Abstract
In this paper, we evaluated the difference between the modified subvastus approach and the medial parapatellar approach in total knee arthroplasty(TKA). We assessed the time of active straight-leg raise (SLR) post-operatively and the range of flexion of the operated knee at the tenth post-operative day, 6 weeks and 6 months, 12 months and 3 years. We investigated the degree of the patellar tilt and subluxation 24 months post-operatively. The patients who underwent the modified subvastus approach performed active SLR earlier (mean 0.5 days) than the medial parapatellar approach patients (mean 2.2 days). Knee flexion was better at the tenth post-operative day in the modified subvastus approach group compared to the medial parapatellar approach group. There was no statistical difference between the two groups with regard to the patellar tilt and subluxation. We conclude that the modified subvastus approach is recommendable in primary TKA.
Résumé
Nous avons évalué la différence entre l’abord médial para patellaire et l’abord modifié subvastus lors de la mise en place d’une prothèse totale du genou. Nous avons apprécié le temps de récupération post-opératoire de l’extension active du genou et le degré de flexion de celui-ci à 10 jours, 6 semaines, 6, 12 et 36 mois. Nous avons également exploré les complications rotuliennes, notamment subluxations à 24 mois. Les patients ayant bénéficié d’un abord subvastus récupèrent une extension active plus précoce (en moyenne de 0,5 jours), contre 2,2 jours pour l’abord médian. L’amélioration de la flexion du genou est également meilleure à 10 jours post-opératoire dans ce groupe. Il n’y a pas de différence significative entre ces deux groupes en ce qui concerne les problèmes rotuliens. Nous pensons que l’abord subvastus est à recommander dans la mise en place d’une prothèse totale du genou.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The medial parapatellar approach has been used as the most general approach for total knee arthroplasty (TKA) until now and it provides a good surgical view. However, an incision in the vicinity of the patella may cause the impairment of blood supply to the patella [5, 10]. In addition, avascular necrosis caused by the impairment of blood supply induces patella fracture or anterior knee pain. The problem of the avascular necrosis is increased in the cases requiring lateral retinacular release. In addition, if the suture is too loose after the medial parapatellar approach, the problem of the mal-tracking of the patella may be induced.
The subvastus approach was introduced to English-speaking countries by Hofmann et al. [4]. This approach can conserve the blood supply to the patella, even if performed together with lateral retinacular release, and, in addition, it provides an adequate surgical view. Furthermore, since it preserves the quadricep’s muscle function, it reduces the problem of patella tracking.
However, the clinical usefulness of the traditional subvastus approach to the knee has been limited because it is difficult to evert the patella in muscular or obese patients [4, 6, 8]. We therefore devised the modified subvastus approach to overcome the disadvantages of the classical subvastus approach. Here, we attempt to evaluate the clinical and radiological difference between the modified subvastus approach and the medial parapatellar approach in TKA.
Materials and methods
The study was performed on 26 patients and 40 cases (bilateral 28 cases, unilateral 12 cases) who were diagnosed with osteoarthritis and who underwent their first TKA. There were 24 female patients, two male patients and the average follow up period was 58.4 months (range 36–78 months). The study population was divided randomly into two groups, who were allotted the medial parapatellar approach or the modified subvastus approach. The medial parapatellar approach was alloted to 19 cases and the modified subvastus approach was assigned to 21 cases. The age, gender and flexion range prior to surgery of the 40 cases in the two groups are shown in Table 1. In the bilateral TKA, in all patients, a different approach was used for the right and left knees. All surgery was performed by the same surgeon, the posterior cruciate ligament sacrificing type LCS design (Depuy™, USA) was used and patella resurfacing was not done, if the thickness of the patella was less than 21 mm or if the patellar cartilage was relatively good, in the cases without tenderness and crepitus in the patello-femoral area and in the cases with a good trochlea. In both groups, since the vertical skin incision in the midline of the patella was made, even patients who underwent bilateral TKA were unable to recognise the difference the two approach methods.
The subvastus approach technique is as follows. Skin incision was a vertical incision in the middle or slightly medial to the midline of the patella. Lateral incision or subcutaneous dissection was not performed, and, on the medial side, to facilitate the eversion of the patella, the fascia in the vicinity of muscles was lifted bluntly to the vicinity of the proximal in the medial vastus medialis muscles. Approximately 10 cm proximal to the adductor tubercle, the medial vastus medialis muscles was dissected bluntly from the medial intermuscular septum using fingers. This must be performed with caution so as not to injure the intermuscular septal branch or articular branch of the descending genicular artery passing through the intermuscular septum. To facilitate the eversion of the patella, in contrast to the medial parapatellar approach, the medial articular capsule was incised transversely from the upper patella, the tensed soft tissues, such as the plica and the fascia, were released by incision and the incision was made along the medial border of the patellar tendon (Fig. 1). However, in the cases with a limited range of joint movement or severe deformity and in extremely obese patients, eversion of the patella by the technique described above is difficult but, by applying a modified method that incises transversely approximately 1–2 cm of the insertion area of the vastus medialis muscle, the inversion of the patella could be preformed readily. Dissection of the medial vastus medialis muscle was reduced which was advantageous, as the length of the skin incision was shorter than the classic subvastus approach. In fact, during surgery, if the eversion of the patella could not be performed readily by the subvastus approach, the transverse incision of 1–2 cm of the tendon and the fascia area of the insertion of the medial vastus medialis muscle to the patella facilitates the eversion of the patella.
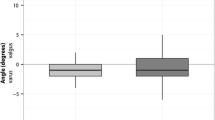
To view the femoral condyle, the knee joint was flexed slowly while the eversion of the patella was performed. If required, the eversion of the patella could be facilitated by incising the fascia of the medial vastus medialis muscle. After the insertion of the knee joint prosthesis, the patella was placed in its preoperative position, the patella tracking was evaluated and, in the modified subvastus approach, a well preserved extensor mechanism allows easy assessment of patellar tracking, without the necessity of the use of a towel clip etc. to stabilise the patella. During surgery, patella tracking appeared to be superior to the medial parapatellar approach group. The inversed V-shape incision in the joint capsule was restored by an absorbable stitch (Fig. 2) and it was not necessary to suture the medial vastus medialis muscle dissected from the intermuscular septum, the medial vastus medialis tendon was sutured firmly to the insertion area of the patella with No.1 Vicryl (Ethicon, Somerville) and the skin was sutured by a conventional method. After the placement of a Hemovac drain in the joint. Intravenous pain-controlled anaesthesia was administered post-operatively. The evaluation of patients was performed by an orthopaedic surgeon who had not participated in the surgery, and the range of movement of the knee joint of the active straight leg raising in the initial period and 10 days after surgery was assessed. The range of movement of the knee joint after 6 weeks, 6 months, 12 months and 3 years were assessed in the outpatient clinic. From 3 months after surgery, when the soft tissue was expected to be healed to some degree, the Merchant view was assessed in the outpatient clinic, and 3 years after surgery, on the Merchant view, the shift and tilt of the patella was measured. The shift and tilt of the patellar component after surgery was measured by the method described by Gomes et al. [3] (Fig. 3), and, in regard to the shift and tilt, 5 mm and less than 5°, respectively, were considered as normal.
a Patellar tilt and b patella shift were measured from the 45° Merchant view using the method of Gomes et al. [3]
After 1 year of follow up, loosening was evaluated on the antero-posterior and lateral radiographs, by applying the Knee Society roentgenographic evaluation. In the patients who underwent bilateral TKA, by evaluating the pain and the functional activity of the knee favoured by the patient, the subjective preference of the patient was evaluated. By performing an identical skin incision in the middle of the knee joint or slightly medial to the midline, both investigators and patients were unable to obtain information on the approach method used. The statistical analysis of the results of the two groups was performed by Student’s t-test. Power analysis was performed. The alpha, power, effect size for the range of motion and effect size for the shift or tilt were 0.05, 0.95, 5° and 2 mm, respectively. The required sample size was three cases and three controls for the range of motion and eight cases and eight controls for the shift or tilt. So, our sample size was large enough to compare the two groups.
Results
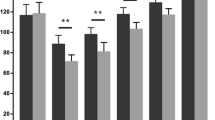
During the follow up, in all of the patients in both groups, inflammation or loosening of the component was not detected. In the group who underwent the modified subvastus approach, active straight leg raising of the patient was achieved in 0.5 days (±0.8) on average, which was faster than 2.2 days (±1.4) (p = 0.000), and at follow up at 10 days, 6 weeks, 6 months, 12 months and 3 years after surgery, the flexion range of the knee joint at 10 days after surgery was 99.2 ± 13.0 in the modified subvastus approach group, which was significantly superior to 87.3 ± 10.9, and, after that time, a statistically significant difference was not detected (Table 2). The shift and tilt of the knee joint were shown in Table 3 and a statistically significant difference between the two groups was not detected. In addition, although it is not an objective test, in the patients who underwent the bilateral TKA, at the last follow up, the subjective preference of the patient (post-operative pain, functional activity) resulted in 11 patients out of 14 patients preferring the knee joint treated by the modified subvastus approach.
Discussion
The modified subvastus approach that we performed in TKA allowed active straight leg raising in a shorter time and it showed superior flexion of the knee joint until 10 days after surgery compared to the conventional medial parapatellar approach. However, in regard to the flexion range 6 weeks after surgery and radiographical tests performed 3 years after surgery, the shift and tilt of the knee joint in the two groups were not statistically significantly different. Nevertheless, Matsueda and Gustilo [7] have reported that, in comparison with the medial parapatellar approach, the subvastus approach showed better results with the shift and tilt of the patella and also superior patellar tracking. In our study, the shift and tilt of the patella was not different between the two groups, and we consider that the balance of soft tissues was accurate so that no difference was detected. Numerous other studies have also reported the advantages of the subvastus approach, including the absence of impairment of the blood supply in the vicinity of the patella, the advantages of the decreased use of analgesics after surgery, the shortened admission period and the decreased blood loss during surgery [2, 4, 7, 9]. The problem of the lateral retinacular release in the medial parapatellar approach has been raised by Scuderi et al. [11], and, in the bone scan of patients who underwent these procedures, the incidence of cold patella with the decreased accumulation of isotope by 56.4% was observed. In the cases without the lateral retinacular incision, the incidence of cold patella has been reported to be 15% [11]. In the conventional medial parapatellar approach, through the incision of the vastus medialis tendon, the medial vastus medialis muscle is detached from the patella. Consequently, this includes incision of the articular branch of the descending genicular artery, as well as the upper and lower parts of the artery in the medial knee joint. More severe blood flow may be induced by excessive incision of the lateral, upper and lower blood vessels in the knee joint during the lateral retinacular incision.
Although the muscle strength of the vastus medialis muscle was not quantified during follow ups in our study, Fauré et al. [2] have reported that, in 20 patients, in comparison with the medial parapatellar approach, the muscle strength after surgery is stronger in the subvastus approach. Engh and Parks [1] have reported that, in TKA, a good result could be obtained by the midvastus approach. In such cases, a portion of the insertion area of the medial vastus medialis muscle to the patella remained intact; however, a substantial portion was detached from the patella, and, thus, the medial plexus was incised. In the modified subvastus approach, since 1–2 cm of the medial vastus medialis tendon was incised, it has the advantage that the dissection of the vastus medialis muscle from the intermuscular septum is reduced, blood vessels in the vicinity could be conserved well, muscle damage does not occur during surgery and the skin incision is relatively shorter than the original subvastus approach.
The cases to avoid using the modified subvastus approach are severely obese patients with significant patella baja, those who have undergone previous high tibial osteotomy, and patients who were previously treated with the medial parapatellar approach who should not considered [6].
Conclusions
By using this approach, in comparison to the conventional medial parapatellar approach, early active straight leg raising and a better range of motion of the knee flexion up to 10 days after surgery were detected. This shows that it promotes fast rehabilitation and early movement of patients after total knee arthroplasty (TKA), and we conclude that the modified subvastus approach is recommendable in primary TKA.
References
Engh GA, Parks NL (1998) Surgical technique of the midvastus arthrotomy. Clin Orthop Relat Res 351:270–274
Fauré BT, Benjamin JB, Lindsey B, Volz RG, Schutte D (1993) Comparison of the subvastus and paramedian surgical approaches in bilateral knee arthroplasty. J Arthroplasty 8:511–516
Gomes LS, Bechtold JE, Gustilo RB (1988) Patellar prosthesis positioning in total knee arthroplasty. A roentgenographic study. Clin Orthop Relat Res 236:72–81
Hofmann AA, Plaster RL, Murdock LE (1991) Subvastus (southern) approach for primary total knee arthroplasty. Clin Orthop Relat Res 269:70–77
Holtby RM, Grosso P (1996) Osteonecrosis and resorption of the patella after total knee replacement: a case report. Clin Orthop Relat Res 328:155–158
In Y, Kim JM, Choi NY, Kim SJ (2007) Large thigh girth is a relative contraindication for the subvastus approach in primary total knee arthroplasty. J Arthroplasty 22:569–573
Matsueda M, Gustilo RB (2000) Subvastus and medial parapatellar approaches in total knee arthroplasty. Clin Orthop Relat Res 371:161–168
Pagnano MW, Meneghini RM (2006) Minimally invasive total knee arthroplasty with an optimized subvastus approach. J Arthroplasty 21:22–26
Roysam GS, Oakley MJ (2001) Subvastus approach for total knee arthroplasty: a prospective, randomized, and observer-blinded trial. J Arthroplasty 16:454–457
Scapinelli R (1967) Blood supply of the human patella. Its relation to ischaemic necrosis after fracture. J Bone Joint Surg Br 49:563–570
Scuderi G, Scharf SC, Meltzer LP, Scott WN (1987) The relationship of lateral releases to patella viability in total knee arthroplasty. J Arthroplasty 2:209–214
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jung, Y.B., Lee, Y.S., Lee, E.Y. et al. Comparison of the modified subvastus and medial parapatellar approaches in total knee arthroplasty. International Orthopaedics (SICOT) 33, 419–423 (2009). https://doi.org/10.1007/s00264-007-0510-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-007-0510-y