Abstract
The primary goals of this critical literature review were to determine whether revision rates of primary total hip arthroplasty in patients with osteonecrosis differ based on the underlying associated risk factors and diagnoses, whether the outcomes of this procedure have improved over the past two decades, and to compare outcomes based on study level of evidence. A systematic literature review yielded 67 reports representing 3,277 hips in 2,593 patients who had a total hip arthroplasty for osteonecrosis of the femoral head. Stratification of outcomes by associated risk factors or diagnoses revealed significantly lower revision rates in patients with idiopathic disease, systemic lupus erythematosus, and after heart transplant, and significantly higher rates in patients with sickle cell disease, Gaucher disease, or after renal failure and/or transplant. There was a significant decrease in revision rates between patients operated upon before 1990 versus those in 1990 or later, with rates of 17% and 3%, respectively. The results for arthroplasties performed in 1990 or later were similar to those for all hips in publicly reported national joint registries. Certain risk factors were associated with higher revision rates in patients with osteonecrosis who were treated by total hip arthroplasty. However, most patients (82%) do not have these associated negative risk factors. Overall, this critical literature review provides evidence that osteonecrosis itself, or when associated with the most common risk factors and/or diagnoses, is not associated with poor outcomes in total hip arthroplasty.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Total hip arthroplasty is often the only available treatment to reduce pain and restore mobility in patients with post-collapse osteonecrosis of the femoral head. There have been a number of reports studying the outcomes of total hip arthroplasty for this disease, with a wide range of results. Historically, several authors described failure rates as high as 39% to 53% with first generation hip arthroplasty implant designs and techniques [15, 20, 82]. Some recent studies, reflecting third generation designs and techniques, have reported much lower revision rates [5, 42, 65, 79].
Patients with osteonecrosis are often grouped by associated risk factors and/or diseases. Some of the most common and well-described risk factors associated with this condition include corticosteroid use, excessive alcohol consumption, and smoking [63]. More recently, human immunodeficiency virus infection [47, 61] and organ transplantation, specifically heart, liver, and kidney transplants [8, 37, 58], have been found to be associated with osteonecrosis. Some risk factors might portend a better or worse outcome for total hip arthroplasty, and a few studies have reported increased failure rates with certain sub-populations (e.g. patients with sickle cell disease) [1, 7, 17, 54, 66, 68, 80, 88]. Other factors unique to osteonecrosis may further have contributed to the worse outcomes historically reported in the literature. The disorder is associated with altered bone remodelling, which may adversely affect the quality of the bone available for fixation of the implant [87]. In addition, osteonecrosis tends to affect younger individuals who commonly have a higher activity level as compared to older patients, potentially placing additional stress on the implant [24, 81]. Finally, in some patients, such as those exposed to high dose corticosteroids, the necrotic lesion may extend into the calcar, with the resultant dead bone providing inadequate support to prevent subsidence of the femoral component [62].
The primary purpose of this literature review was to pool the reported results of total hip arthroplasty for osteonecrosis to assess the overall revision rates to help us determine whether the disease itself is an independent risk factor for revision. Specific questions addressed were: (1) whether revision rates differ based on associated risk factors and/or diseases for osteonecrosis; (2) whether revision rates have changed over time, based on the year of index procedure; and (3) whether reported outcomes differ based on the level of evidence of the study. Where appropriate, an attempt was made to analyse whether there were differences in gender distribution, types of fixation, and length of follow-up that may have contributed to any differences in the results between these groups. An additional purpose was to compare the revision rates of more recently performed total hip arthroplasties for osteonecrosis (in 1990 or later) to the results for a variety of diagnoses reported in the larger national joint registries.
Materials and methods
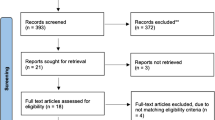
A comprehensive search was performed of the MEDLINE and EMBASE online databases for articles published up to December 31, 2007, using combinations of the initial terms 'total hip', 'arthroplasty', 'replacement', 'osteonecrosis', and 'avascular necrosis', and potentially relevant articles were identified. A review of the reference lists was made of the identified articles for any additional relevant studies. Three of the authors of our study (H.R.J., M.G.Z., M.A.M.) screened all the reports following our inclusion and exclusion criteria using the following guidelines: (1) inclusion of reports of patients treated with primary total hip arthroplasty for osteonecrosis using any combination of cemented, cementless, or hybrid component fixation, with outcomes measured by revision rates; (2) exclusion of any reports studying revision cases, those that contained previously published cases, or those surveying hemi-arthroplasty, bipolar arthroplasty, resurfacing, and/or thrust plate prostheses; (3) exclusion of studies that contained less than ten patients; (4) only studies with a reported follow-up were included, and (5) only the most recent study was included when the same patient cohort was reported in multiple follow-up articles.
Two of the authors of this study (H.R.J., M.G.Z.) extracted demographic data, types of fixation, associated risk factors and/or diagnoses, outcome data, study level of evidence, and years of index surgery into an electronic form using Microsoft Excel software (2003 version; Microsoft Corporation, Redmond, Washington), which was then combined into a single spreadsheet using the same software. The accuracy of the collected data was independently verified by three of the authors (D.R.M., M.A.M., M.S.M.). The specific demographic data collected included: number of patients, number of hips, age, gender, and follow-up period. The number of implants with cemented, cementless, hybrid, or reverse hybrid fixation was recorded for each report. Additional data included the presence or absence of any of the identified risk factors and/or associated diseases for osteonecrosis listed in Table 1. Outcome parameters included the number and percentage of hips that underwent revision surgery for any reason, that were scheduled for revision surgery, or that were recommended for revision surgery. Overall demographic, associated risk factor, and outcome data were averaged by weighting for the number of hips reported in each study, thereby preventing any one study from disproportionately influencing the overall results.
Sixty-seven studies were identified that reported on total hip arthroplasty for osteonecrosis of the femoral head that met our inclusion and exclusion criteria [1–3, 7, 9, 12–23, 25, 28–32, 34–36, 38–41, 43, 45, 46, 48–57, 59, 60, 64–66, 68–71, 73–80, 84, 86, 88–92], encompassing 3,277 hips in 2,593 patients. These reports were published between 1985 and 2007, with index arthroplasties performed between 1962 and 2006. The patients included in these reports had a mean age at index procedure of 44 years (range, 15–90 years), and were followed for a mean of eight years (range, 1–28 years). Men represented 60% of the patients and women 40%. Cemented fixation was used in 41% of the hips, cementless fixation in 51% of the hips, hybrid fixation in 7% of the hips, and reverse hybrid fixation in less than 1% of the hips (12 out of 3,277 hips). The most commonly reported associated risk factors and diseases were corticosteroid use for any reason (41%), steroid use for reasons other than organ transplant/failure or systemic lupus erythematosus (22%), and excessive alcohol use (19%). Twenty-one percent of patients had no identifiable risk factor and/or disease, and were classified as having idiopathic disease. The prevalence of various associated risk factors can be found in Table 1.
Thirty studies representing 1,273 hips (963 patients) contained sufficient information to stratify outcomes by associated risk factor [1–3, 7, 9, 15, 17, 18, 20, 21, 23, 25, 31, 36, 39, 41, 43, 45, 54, 56, 57, 66, 68, 70, 71, 73, 74, 76, 77, 80, 88], with index arthroplasties performed between 1970 and 2006. The demographic profile of the patients in these studies was similar to the overall patient population, with a mean age of 44 years (range, 16–90 years), and a mean follow-up of eight years (range, 1–26 years). Men represented 51% of the patients, and women 49%. Cemented fixation was used in 64% of the hips, cementless fixation in 33%, hybrid fixation in 3%, and reverse hybrid fixation in the remaining 1% of the hips. Insufficient information was available to make a statistical comparison between mean ages, gender distribution, and lengths of follow-up between subgroups of stratified patients and the whole population. Two corticosteroid groups were used in our analysis: one group included all patients with a history of corticosteroid use, including those with a history of organ failure and/or transplant or systemic lupus erythematosus; the second group included only those patients with a history of corticosteroid use for reasons other than the above co-morbidities. A comparison between these two groups was used to analyse whether risk for failure in patients with a history of corticosteroid use differed based on the underlying condition. A full description of revision rates stratified by risk factors can be found in Table 2.
All studies that met our inclusion and exclusion criteria were grouped into those with index arthroplasties performed before 1990, and those performed in 1990 and later. Studies were stratified in this manner, because in the 1980s there were important changes in surgical techniques and prosthesis design for total hip arthroplasty. Specifically, second-generation cementing techniques were adopted and reported by a number of investigators during this decade, and circumferentially proximally-coated cementless stems were made available. Both of these advances were reported to substantially reduce the incidence of femoral component loosening or revision [4, 6, 67, 85]. Most investigators had adopted these innovations into their surgical practice by the year 1990. Stratifying studies around this year was designed to allow us to evaluate the influence of modern techniques and designs on the outcomes of total hip arthroplasty for osteonecrosis. Some reports included patients operated upon both before and after 1990. In these reports, we determined when each patient’s procedure was performed, assigning them to the appropriate group. When this was not possible, the report was excluded from our temporal review of hip revision rates. Four reports did not contain sufficient information for stratification [22, 51, 52, 91]; these studies were included in our overall review, but were excluded from the analyses of differences before and in or after 1990. Twenty-eight studies included index arthroplasty dates prior to 1990 [1, 3, 7, 9, 15, 17, 19, 20, 28, 31, 32, 34, 36, 39, 43, 45, 50, 53, 57, 59, 60, 66, 68, 71, 73, 74, 76, 77], representing 1,209 hips in 944 patients. The patients in this group had a mean age of 45 years (range, 16–90 years), with men representing 49% of the patients and women 51%. Cemented fixation was used in 71% of the hips, cementless fixation in 28%, and reverse hybrid fixation in the remaining 1% of the hips. Nine studies included index arthroplasty dates in 1990 or later [13, 40, 48, 55, 56, 64, 65, 70, 79], representing 458 hips in 395 patients. The patients in this group had a mean age of 45 years (range, 15–77 years). Men represented 71% of the patients and women 29%. Cementless fixation was used in 89% of the hips, and hybrid fixation in the remaining 9% of the hips. No patients were treated with fully cemented prostheses. Some variability was seen in the prevalence of various risk factors and/or diseases between the two groups. The most commonly reported associated factors in patients operated in 1990 or later were idiopathic disease (35%), ethanol abuse (26%), and corticosteroid use (20%). In comparison, in patients operated prior to 1990, these factors had a prevalence of 19%, 11%, and 19%, respectively. A complete description of demographic findings can be found in Table 3.
Studies were grouped by level of evidence. High level of evidence studies (levels I and II) are widely accepted as providing higher-quality evidence for the outcomes of treatments and/or interventions while minimising bias, owing to their prospective, randomised, and controlled design. In contrast, lower level studies (levels of evidence III and IV) are either retrospective in design or do not include a comparison or control group, and are generally accepted to be more susceptible to bias and error. Grouping studies by level of evidence was made to allow the authors to (1) evaluate whether differences existed in reported outcomes based on study design, and (2) assess the overall quality of the evidence for the outcomes of primary total hip arthroplasty in patients who had osteonecrosis as reported in the orthopaedic literature. Thirty-four studies encompassing 1,599 hips had a level of evidence of IV, 32 studies encompassing 1,647 hips had a level of evidence of III, one study encompassing 31 hips had a level of evidence of II, and no studies had a level of evidence of I. This precluded a comparison of prospective randomised trials to case series reports, but allowed comparison of reports with levels of evidence III and IV. The demographic profiles showed similar weighted mean ages and gender distribution in both level III and level IV study groups.
The most recent reports of the Canadian [10], English and Welsh [26], Norwegian [27], Danish [72], Swedish [44], Australian [33], and New Zealand [11] joint registries were reviewed to determine the six-year and ten-year survival of primary hip arthroplasties. Only the Danish, Swedish, Australian, and New Zealand reports contained sufficient data and/or follow-up time to extract this information. Data was extracted for all primary total hip arthroplasties, and those performed in patients who had osteoarthritis only. None of the reports presented separate outcomes for patients who had a diagnosis of osteonecrosis. The outcomes were then compared to the results of our review of the nine studies encompassing patients operated in 1990 or later. A comparison of reported registry results was not made to the total osteonecrosis patient population of all 67 reviewed studies because, although this group had a mean follow-up of eight years, the range of follow-ups had a large variation (between one and 26 years), making a meaningful comparison impossible.
To answer the specific questions posed in this study, a review of the collected data was performed to determine the overall demographic profile of the combined patient cohort, the incidence of the previously defined associated risk factors and diseases, and the overall rate of revisions. Stratification of patients based on age or gender was not possible. However, to minimise any possible study bias, a review was performed concerning whether these factors differed significantly between: (1) the overall patient population and the subset that had outcome data stratified by associated risk factors and/or diagnoses shown in Table 1; (2) patients who were operated upon pre or post-1990; and (3) studies with differing levels of evidence. In addition, a review of whether significant differences existed in the types of fixation used in the groups described above was performed. Stratification of the reports by these groups was performed, with a separate review made of all of the variables (demographic data, revision rates, associated risk factors and diagnoses, and follow-up times) to search for any significant differences in these population characteristics that might influence the results.
Statistical methods
Averaging, weighting, and comparative analyses was performed using SigmaStat statistical software (version 3.00; SPSS Inc., Chicago, Illinois) and the Microsoft Excel spreadsheet program (2003 version; Microsoft Corporation, Redmond, Washington) using chi-square, Student’s t-test, and logistical regression analyses where appropriate.
Results
Total hip arthroplasties performed after 1990 revealed a survival rate of 97% at a mean follow-up time of six years. This is in contrast to a survival rate of 83% at a mean follow-up of nine years for total hip arthroplasties performed before 1990. Overall, the survival rate for all the primary hip arthroplasties included in this analysis was 87%, with revision surgery performed or indicated in 13% of hips (range in reports, 0–50%).
Stratification of revision rates in all reviewed patients with osteonecrosis by associated risk factors and/or diseases revealed revision rates significantly higher than the overall rate in patients with sickle cell disease (p < 0.001), renal failure and/or transplant (p = 0.002) and Gaucher disease (p = 0.013). The total number of osteonecrosis patients with risk factors and/or diseases who had revision rates significantly higher than the overall rate represented 18% of the total number of patients who were treated by primary total hip arthroplasty for osteonecrosis. Therefore, over 80% of patients with osteonecrosis did not have a higher risk of failure as compared to the overall mean rate. Revision rates were significantly lower than the overall mean rate for three risk factors: systemic lupus erythematosus (p < 0.001), idiopathic disease (p = 0.005), and heart transplant (p = 0.027). Revision rates for all patients with a history of corticosteroid use were similar to the overall population (p = 0.997), but those with a diagnosis of systemic lupus erythematosus or after organ failure and/or transplant had significant differences in revision rates as compared to the overall group, while the patients who had a history of corticosteroid use for other indications did not (p = 0.952).
A significant difference was found in total hip arthroplasty revision rates over time (p < 0.0001), with an odds ratio of 5.7 for studies with index arthroplasty performed prior to 1990 as compared to those performed in 1990 or later. Normalisation of rates revealed revisions per 100 observed implant years of 1.9 and 0.5 (odds ratio = 3.8) for patients with index surgery prior to and after 1990, respectively. The overall total hip arthroplasty survival rate for index procedure performed in 1990 or later was 97%, with revision surgery performed or indicated in 3% of hips (range in studies, 0–7%); whereas the overall total hip arthroplasty survival rate in patients with osteonecrosis and index procedures performed prior to 1990 was 83% at final follow-up, with revision surgery performed or indicated in 17% of hips (range in studies, 0–50%). Insufficient information was available to make a statistical comparison between the mean age and length of follow-up of the two groups, but significant differences were found in gender distribution (p < 0.001) and type of fixation (p < 0.001), with a higher proportion of men and more frequent use of cementless fixation seen in osteonecrosis patients operated upon in 1990 or later.
In studies with levels of evidence of III and IV, the revision rates were 13% for both, at mean follow-ups of nine years and seven years, respectively. There was a significant difference in type of fixation (p < 0.001), with more hybrid and less cementless fixation in level IV studies. Only one study with a level of evidence of I or II was identified [55].
A review of national joint replacement registries revealed six-year survivorship of between 95% and 97% for all primary total hip arthroplasties for a variety of diagnoses combined, and between 97% and 98% for arthroplasties performed in patients who had osteoarthritis. These findings are similar to the 97% survival at a mean follow-up of six years found in our analysis for arthroplasties performed for osteonecrosis in 1990 or later. The results are summarised in Table 4.
Discussion
While total hip arthroplasty has been the definitive treatment for end-stage osteonecrosis of the hip, marked by collapse of the femoral head, published outcomes of this treatment have varied greatly. Some reports have noted high failure rates, while others have reported more optimistic outcomes. Because of this large variation in results, we decided to pool the published results of primary total hip arthroplasty for osteonecrosis to ascertain overall outcomes for this procedure, finding an overall revision rate of 13% over 3,277 hips at a weighted mean follow-up of eight years (range, 1–28 years). Fortunately, a significant reduction in the rate of revisions in patients operated upon in 1990 or later, as compared to those operated prior to that year, was found. This may be a reflection of the fact that only 458 hips were operated after 1990 and 89% of them underwent cemented fixation of the femoral component.
One of the limitations of this report is that failures examined were based on component revision rates, but not on an assessment of clinically poor results or radiographic failures. However, because clinical or radiographic failures that are sufficiently severe will often result in recommended component revision, the authors believe that revision rates allow an excellent comparison of the relative success of total hip arthroplasty in the groups compared in this report. Secondly, there were other differences that were found for certain demographic and surgical factors such as age, type of implant fixation, and length of follow-up between patient sub-populations that were compared in this report, and it is possible that these differences influenced the revision rates in the comparison groups. Furthermore, the prevalence of negative risk factors (sickle cell disease, renal failure and/or transplant, and Gaucher disease) was significantly higher in patients with index arthroplasties prior to 1990 compared to those in 1990 or later (31% versus 1%, respectively; p < 0.001), which may be responsible for some of the differences in revision rates found between these two groups. However, when all the patients with negative risk factors were excluded, the revision rates in patients operated upon prior to 1990 was 12%, which remains considerably higher compared to the 3% rate in all patients with index arthroplasties in 1990 or later. There was a lack of prospective, randomised studies which made it impossible to analyse any of the factors evaluated in this report using traditional meta-analysis methodology and to perform a rigorous statistical evaluation of the outcomes of this procedure. However, the authors believe that this synthesis nevertheless confirms suspicions about the improving outcomes of the use of total hip arthroplasty for the treatment of osteonecrosis of the femoral head. It is hoped that this study will highlight the paucity of high-quality evidence studies regarding this treatment modality, and encourage the orthopaedic community to evaluate this condition more thoroughly.
The last few decades have been marked by advances in the understanding of osteonecrosis, and consequently by improvements in treatments designed to address the specific pathological elements of this disorder. For total hip arthroplasty, the past two decades have been marked by the widespread implementation of second and third-generation implant designs, with some authors demonstrating their positive influence on survivorship of total hip implants in patients with osteonecrosis [75]. For example, Steinberg et al. recently reviewed the outcomes for total hip arthroplasties performed in patients with osteonecrosis (203 hips) and degenerative joint disease (300 hips), and found a higher overall failure rate in patients who had osteonecrosis (10% versus 4%) at a mean follow-up of 14 years (range, 12–15 years) [83]. However, when the authors limited their analysis to patients who were treated with a newer-generation uncemented acetabular cup, they found only one revision in 111 hips with osteonecrosis, and no failures in 124 hips with degenerative joint disease. When stratified by year of surgery, our study had similar findings to those described by Steinberg et al., with a revision rate of 3% in patients who had their index primary total hip arthroplasty performed in 1990 and later (representing primarily second-generation cementless components), compared with a revision rate of 17% in hips operated upon before 1990.
Although osteonecrosis is not an inherent predictor of less favourable outcomes for primary total hip arthroplasty, certain risk factors are associated with higher or lower revision rates. It appears that patients with sickle cell disease, renal failure and/or transplant, and Gaucher disease have significantly higher revision rates when compared to the overall population of patients treated with primary total hip arthroplasty for osteonecrosis. However, 82% of patients in this analysis did not have any of these diagnoses, suggesting that for the majority of patients, their associated risk factors and/or diagnoses do not predict poorer outcomes after total hip arthroplasty.
Although patients who had renal failure and/or transplant, heart transplant, and systemic lupus erythematosus all had a history of corticosteroid use, there were significant differences in failure rates between these groups. It is possible that the somewhat shorter mean follow-up time of the heart transplant patients (three years), as well as the typically lower activity level of this population, was responsible for the lower failure rates seen in our study. Renal transplant patients are typically treated with much higher doses of corticosteroids compared to other populations, and this might have a greater adverse impact on bone metabolism, contributing to the higher failure rates seen for this group. However, this is based on conjecture only, and an analysis of the underlying causes of variations in failure rates is beyond the scope of this study.
Overall, this literature review provides evidence that the failure rates of primary total hip arthroplasties in patients with osteonecrosis were similar to the overall rates found in the general population treated with these implants. Certain risk factors appear to portend worse outcomes for patients with osteonecrosis (such as renal failure and/or transplant and sickle cell disease), but these were found in a minority of patients. In contrast, over 80% of patients did not have any associated risk factors and/or diagnoses which put them at significantly higher risk for revision. In summary, it appears that osteonecrosis per se may not a predictor of poor outcomes for total hip arthroplasty.
References
Acurio MT, Friedman RJ (1992) Hip arthroplasty in patients with sickle-cell haemoglobinopathy. J Bone Jt Surg Br 74:367–371
Al-Mousawi F, Malki A, Al-Aradi A, Al-Bagali M, Al-Sadadi A, Booz MM (2002) Total hip replacement in sickle cell disease. Int Orthop 26:157–161. doi:10.1007/s00264-002-0337-5
Alpert B, Waddell JP, Morton J, Bear RA (1992) Cementless total hip arthroplasty in renal transplant patients. Clin Orthop Relat Res 284:164–169
Archibeck MJ, Berger RA, Jacobs JJ, Quigley LR, Gitelis S, Rosenberg AG, Galante JO (2001) Second-generation cementless total hip arthroplasty. Eight to eleven-year results. J Bone Jt Surg Am 83:1666–1673
Baek SH, Kim SY (2008) Cementless total hip arthroplasty with alumina bearings in patients younger than fifty with femoral head osteonecrosis. J Bone Jt Surg Am 90:1314–1320
Barrack RL, Mulroy RD Jr, Harris WH (1992) Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Jt Surg Br 74:385–389
Bishop AR, Roberson JR, Eckman JR, Fleming LL (1988) Total hip arthroplasty in patients who have sickle-cell hemoglobinopathy. J Bone Jt Surg Am 70:853–855
Bradbury G, Benjamin J, Thompson J, Klees E, Copeland J (1994) Avascular necrosis of bone after cardiac transplantation. Prevalence and relationship to administration and dosage of steroids. J Bone Jt Surg Am 76:1385–1388
Brinker MR, Rosenberg AG, Kull L, Galante JO (1994) Primary total hip arthroplasty using noncemented porous-coated femoral components in patients with osteonecrosis of the femoral head. J Arthroplasty 9:457–468
Canadian Joint Replacement Registry (2007) Annual report. Canadian Institute for Health Information, Ottawa, Canada
Canterbury District Health Board Ltd. (2008) NZ national joint registry. http://www.cdhb.govt.nz/njr/. Accessed October 30 2008
Cebesoy O, Erdemli B, Kose KC, Guzel B, Cetin I (2006) Midterm results of total hip replacement in osteonecrosis of the hip joint. Acta Orthop Traumatol Turc 40:301–306
Celebi L, Muratli HH, Aksahin E, Yagmurlu MF, Yuksel HY, Bicimoglu A (2006) Cementless total hip arthroplasty in patients with avascular necrosis of the femoral head. Acta Orthop Traumatol Turc 40:105–110
Chan YS, Shih CH (2000) Bipolar versus total hip arthroplasty for hip osteonecrosis in the same patient. Clin Orthop Relat Res 379:169–177
Chandler HP, Reineck FT, Wixson RL, McCarthy JC (1981) Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Jt Surg Am 63:1426–1434
Chen YW, Chang JK, Huang KY, Lin GT, Lin SY, Huang CY (1999) Hip arthroplasty for osteonecrosis in patients with systemic lupus erythematosus. Kaohsiung J Med Sci 15:697–703
Cheng EY, Klibanoff JE, Robinson HJ, Bradford DS (1995) Total hip arthroplasty with cement after renal transplantation. Long-term results. J Bone Jt Surg Am 77:1535–1542
Chiu KH, Shen WY, Ko CK, Chan KM (1997) Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. A comparison with other diagnoses. J Arthroplasty 12:683–688
Chiu KY, Ng TP, Tang WM, Poon KC, Ho WY, Yip D (2001) Charnley total hip arthroplasty in Chinese patients less than 40 years old. J Arthroplasty 16:92–101. doi:10.1054/arth.2001.19156
Cornell CN, Salvati EA, Pellicci PM (1985) Long-term follow-up of total hip replacement in patients with osteonecrosis. Orthop Clin North Am 16:757–769
D’Antonio JA, Capello WN, Manley MT, Feinberg J (1997) Hydroxyapatite coated implants. Total hip arthroplasty in the young patient and patients with avascular necrosis. Clin Orthop Relat Res 344:124–138
Davis ET, McKee MD, Waddell JP, Hupel T, Schemitsch EH (2006) Total hip arthroplasty following failure of free vascularized fibular graft. J Bone Jt Surg Am 88(Suppl 3):110–115. doi:10.2106/JBJS.F.00771
Deo S, Gibbons CL, Emerton M, Simpson AH (1995) Total hip replacement in renal transplant patients. J Bone Jt Surg Br 77:299–302
Dorr LD, Takei GK, Conaty JP (1983) Total hip arthroplasties in patients less than forty-five years old. J Bone Jt Surg Am 65:474–479
Dudkiewicz I, Covo A, Salai M, Israeli A, Amit Y, Chechik A (2004) Total hip arthroplasty after avascular necrosis of the femoral head: does etiology affect the results? Arch Orthop Trauma Surg 124:82–85. doi:10.1007/s00402-003-0630-9
Emsley D, Martin J, Newell C, Pickford M, Royall M, Swanson M, van der Meulen J, Charman S, Gregg P, Porter M, Tucker K, Howard P (2008) 5th annual report. National Joint Registry for England and Wales, Hemel Hempstead, UK
Furnes O, Havelin LI, Espehaug B, Steindal K, Sørås TE (2008) Report 2008. Centre of Excellence of Joint Replacements, Bergen, Norway
Fyda TM, Callaghan JJ, Olejniczak J, Johnston RC (2002) Minimum ten-year follow-up of cemented total hip replacement in patients with osteonecrosis of the femoral head. Iowa Orthop J 22:8–19
Fye MA, Huo MH, Zatorski LE, Keggi KJ (1998) Total hip arthroplasty performed without cement in patients with femoral head osteonecrosis who are less than 50 years old. J Arthroplasty 13:876–881
Garino JP, Steinberg ME (1997) Total hip arthroplasty in patients with avascular necrosis of the femoral head: a 2- to 10-year follow-up. Clin Orthop Relat Res 334:108–115
Goffin E, Baertz G, Rombouts JJ (2006) Long-term survivorship analysis of cemented total hip replacement (THR) after avascular necrosis of the femoral head in renal transplant recipients. Nephrol Dial Transplant 21:784–788. doi:10.1093/ndt/gfi233
Gonzalez MH, Ortinau ET, Buonanno W, Prieto J (1997) Cementless total hip arthroplasty in patients with advanced avascular necrosis. J South Orthop Assoc 6:162–168
Graves S, Davidson D, de Steiger R, Tomkins A, Ryan P, Griffith L, McDermott B, Pratt N, Miller L, Stanford T (2008) National Joint Replacement Registry annual report. Adelaide, Australia
Grecula MJ, Grigoris P, Schmalzried TP, Dorey F, Campbell PA, Amstutz HC (1995) Endoprostheses for osteonecrosis of the femoral head. A comparison of four models in young patients. Int Orthop 19:137–143
Gualtieri G, Vellani G, Dallari D, Catamo L, Gualtieri I, Fatone F, Bonomini V (1995) Total hip arthroplasty in patients dialyzed or with renal transplants. Chir Organi Mov 80:139–145
Hanssen AD, Cabanela ME, Michet CJ Jr (1987) Hip arthroplasty in patients with systemic lupus erythematosus. J Bone Jt Surg Am 69:807–814
Harrington KD, Murray WR, Kountz SL, Belzer FO (1971) Avascular necrosis of bone after renal transplantation. J Bone Jt Surg Am 53:203–215
Hartley WT, McAuley JP, Culpepper WJ, Engh CA Jr, Engh CA Sr (2000) Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. J Bone Jt Surg Am 82:1408–1413
Huo MH, Salvati EA, Browne MG, Pellicci PM, Sculco TP, Johanson NA (1992) Primary total hip arthroplasty in systemic lupus erythematosus. J Arthroplasty 7:51–56
Ince A, Lermann J, Gobel S, Wollmerstedt N, Hendrich C (2006) No increased stem subsidence after arthroplasty in young patients with femoral head osteonecrosis: 41 patients followed for 1–9 years. Acta Orthop 77:866–870. doi:10.1080/17453670610013141
Ito H, Matsuno T, Hirayama T, Tanino H, Minami A (2007) Health-related quality of life in patients with systemic lupus erythematosus after medium to long-term follow-up of hip arthroplasty. Lupus 16:318–323. doi:10.1177/0961203307077989
Johnsen SP, Sorensen HT, Lucht U, Soballe K, Overgaard S, Pedersen AB (2006) Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms. A nationwide Danish follow-up study including 36,984 patients. J Bone Jt Surg Br 88:1303–1308. doi:10.1302/0301-620X.88B10.17399
Kantor SG, Huo MH, Huk OL, Salvati EA (1996) Cemented total hip arthroplasty in patients with osteonecrosis. A 6-year minimum follow-up study of second-generation cement techniques. J Arthroplasty 11:267–271
Kärrholm J, Garellick G, Rogmark C, Herberts P (2008) Annual report 2007. Swedish Hip Arthroplasty Register, Mölndal, Sweden
Katz RL, Bourne RB, Rorabeck CH, McGee H (1992) Total hip arthroplasty in patients with avascular necrosis of the hip. Follow-up observations on cementless and cemented operations. Clin Orthop Relat Res 281:145–151
Kawasaki M, Hasegawa Y, Sakano S, Masui T, Ishiguro N (2005) Total hip arthroplasty after failed transtrochanteric rotational osteotomy for avascular necrosis of the femoral head. J Arthroplasty 20:574–579. doi:10.1016/j.arth.2005.01.018
Keruly JC, Chaisson RE, Moore RD (2001) Increasing incidence of avascular necrosis of the hip in HIV-infected patients. J Acquir Immune Defic Syndr 28:101–102
Kim YG, Kim SY, Kim SJ, Park BC, Kim PT, Ihn JC (2005) The use of cementless expansion acetabular component and an alumina-polyethylene bearing in total hip arthroplasty for osteonecrosis. J Bone Jt Surg Br 87:776–780. doi:10.1302/0301-620X.87B6.15380
Kim YG, Kim SY, Park BC, Kim PT, Ihn JC, Kim ID (2005) Uncemented Harris-Galante total hip arthroplasty in patients with osteonecrosis of the femoral head. A 10–16-year follow-up study. Acta Orthop 76:42–48. doi:10.1080/00016470510030300
Kim YH, Kim JS, Cho SH (1999) Primary total hip arthroplasty with a cementless porous-coated anatomic total hip prosthesis: 10- to 12-year results of prospective and consecutive series. J Arthroplasty 14:538–548
Kim YH, Oh JH, Oh SH (1995) Cementless total hip arthroplasty in patients with osteonecrosis of the femoral head. Clin Orthop Relat Res 320:73–84
Kim YH, Oh SH, Kim JS, Koo KH (2003) Contemporary total hip arthroplasty with and without cement in patients with osteonecrosis of the femoral head. J Bone Jt Surg Am 85:675–681
Kirschenbaum IH, Vernace JV, Booth RE Jr, Balderston RA, Rothman RH (1991) Total hip arthroplasty for osteonecrosis. Semin Arthroplasty 2:234–240
Lebel E, Itzchaki M, Hadas-Halpern I, Zimran A, Elstein D (2001) Outcome of total hip arthroplasty in patients with Gaucher disease. J Arthroplasty 16:7–12. doi:10.1054/arth.2001.19162
Lee SB, Sugano N, Nakata K, Matsui M, Ohzono K (2004) Comparison between bipolar hemiarthroplasty and THA for osteonecrosis of the femoral head. Clin Orthop Relat Res 424:161–165
Leon JL, Resines C, Zafra A (2007) Total hip arthroplasty in heart transplant patients. Acta Orthop Belg 73:720–728
Lieberman JR, Fuchs MD, Haas SB, Garvin KL, Goldstock L, Gupta R, Pellicci PM, Salvati EA (1995) Hip arthroplasty in patients with chronic renal failure. J Arthroplasty 10:191–195
Lieberman JR, Scaduto AA, Wellmeyer E (2000) Symptomatic osteonecrosis of the hip after orthotopic liver transplantation. J Arthroplasty 15:767–771. doi:10.1054/arth.2000.6635
Lins RE, Barnes BC, Callaghan JJ, Mair SD, McCollum DE (1993) Evaluation of uncemented total hip arthroplasty in patients with avascular necrosis of the femoral head. Clin Orthop Relat Res 297:168–173
Lo NN, Tan JS, Tan SK, Vathsala A (1992) Results of total hip replacement in renal transplant recipients. Ann Acad Med Singapore 21:694–698
Mahoney CR, Glesby MJ, DiCarlo EF, Peterson MG, Bostrom MP (2005) Total hip arthroplasty in patients with human immunodeficiency virus infection: pathologic findings and surgical outcomes. Acta Orthop 76:198–203
Mont MA, Hungerford DS (1995) Non-traumatic avascular necrosis of the femoral head. J Bone Jt Surg Am 77:459–474
Mont MA, Jones LC, Hungerford DS (2006) Nontraumatic osteonecrosis of the femoral head: ten years later. J Bone Jt Surg Am 88:1117–1132. doi:10.2106/JBJS.E.01041
Mont MA, Rajadhyaksha AD, Hungerford DS (2001) Outcomes of limited femoral resurfacing arthroplasty compared with total hip arthroplasty for osteonecrosis of the femoral head. J Arthroplasty 16:134–139
Mont MA, Seyler TM, Plate JF, Delanois RE, Parvizi J (2006) Uncemented total hip arthroplasty in young adults with osteonecrosis of the femoral head: a comparative study. J Bone Jt Surg Am 88(Suppl 3):104–109. doi:10.2106/JBJS.F.00451
Moran MC, Huo MH, Garvin KL, Pellicci PM, Salvati EA (1993) Total hip arthroplasty in sickle cell hemoglobinopathy. Clin Orthop Relat Res 294:140–148
Mulroy RD Jr, Harris WH (1990) The effect of improved cementing techniques on component loosening in total hip replacement. An 11-year radiographic review. J Bone Jt Surg Br 72:757–760
Murzic WJ, McCollum DE (1994) Hip arthroplasty for osteonecrosis after renal transplantation. Clin Orthop Relat Res 299:212–219
Nich C, Courpied JP, Kerboull M, Postel M, Hamadouche M (2006) Charnley-Kerboull total hip arthroplasty for osteonecrosis of the femoral head a minimal 10-year follow-up study. J Arthroplasty 21:533–540. doi:10.1016/j.arth.2005.05.028
Nich C, Sariali el H, Hannouche D, Nizard R, Witvoet J, Sedel L, Bizot P (2003) Long-term results of alumina-on-alumina hip arthroplasty for osteonecrosis. Clin Orthop Relat Res 417:102–111. doi:10.1097/01.blo.0000096820.67494.bf
Ortiguera CJ, Pulliam IT, Cabanela ME (1999) Total hip arthroplasty for osteonecrosis: matched-pair analysis of 188 hips with long-term follow-up. J Arthroplasty 14:21–28
Overgaard S, Pedersen AB (2008) Årsrapport 2008. Danish hip arthroplasty register, Århus, Denmark
Phillips FM, Pottenger LA, Finn HA, Vandermolen J (1994) Cementless total hip arthroplasty in patients with steroid-induced avascular necrosis of the hip. A 62-month follow-up study. Clin Orthop Relat Res 303:147–154
Piston RW, Engh CA, De Carvalho PI, Suthers K (1994) Osteonecrosis of the femoral head treated with total hip arthroplasty without cement. J Bone Joint Surg Am 76:202–214
Radl R, Egner S, Hungerford M, Rehak P, Windhager R (2005) Survival of cementless femoral components after osteonecrosis of the femoral head with different etiologies. J Arthroplasty 20:509–515. doi:10.1016/j.arth.2004.09.050
Ritter MA, Helphinstine J, Keating EM, Faris PM, Meding JB (1997) Total hip arthroplasty in patients with osteonecrosis. The effect of cement techniques. Clin Orthop Relat Res 338:94–99
Saito S, Saito M, Nishina T, Ohzono K, Ono K (1989) Long-term results of total hip arthroplasty for osteonecrosis of the femoral head. A comparison with osteoarthritis. Clin Orthop Relat Res 244:198–207
Schneider W, Knahr K (2004) Total hip replacement in younger patients: survival rate after avascular necrosis of the femoral head. Acta Orthop Scand 75:142–146. doi:10.1080/00016470412331294385
Seyler TM, Bonutti PM, Shen J, Naughton M, Kester M (2006) Use of an alumina-on-alumina bearing system in total hip arthroplasty for osteonecrosis of the hip. J Bone Jt Surg Am 88(Suppl 3):116–125. doi:10.2106/JBJS.F.00775
Shrader MW, Schall D, Parvizi J, McCarthy JT, Lewallen DG (2006) Total hip arthroplasty in patients with renal failure: a comparison between transplant and dialysis patients. J Arthroplasty 21:324–329. doi:10.1016/j.arth.2005.07.008
Solacoff D, Mont MA, Krackow KA (1993-1994) Uncemented total hip arthroplasty in patients less than 45 years with avascular necrosis. Orthop Trans 17:1085
Stauffer RN (1982) Ten-year follow-up study of total hip replacement. J Bone Jt Surg Am 64:983–990
Steinberg ME, Lai M, Garino JP, Ong A, Wong KL (2008) A comparison between total hip replacement for osteonecrosis and degenerative joint disease. Orthopedics 31:360
Stulberg BN, Singer R, Goldner J, Stulberg J (1997) Uncemented total hip arthroplasty in osteonecrosis: a 2- to 10-year evaluation. Clin Orthop Relat Res 334:116–123
Tankersley WS, Mont MA, Hungerford DS (1997) A second-generation cementless hip prosthesis: improved results over the first-generation prosthesis. Am J Orthop 26:839–844
Taylor AH, Shannon M, Whitehouse SL, Lee MB, Learmonth ID (2001) Harris Galante cementless acetabular replacement in avascular necrosis. J Bone Jt Surg Br 83:177–182
Tingart M, Beckmann J, Opolka A, Matsuura M, Schaumburger J, Grifka J, Grassel S (2009) Analysis of bone matrix composition and trabecular microarchitecture of the femoral metaphysis in patients with osteonecrosis of the femoral head. J Orthop Res. doi:10.1002/jor.20873
Toomey HE, Toomey SD (1998) Hip arthroplasty in chronic dialysis patients. J Arthroplasty 13:647–652
Wroblewski BM, Siney PD, Fleming PA (2005) Charnley low-frictional torque arthroplasty for avascular necrosis of the femoral head. J Arthroplasty 20:870–873. doi:10.1016/j.arth.2005.02.006
Xenakis TA, Beris AE, Malizos KK, Koukoubis T, Gelalis J, Soucacos PN (1997) Total hip arthroplasty for avascular necrosis and degenerative osteoarthritis of the hip. Clin Orthop Relat Res 341:62–68
Xenakis TA, Gelalis J, Koukoubis TA, Zaharis KC, Soucacos PN (2001) Cementless hip arthroplasty in the treatment of patients with femoral head necrosis. Clin Orthop Relat Res 386:93–99
Zangger P, Gladman DD, Urowitz MB, Bogoch ER (2000) Outcome of total hip replacement for avascular necrosis in systemic lupus erythematosus. J Rheumatol 27:919–923
Author information
Authors and Affiliations
Corresponding author
Additional information
Level of evidence: Level IV therapeutic
Rights and permissions
About this article
Cite this article
Johannson, H.R., Zywiel, M.G., Marker, D.R. et al. Osteonecrosis is not a predictor of poor outcomes in primary total hip arthroplasty: a systematic literature review. International Orthopaedics (SICOT) 35, 465–473 (2011). https://doi.org/10.1007/s00264-010-0979-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-0979-7