Abstract
The Dual Bearing Knee (DBK) prosthesis is a new concept which has a mobile-bearing insert. In May 2001, the posterior femoral condyle design of the DBK was changed to become smaller and there was a posterior shift in the base of the insert dish (Hi-Flex). Between 1998 and 2004, 371 DBKs (112 Hi-Flex and 220 Standard) were performed by one surgical team. There was a significant difference in postoperative flexion angle between the Hi-Flex and Standard DBKs (117.0° and 111.3°; p = 0.001). The delta flexion angle in the Hi-Flex (−2.4°) was significantly increased compared with that in the Standard DBK (−9.6°) (p = 0.001). In the Hi-Flex DBK, the postoperative flexion angle (5.7°) and the delta flexion angle (7.2°) were significantly larger than for the Standard DBK (p < 0.001). These results suggest that the flexion is greater for a design with smaller posterior condyle prosthesis and with a posterior shift in the base of the insert dish in CR mobile-bearing TKA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Total knee arthroplasty (TKA) is associated with excellent clinical results, particularly in terms of pain alleviation and gait recovery. In recent years, demand has increased for TKA that can achieve deeper flexion, such as sitting erect with the legs flexed or kneeling. Many studies have been conducted on range of motion of the knee following TKA, and preoperative range of motion is generally accepted as the most important factor [1]. However, whether the posterior design changes in CR mobile-bearing TKA affects range of motion following TKA remains unclear. In May 1998, we developed a fully congruent designed mobile-bearing knee replacement (the Dual Bearing Knee; DBK prosthesis) in collaboration with Finsbury UK. In May 2001, in order to achieve a greater range of motion, we reduced the curvature radius of the posterior condyle of the femoral component (no change in anteroposterior diameter or osteotomy) and moved the base of the dish of the insert posteriorly by 3 mm (Fig. 1a, b). The effects of these design changes on postoperative range of motion and degree of postoperative improvement in flexion angle were carefully investigated.
Design changes in the Dual Bearing Knee (DBK). a DBK prosthesis. b With the femoral component, the curvature of the posterior condylar area was reduced from the Standard design (broken arrow) to the Hi-Flex design (solid arrow). c With the insert, the bottom of the dish (solid arrow) was moved posteriorly 3 mm. This lowered the height of the posterior lip (broken arrow)
Materials and methods
In the coronal and sagittal planes, the femoral component of the DBK has a single radius shape, and the insert has the same curvature to improve compatibility with the femoral component. This slot-type insert can rotate freely and glide in the anteroposterior direction. The slot-type insert of DBK allows 6 mm of AP sliding.
The DBK prosthesis is not approved for use in the United States. We investigated the patients with a preoperative flexion angle of over 90° on whom DBK TKA was performed from May 1998 to March 2004. The Hi-Flex-design DBK was used in 122 knees (Hi-Flex group; August 2001–March 2004), while the Standard-design DBK was used in 249 knees (Standard group; May 1998–July 2001). Of these, 112 knees in the Hi-Flex group and 220 knees in the Standard group that could be directly examined between 11 and 13 months after operation served as subjects (follow-up rates: 91.8% and 88.4%, respectively). Demographic data on the patients are summarised in Table 1.
No significant inter-group differences in any of the parameters were identified.
All the operations were done by one surgical team. A medial parapatellar approach and the modified gap technique were used in TKA [2–4]. The posterior cruciate ligament (PCL) was conserved in all cases. Cement fixation was used in all cases, and the surgical wound was sutured at a knee flexion angle of 90°.
The patient’s active range of motion was measured by a physical therapist using a goniometer.
The following data were obtained 11–13 months after surgery and analysed: Knee Society Score, as knee score (KS) divided by functional score (FS); pre- and postoperative range of motion (flexion, extension and total range of motion); degree of improvement (postoperative from preoperative) in flexion, extension and range (delta flexion, delta extension and delta range); femoral–tibial angle (FTA); component angles (alpha, beta, gamma and theta); joint line (JL); posterior condylar offset (PCO); patella tendon length (PTL); and patellar thickness (PT). Differences in these parameters before and after surgery were calculated. Parameters were compared within and between groups. Paired t-tests, Student t-tests and Pearson’s correlation coefficient tests were used, and values of p < 0.05 were considered statistically significant for all analyses.
Results
Table 2 shows clinical outcomes for the Hi-Flex and Standard groups. Knee society score (KS/FS) was significantly improved for both groups (p < 0.001). For pre- and postoperative range of motion, the Hi-Flex group displayed significant improvements in extension angle and range of motion (p < 0.001), while flexion angle was maintained postoperatively. Conversely, in the Standard group, extension angle was significantly improved, but flexion angle was decreased (p < 0.001).
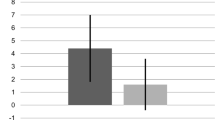
Between the Hi-Flex and Standard groups, no significant intergroup differences in preoperative flexion angle, extension angle or range of motion were noted. Pre- and postoperative mean flexion angles for the Hi-Flex group were 119.4° and 117.0°, respectively, and 120.7° and 111.3° for the Standard group, respectively. There was no difference in the number of patients who lost motion between groups. However, postoperative flexion angle and range of motion were significantly greater for the Hi-Flex group (p = 0.001) (Table 2). The degree of improvement, delta flex and delta range for the Hi-Flex group were also significantly greater (p = 0.001 and 0.005, respectively) (Table 2).
The delta flexion, in standard DBK, 33 knees (29.5%) gained, 14 knees (12.5%) were unchanged, and 65 knees (58%) decreased. In Hi-Flex DBK, 56 knees (26%) gained, 29 knees (13%) were unchanged, and 135 knees (61%) decreased. The percentages of patients who gained and who lost motion are almost the same in both standard DBK and Hi-Flex DBK.
Table 3 shows the results of radiographic measurements. Pre- and postoperative FTAs for the Hi-Flex group were 179.2° and 175.5°, respectively, and 182.0° and 174.8° for the Standard group, respectively. Significant improvements were apparent in both groups (p < 0.001). For both groups, component angles (alpha, beta, gamma and theta) were favourable, and no significant inter-group differences were identified.
JL was measured according to the methods of Figgie et al. [5]. For both groups, JL was significantly increased postoperatively (p < 0.001); however, no significant inter-group difference was found. PCO was measured as described by Bellemans et al. [6]. Significant inter-group differences existed before and after surgery (p = 0.02 and 0.01, respectively). No significant inter-group differences were found in JL, PTL or PT before or after surgery.
As to the degree of improvement in radiographic parameters, delta FTAs for the Hi-Flex and Standard groups were −4.5° ± 6.2 and −7.7° ± 8.0, respectively, and there was a significant inter-group difference (p = 0.04). However, no significant inter-group differences were apparent in the other parameters: delta JL was +2.6 mm ±3.0 and +3.9 mm±4.8, respectively, for the Hi-Flex and Standard groups; delta PTL was +0.3 mm±2.7 and +1.5 mm±5.5, respectively; and delta PT was −0.1 mm±0.9 and +0.3 mm±1.3, respectively.
In order to predict postoperative flexion angle based on preoperative flexion angle for each implant design, a single regression analysis was used to determine a regression line for pre- and postoperative flexion angles for the Hi-Flex and Standard groups (Fig. 2a, b). In both groups, the preoperative flexion angle exhibited a significant correlation to postoperative flexion angle.
Prediction of postoperative flexion angle. Single regression analysis was used to calculate a regression line for flexion angle before and after surgery in both groups. In both groups, pre- and postoperative flexion angles exhibited significant correlations. a Hi-Flex Dual Bearing Knee (DBK). b Standard DBK
A regression line for preoperative flexion angle and delta flex was also determined (Fig. 3). In both groups, the preoperative flexion angle exhibited a significant correlation to delta flex. The results confirmed that preoperative flexion angle has a negative impact on delta flex.
Prediction of change in flexion angle. Single regression analysis was used to calculate a regression line for preoperative flexion angle and the change in flexion angle (delta flex) in both groups. In both groups, significant correlations were found between preoperative flexion angle and delta flex, revealing that preoperative flexion angle exhibited a negative correlation to postoperative flexion angle according to the study; a negative correlation existed between preoperative flexion angle and delta flex, not postoperative flexion angle. Furthermore, values of delta flex for the Hi-Flex and Standard groups were 115.4° and 104.7°, respectively, where pre- and postoperative flexion angles were the same. a Hi-Flex Dual Bearing Knee (DBK). b Standard DBK
An investigation was also performed to identify factors influencing delta flex. In the Standard group, delta flex was significantly greater for RA patients than for OA patients (p = 0.002). In the Hi-Flex group, delta flex was significantly greater for female patients than for male patients (p = 0.003). No significant differences existed with respect to right/left knee and patellar replacement.
In both groups, delta flex exhibited no significant correlation to age, BMI, component angles (alpha, beta, gamma and theta), or preoperative, postoperative and delta values of FTA, JL, PCO, PTL and PT.
Discussion
In the latest reports, the use of navigation, the different types of inserts (fixed-bearing / rotating platform) and the different surgical approaches (modified subvastus / medial parapatellar ) have no influence the flexion angle after total knee arthroplasty [7–9].
What is the factor that improves flexion angle after the total knee arthroplasty?
Our study investigated the effects of implant posterior design changes on postoperative flexion angle following TKA. While the need for design changes to allow greater flexion has been recognised, this is the first study to actually provide clinical data in CR mobile-bearing TKA.
In past studies investigating the posterior condylar design of femoral components, Anouchi et al. [10] used Advantim (Wright Medical Technology, Arlington, TN) and reported no significant difference in degree of postoperative improvement in flexion angle between 232 conventional TKAs and 50 TKAs using a larger posterior condyle for the femoral component. In that study, mean flexion angle two years after surgery was 107° ± 10°, and mean postoperative flexion angle for the Hi-Flex group in our study was about 10° greater, at 117.0° ± 11.3°, suggesting that the effect of the change in their posterior condyle was insufficient.
In PS mobile-bearing TKA, Gupta et al. [11] and Ranawatt et al. [12] used P.F.C.Sigma RP-F and P.F.C.Sigma RP (DePuy Orthopaedics, Inc.,Warsaw, IN) and reported a significant difference in degree of postoperative improvement in flexion angle between 50 Sigma RP-F TKAs and 50 Sigma RP TKAs. The P.F.C.Sigma RP-F changed the radius of curvature of the posterior femoral condyle less than the P.F.C.Sigma RP, suggesting that the effect of the change in their posterior condyle was sufficient.
In our study, by decreasing the curvature of the posterior condyle for the femoral component, the posterior space was enlarged to allow easier rollback mechanism, thus improving postoperative flexion angle. Furthermore, by moving the base of the insert dish in a posterior direction, the height of the posterior lip on the insert was lowered to reduce posterior impingement, thus leading to better results.
In addition, Walker et al. [13] demonstrated that the factors which contribute to the improvement of postoperative ROM are proximal femoral condyle, large posterior offset, small anterior distance, and large posterior slope. In this study, the small anterior distance due to the posterior shift in the base of the insert dish would be useful.
We examined only the clinical data and previously reported in vivo kinematics of Standard DBK with fluoroscopy [14]; we are now investigating the difference in the contact points between Standard DBK and Hi-Flex DBK. Our latest investigation of in vivo kinematics demonstrated that the medial and lateral nearest contact points of Hi-Flex DBK moved significantly posterior compared with Standard DBK (unpublished data).
In our study, in order to exclude the effect of the postoperative period, we compared the postoperative flexion angle at 12 months after operation. Because the periods of the operations between Standard DBK and Hi-Flex DBK were different, if we used the latest follow-up data, the average follow-up periods in each group must be different. However, even when we compared the latest follow-up data, postoperative flexion angle, postoperative range of motion, delta flex and delta range were significantly improved for the Hi-Flex group compared to the Standard group.
Ritter et al. reported that postoperative flexion angle correlated to post- and intraoperative flexion angles [1]. Anouchi et al. assessed delta flex 24 months after surgery by dividing patients into three groups with respect to preoperative flexion angle (<90°, 91–104° and ≥105°) and documented that degree of improvement for the <90° group was 19° greater compared to the 91–104° group and 35° greater when compared to the ≥105° group (p < 0.0001) [10]. Thus, the preoperative flexion angle correlates to the postoperative flexion angle, because if the preoperative flexion angle is small, the degree of improvement is large, but if the preoperative flexion angle is large, the postoperative flexion angle decreases.
In our study, a significant positive correlation existed between pre- and postoperative flexion angles for the Hi-Flex and Standard groups (Fig. 2a, b). Furthermore, a significant negative correlation existed between preoperative flexion angle and delta flex. In this manner, the results in our study are consistent with previous reports [1, 5].
In our study, the value of delta flex would have been zero at 115.4° for the Hi-Flex group and 104° for the Standard group (Fig. 3a, b). We believe that this difference of 10.7° due to the component design change is important for obtaining better results using the Hi-Flex-design DBK.
Regarding the relationship between delta flex and disease type, Schurman et al. reported that the degree of improvement for RA and OA was −8° and −3°, respectively, thus significantly greater for OA [15]. However, Ritter et al. documented no significant differences in postoperative range of motion among patients with OA, RA and ON [1]. In our study, delta flex for the Standard group was −4.9° for RA patients and −12.4° for OA patients, and a significant difference was noted between RA and OA. However, no significant differences were found between RA and OA in the Hi-Flex group, although delta flex tended to be better for RA patients.
For the relationship between delta flex and age, Ritter et al. reported that mean postoperative flexion angle was lower for women than for men [1]. In our study, delta flex for female patients in the Hi-Flex group was significantly greater than that for male patients in the Hi-Flex group.
Figgie et al. reported that, in CR-type TKA, when JL was set high, PCL was overly tense, hindering the rollback mechanism and impairing knee flexion, and they noted that the JL should not increase by more than 8 mm [5]. Kim et al. performed fixed- and mobile-bearing CR-type TKAs and reported that postoperative flexion angle for a group with an increase of ≥5 mm in JL was lower than that for a group with an increase of <5 mm [16]. In our study, JL was significantly increased for both groups, but no significant correlation between delta JL and delta flex was identified. The reason for this was that degree of increase in JL was suppressed for the Hi-Flex and Standard groups at +2.6 and +3.9 mm, respectively.
Bellemans et al. studied 30 patients who underwent CR-type TKA with postoperative flexion of ≥100° by 3-dimensional video fluoroscopy [6]. They reported that because the posterior surface of the femur and insert impinged during maximum flexion in 72% of patients, maintaining the posterior condylar offset would be important. Furthermore, when PCO decreased by 1 mm postoperatively, postoperative flexion angle decreased by 6.1°. In our study, no significant change in PCO was noted for either group. In addition, delta PCO for the Hi-Flex and Standard groups was −0.5 and −0.6 mm, respectively, and no correlation existed between delta PCO and delta flex. However, preoperative PCO for the Hi-Flex and Standard groups was 26.4 and 24.5 mm, respectively, and postoperatively the PCO was 25.9 and 23.9 mm, respectively. The relationship between flexion angle and PCO was investigated before and after surgery, but no correlation was seen between preoperative flexion angle and preoperative PCO, between postoperative flexion angle and postoperative PCO in the Hi-Flex group or between postoperative flexion angle and postoperative PCO in the Standard group. In other words, these findings suggest that PCO is not related to the flexion angle.
In a clinical report, Ryu et al. divided patients into groups displaying favourable post-TKA flexion (≥120°) and poor post-TKA flexion (≤90°), and documented that patellar thickness for the poor flexion group was increased [17]. They subsequently recommended that patellar thickness should remain at the preoperative thickness. Barrack et al. resurfaced the patella within 1 mm of original thickness using calipers and reported no significant differences in postoperative range of motion between a group with patellar replacement and another group without patellar replacement [18]. In our study, no significant difference was noted in patellar thickness before and after surgery in either group. Also, delta PT for the Hi-Flex and Standard groups was −0.1 and +0.3 mm, respectively, and exhibited no correlation to delta flex. Furthermore, no significant difference in delta flex was identified irrespective of whether the patella was replaced.
In conclusion, postoperative flexion angle, postoperative range of motion, delta flex and delta range were significantly improved for the Hi-Flex group compared to the Standard group. In CR mobile-bearing TKA, the results suggest that two design changes improve post-TKA flexion angle of the knee: a smaller radius of curvature for the posterior condyle and a posterior shift in the base of the insert dish.
References
Ritter MA, Harty LD, Davis KE, Meding JB, Berend ME (2003) Predicting range of motion after total knee arthroplasty. Clustering, log-linear regression, and regression tree analysis. J Bone Jt Surg Am 85–A:1278–1285
Lombardi AL Jr (2002) The adult knee. In: Callaghaen JJ (ed) Soft tissue balancing of the knee-flexion. Lippincott Williams &Wilkins, Philadelphia, pp 1223–1232
Parkinson R, Bhalaik V (2001) The valgus and varus knee. Curr Orthop 15:413–422
Macdonald D (2001) Flexion-extension gap theory. Curr Orthop 15:423–427
Figgie HE 3rd, Goldberg VM, Heiple KG, Moller HS 3rd, Gordon NH (1986) The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Jt Surg Am 68:1035–1040
Bellemans J, Banks S, Victor J, Vandenneucker H, Moemans A (2002) Fluoroscopic analysis of the kinematics of deep flexion in total knee arthroplasty. Influence of posterior condylar offset. J Bone Jt Surg Br 84:50–53
Seon JK, Park SJ, Lee KB, Li G, Kozanek M, Song EK (2009) Functional comparison of total knee arthroplasty performed with and without a navigation system. Int Orthop 33:987–990
Hanusch B, Lou TN, Warriner G, Hui A, Gregg P (2009) Functional outcome of PFC Sigma fixed and rotating-platform total knee arthroplasty. A prospective randomized controlled trial. Int Orthop 34:349–354
Jung YB, Lee YS, Lee EY, Jung HJ, Nam CH (2009) Comparison of the modified subvastus and medial parapatellar approaches in total knee arthroplasty. Int Orthop 33:419–423
Anouchi YS, McShane M, Kelly F Jr., Elting J, Stiehl J (1996) Range of motion in total knee replacement. Clin Orthop Relat Res 87–92
Gupta SK, Ranawat AS, Shah V, Zikria BA, Zikria JF, Ranawat CS (2006) The P.F.C. sigma RP-F TKA designed for improved performance: a matched-pair study. Orthopedics 29:S49–S52
Ranawat AS, Gupta SK, Ranawat CS (2006) The P.F.C. sigma RP-F total knee arthroplasty: designed for improved performance. Orthopedics 29:S28–S29
Walker PS, Yildirim G, Sussman-Fort J, Roth J, White B, Klein GR (2007) Factors affecting the impingement angle of fixed- and mobile-bearing total knee replacements: a laboratory study. J Arthroplasty 22:745–752
Watanabe T, Yamazaki T, Sugamoto K, Tomita T, Hashimoto H, Maeda D, Tamura S, Ochi T, Yoshikawa H (2004) In vivo kinematics of mobile-bearing knee arthroplasty in deep knee bending motion. J Orthop Res 22:1044–1049
Schurman DJ, Parker JN, Ornstein D (1985) Total condylar knee replacement. A study of factors influencing range of motion as late as two years after arthroplasty. J Bone Jt Surg Am 67:1006–1014
Kim YH, Kook HK, Kim JS (2001) Comparison of fixed-bearing and mobile-bearing total knee arthroplasties. Clin Orthop Relat Res 101–115
Ryu J, Saito S, Yamamoto K, Sano S (1993) Factors influencing the postoperative range of motion in total knee arthroplasty. Bull Hosp Joint Dis 53:35–40
Barrack RL, Bertot AJ, Wolfe MW, Waldman DA, Milicic M, Myers L (2001) Patellar resurfacing in total knee arthroplasty. A prospective, randomized, double-blind study with five to seven years of follow-up. J Bone Jt Surg Am 83–A:1376–1381
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsuji, S., Tomita, T., Hashimoto, H. et al. Effect of posterior design changes on postoperative flexion angle in cruciate retaining mobile-bearing total knee arthroplasty. International Orthopaedics (SICOT) 35, 689–695 (2011). https://doi.org/10.1007/s00264-010-1060-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1060-2