and for the bipolar head 1.0 mm. In our opinion, this small difference in size will not significantly affect the surgeon’s ability to optimally match the acetabular dimension. However, there was a lower size limit on available bipolar heads. Under this size the inner polyethylene lining becomes too thin. This is reflected in our study by the two patients randomised to a bipolar HA who needed a primary unipolar HA because their acetabulum was smaller than the smallest available bipolar head. It is possible to circumvent this particular problem by using a 22-mm inner head which is currently available for the Exeter® bipolar HA and gives a smallest outer diameter of 41 mm.
Another interesting finding was that acetabular erosion occurred more frequently in patients with a low BMI (<24) than in those with a high BMI (>24), i.e. in 21% compared to 5%. The explanation is unclear. It would be understandable if a high body weight resulted in increased acetabular wear, but there is obviously some other more important mechanism in operation. One possible mechanism could be osteoporosis. We know that low weight is associated with osteoporosis [27], but since we did not evaluate the degree of osteoporosis with DXA in our patients, this remains an hypothesis.
The percentage of hip complications, although not statistically significant, was higher in the bipolar HA group, i.e. 10%, compared to 5% in the unipolar HA group. The main difference was due to three patients in the bipolar HA group sustaining a periprosthetic fracture following a new fall during the first two months after the index operation. As identical prosthetic stems were used in both groups, this particular complication can hardly be blamed on the bipolar design. The other hip complications, namely, deep infection and prosthetic dislocation, were evenly distributed between the groups. The overall dislocation rate was 2.5%, which is what can be expected after an HA performed using the anterolateral approach [28], and there were no inter-prosthetic dissociations in the bipolar HA group. The number of general complications apart from mortality did not differ between groups, but there was a trend towards a higher mortality rate in the bipolar group, i.e. 22%, compared to 12% in the unipolar group. This difference in mortality rate is explained by the random selection of a higher proportion of men to the bipolar group, i.e. 30%, compared to 18% in the unipolar group. As expected, the mortality rate was significantly higher among male patients, i.e. 35%, compared to 11% among female patients. This higher mortality rate among male hip fracture patients is well known and has been confirmed by earlier studies [29].
The strengths of this study were the randomised controlled design, the well-defined population, the use of validated outcome instruments, mostly self-reported, and the high follow-up rate. Moreover, acetabular erosion was assessed by a radiologist blinded to the clinical outcome and using a previously published grading system for acetabular erosion.
A limitation of the study was that, although all clinical variables except hip motion were assessed by an unbiased observer, this observer was not blinded to the type of surgical intervention, which may add a risk of bias. However, as most of the outcome measures, including EQ-5D and HHS, except for range of motion, were self-reported, the risk of bias is assumed to be limited. Furthermore, the fact that our interpretation of the quality-of-life data is based on our patients’ ability to correctly recall their health status prior to the hip fracture may be considered a weakness. However, since it is not possible to collect preinjury HRQoL data prospectively in trauma studies, we have to rely on preinjury recall or a comparison with population figures. Our patient-assessed prefracture EQ-5D index score was slightly higher than in comparable age groups of the Swedish reference population [30], which may be explained by our inclusion criteria, which selected healthier elderly individuals. Furthermore, a recent study reports that older patients can accurately recall their previous health status for up to six weeks [31]. Therefore, we believe that the effect of recall bias can be considered to be limited. In summary, we believe our results are representative of this patient population and that our conclusions are valid.
Which type of HA should we select for the most elderly patients with displaced fractures of the femoral neck? Based on the results of our study and previous ones [12–15], there does not appear to be any clinical disadvantage with the bipolar design. On the contrary, the results of our study showed that the rate of acetabular erosion was significantly lower after the bipolar HA, which in turn may indicate an advantage in the longer term. However, there is one frequently cited disadvantage associated with the bipolar HA, i.e. the higher cost, the magnitude of which probably differs between countries. The difference in cost for the prosthesis used in this study is, according to the present prices at our institution, SEK 1800 higher for the bipolar HA (stem + 28 mm head + bipolar head) compared to the unipolar HA (stem + unipolar head). This is equal to USD 260 according to the present exchange rate. Since there were no differences in duration of surgery, need for blood transfusions, hospital stay and complications during the first year, this difference probably represents the total difference in primary costs for the two treatment modalities. This investment may well be justified in order to reduce the risk of future problems owing to acetabular erosion.
References
Blomfeldt R (2006) Surgical treatment of patients with displaced femoral neck fractures. Aspects on outcome and selection criteria. Karolinska Institutet, Stockholm. http://diss.kib.ki.se/2006/91-7140-801-0/. Accessed 24 January 2011
Garden RS (1961) Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg Br 43:647–663
Tidermark J, Zethraeus N, Svensson O, Törnkvist H, Ponzer S (2002) Quality of life related to fracture displacement among elderly patients with femoral neck fractures treated with internal fixation. J Orthop Trauma 16:34–38
Bhandari M, Devereaux PJ, Tornetta P 3rd, Swiontkowski MF, Berry DJ, Haidukewych G, Schemitsch EH, Hanson BP, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt GH (2005) Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am 87:2122–2130
Rogmark C, Carlsson A, Johnell O, Sernbo I (2002) A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg Br 84:183–188
Keating JF, Grant A, Masson M, Scott NW, Forbes JF (2006) Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am 88:249–260
Blomfeldt R, Törnkvist H, Ponzer S, Söderqvist A, Tidermark J (2005) Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg Am 87:1680–1688
Baker RP, Squires B, Gargan MF, Bannister GC (2006) Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am 88:2583–2589
Varley J, Parker MJ (2004) Stability of hip hemiarthroplasties. Int Orthop 28:274–277
Parker MJ, Gurusamy KS, Azegami S (2010) Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev 6:CD001706
Parker MI, Pryor G, Gurusamy K (2010) Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomised controlled trial in 400 patients. J Bone Joint Surg Br 92:116–122
Cornell CN, Levine D, O'Doherty J, Lyden J (1998) Unipolar versus bipolar hemiarthroplasty for the treatment of femoral neck fractures in the elderly. Clin Orthop Relat Res 348:67–71
Davison JN, Calder SJ, Anderson GH, Ward G, Jagger C, Harper WM, Gregg PJ (2001) Treatment for displaced intracapsular fracture of the proximal femur. A prospective, randomised trial in patients aged 65 to 79 years. J Bone Joint Surg Br 83:206–212
Raia FJ, Chapman CB, Herrera MF, Schweppe MW, Michelsen CB, Rosenwasser MP (2003) Unipolar or bipolar hemiarthroplasty for femoral neck fractures in the elderly? Clin Orthop Relat Res 259–265
Calder SJ, Anderson GH, Jagger C, Harper WM, Gregg PJ (1996) Unipolar or bipolar prosthesis for displaced intracapsular hip fracture in octogenarians: a randomised prospective study [see comments]. J Bone Joint Surg Br 78:391–394
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23:433–441
Hardinge K (1982) The direct lateral approach to the hip. J Bone Joint Surg Br 64:17–19
Owens WD, Felts JA, Spitznagel EL Jr (1978) ASA physical status classifications: a study of consistency of ratings. Anesthesiology 49:239–243
Katz S, Ford A, Moskowitz R, Jackson B, Jaffe M (1963) Studies of illness in the aged The index of ADL: A standardized measure of biological and psychological function. JAMA 185:94–99
Brooks R (1996) EuroQol: the current state of play. Health Policy 37:53–72
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Tidermark J, Ponzer S, Svensson O, Söderqvist A, Törnkvist H (2003) Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg Br 85:380–388
Hedbeck C, Enocson A, Lapidus G, Blomfeldt R, Törnkvist H, Ponzer S, Tidermark J (2011) Comparison of bipolar hemiarthroplasty with total hip arthroplasty for displaced femoral neck fractures. A concise four-year-follow-up of a randomized trial. J Bone Joint Surg Am (in press)
SCB (2010) Statistics Sweden (in Swedish). http://www.scb.se. Accessed 24 January 2011
Phillips TW (1987) The Bateman bipolar femoral head replacement. A fluoroscopic study of movement over a four-year period. J Bone Joint Surg Br 69:761–764
Verberne GH (1983) A femoral head prosthesis with a built-in joint. A radiological study of the movements of the two components. J Bone Joint Surg Br 65:544–547
Coin A, Sergi G, Beninca P, Lupoli L, Cinti G, Ferrara L, Benedetti G, Tomasi G, Pisent C, Enzi G (2000) Bone mineral density and body composition in underweight and normal elderly subjects. Osteoporos Int 11:1043–1050
Enocson A, Tidermark J, Törnkvist H, Lapidus LJ (2008) Dislocation of hemiarthroplasty after femoral neck fracture: better outcome after the anterolateral approach in a prospective cohort study on 739 consecutive hips. Acta Orthop 79:211–217
Söderqvist A, Ekström W, Ponzer S, Pettersson H, Cederholm T, Dalen N, Hedström M, Tidermark J (2009) Prediction of mortality in elderly patients with hip fractures: a two-year prospective study of 1,944 patients. Gerontology 55:496–504
Burström K, Johannesson M, Diderichsen F (2001) Swedish population health-related quality of life results using the EQ-5D. Qual Life Res 10:621–635
Marsh J, Bryant D, MacDonald SJ (2009) Older patients can accurately recall their preoperative health status six weeks following total hip arthroplasty. J Bone Joint Surg Am 91:2827–2837
Acknowledgements
This study was supported in part by grants from the Trygg-Hansa Insurance Company and through the Regional Agreement on Medical Training and Clinical Research (ALF) between the Stockholm County Council and Karolinska Institutet.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hedbeck, C.J., Blomfeldt, R., Lapidus, G. et al. Unipolar hemiarthroplasty versus bipolar hemiarthroplasty in the most elderly patients with displaced femoral neck fractures: a randomised, controlled trial. International Orthopaedics (SICOT) 35, 1703–1711 (2011). https://doi.org/10.1007/s00264-011-1213-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1213-y