Abstract
In a previous study, the authors reported the clinical and radiological results of Duchenne muscular dystrophy (DMD) scoliosis surgery in 14 patients with a low FVC of <30%. The purpose of this study was to determine if surgery improved function and QOL in these patients. Furthermore, the authors assessed the patients’ and parents’ satisfaction. %FVC increased in all patients after preoperative inspiratory muscle training. Scoliosis surgery in this group of patients presented no increased risk of major complications. All-screw constructions and fusion offered the ability to correct spinal deformity in the coronal and pelvic obliquity initially, intermediate and long-term. All patients were encouraged to continue inspiratory muscle training after surgery. The mean rate of %FVC decline after surgery was 3.6% per year. Most patients and parents believed scoliosis surgery improved their function, sitting balance and quality of life even though patients were at high risk for major complications. Their satisfaction was also high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Posterior spinal fusion and instrumentation for scoliosis in Duchenne muscular dystrophy (DMD) has been aimed at maximising function and improving patients’ quality of life [1–5, 7, 10, 13, 15–18, 20, 22]. This surgery has been widely accepted as an optimal procedure to prevent progression of scoliosis and maintain upright and comfortable sitting balance [1–5, 7, 10, 13, 15–18, 20, 22]. Although many studies have reported the results of scoliosis surgery in patients with DMD, most studies have lacked a postoperative evaluation of the quality of life (QOL) of the patients and the overall effects on the parents. The majority of studies have reported only data on changes in scoliotic curvature and complications. Irreversible changes in cardiac and pulmonary function pose serious risks to anaesthesia and have been relative contraindications to surgery [7, 17, 18, 20, 22, 23].
In a previous study, the authors reported the clinical and radiological results of DMD scoliosis surgery in patients with a low forced vital capacity (FVC) of <30%, conventionally considered too low to permit reasonable surgical risk [23]. Scoliosis surgery for such patients must provide meaningful benefit in their function, QOL and satisfaction in proportion to risks involved for patients and parents.
The purpose of this study was to determine if scoliosis surgery improved function and QOL in patients with severe DMD scoliosis and high risk pulmonary dysfunction. Furthermore, the authors assessed the patient’s and parent’s satisfaction after scoliosis surgery.
Materials and methods
This study was approved by the Institutional Review Board of Kitasato University and informed consent was obtained from all patients prior to participation in this study.
Between 2005 and 2007, a total of 14 patients with scoliosis secondary to DMD and a FVC of <30% of predicted value at the time of admission underwent scoliosis surgery. Before surgery, all patients were nonambulatory. All patients were able to ventilate autonomously and were not respirator dependent. They were trained with preoperative inspiratory muscle training by a pulmonary trainer (Threshold IMT) (Figs.1 and 2 ) for six weeks prior to surgery [23]. All patients recovered well following the surgery with no major complications [23]. They were encouraged to continue inspiratory muscle training after surgery and even at home after discharge.
Pulmonary trainer (Threshold IMT, Philips Respironics, Inc., Murrysville, PA, USA) provides consistent and specific pressure for inspiratory muscle strength and endurance training, regardless of how quickly or slowly patients breathe. This device incorporates a flow-independent one-way valve to ensure consistent resistance and features an adjustable specific pressure setting (in cm H20) to be set by a healthcare professional. When patients inhale through Threshold IMT, a spring-loaded valve provides a resistance that exercises respiratory muscles through conditioning
Pulmonary function tests [23]
Pulmonary function tests were performed with a computerised pulmonary function system (FUDAC-50, Fukuda Denshi, Tokyo). Pulmonary function values reported in this study are forced vital capacity (FVC) expressed as percent of predicted value (%FVC) on the published normative data. Pulmonary function tests were evaluated at six weeks and three weeks before surgery, the day before surgery, and then at six weeks, one year and two years after surgery as well as at the last follow-up. %FVC was measured three times and evaluated by one independent observer. The best trial for the test was used for further analysis.
Inspiratory muscle training [9, 11, 23]
After surgery and even in the home after discharge, patients had to perform both resistive breathing manoeuvres and maximal static inspiratory efforts. They were trained with inspiratory muscle training by a pulmonary trainer.
The pulmonary trainer resistive exercise intervention was based on previously published protocols. Inspiratory muscle training was performed daily. Three sets of 15 repetitions were performed.
Radiographic assessments
Radiographic assessments were performed on anteroposterior spinal radiographs covering the whole spinal column with the patient in sitting position. These assessments were made the day before surgery, in the postoperative week, at one and two years after surgery and at the last follow-up. The Cobb angles of the curves and the pelvic obliquity (spinal pelvic obliquity [SPO]) on the coronal plane were measured.
Surgical procedure [23]
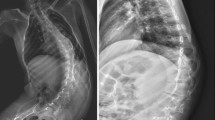
The primary aim of this surgery was to obtain a solid fusion, level pelvis and a balanced spine. All patients had posterior spine fusion and all-screw construction from the upper thoracic spine (T3 or T4) to the lower lumber spine (L5) for scoliosis, performed by the same surgeon (M.T.) as described in the previous study (Fig. 3). No anterior surgery was performed in any of these consecutive series. All operations were performed under general anaesthesia.
a, b A 13-year-old boy with DMD. Anteroposterior radiograph shows severe scoliosis of 93° with significant pelvic obliquity of 20°. Thoracic hypokyphosis and lumbar hyperlordosis were present. c, d All-screw constructs and fusion to L5 were performed. Postoperative sitting views show significant coronal curve correction of 20° with normalization of sagittal plane. Pelvic obliquity improved to 5°
Patient/parent evaluation of surgery
At the last follow-up, patients and parents were interviewed and asked to complete an outcome questionnaire by one independent observer. The authors modified the previous questionnaire described by Bridwell et al. [5] and made our own simple outcome questionnaire. Six of the questions addressed function (questions 1–6), two addressed quality of life (questions 7 and 8) and three targeted satisfaction (questions 9–11).
Results
A total of 14 consecutive patients were enrolled in this study. No patient was lost to follow-up. The mean follow-up period was four years one month (range, 2 years 6 months to 5 years 11 months). Details of radiographic parameters in the study group are shown in Table 1. Changes in %FVC are shown in Fig. 4. The mean %FVC at the time of admission was 21.6% (range, 16–27%). There were no ventilator dependent patients preoperatively. %FVC increased to 26.2% (range, 22–31%) the day before surgery after six-week inspiratory muscle training. %FVC remained stable or increased slightly in all patients at six weeks after surgery. %FVC continued to decrease to 23.2% (range, 19%–27%) at one year after surgery, 20.1% (range, 16%–25%) at two years after surgery and 12.0% (range, 9%–22%) at the last follow-up (four years one month after surgery). The mean rate of %FVC decline after surgery was 3.6% per year in our patients.
Changes in %FVC are demonstrated. After preoperative respiratory muscle training for six weeks, %FVC increased in all patients. All 14 patients underwent surgical correction of scoliosis successfully without any complications. At six weeks after operation, %FVC remained stable or increased slightly. %FVC decreased in all patients at one year, two years after operation and at the last follow-up. The average rate of decline of %FVC was 3.6% per year at the last follow-up
The mean preoperative scoliotic curvature was 98° (range, 81°–130°).The mean immediate postoperative scoliotic curvature was 34° (range, 20°–40°). The mean scoliotic curvature was 35° (range, 23°–42°) at the last follow-up. The pelvic obliquity improved from a preoperative mean of 22° (range, 15°–34°) to an immediate postoperative mean of 8° (range, 4°–17°) and a mean of 8° (range, 5°–17°) at the last follow-up. No significant loss of correction of scoliotic curvature and pelvic obliquity was found at the last follow-up.
Balanced sitting posture was achieved and maintained in all but three patients who had postoperative pelvic obliquity of >15°. These three patients had preoperative Cobb angles of 101°, 128° and 130° and pelvic obliquities of 29°, 30° and 34°, respectively.
Table 2 shows the questionnaire with answers and the tally for each of the questions broken down into the total answers. All patients reported difficulty in sitting. After surgery, all patients reported major or moderate improvement (question 1). All patients reported difficulty using their arms and hands before surgery due to poor sitting balance. After surgery, 14 patients reported improvement and only one reported no change (question 2).
Before surgery, all patients were able to feed themselves. At the last follow-up, ten patients were able to feed themselves but four patients were unable to feed themselves because their arms were getting weaker (question 3). Two of the 14 patients/parents reported problems with digestive systems before surgery. Both of them reported major or moderate improvement (question 4). Nine patients reported respiratory problems before surgery. At the last follow-up, six reported moderate to major improvement and three reported minimal improvement. In the assessment of the child's overall activity level, 14 patients reported improvement (question 6). Only two patients had pressure sores before surgery. Both of them reported a major improvement after surgery (question 7). Regarding the overall quality of life, all 14 children reported improvement (question 8). All patients considered the surgery successful and satisfactory (question 9). Twelve of the 14 patients definitely would have the surgery again, and only two probably would have (question 10). Twelve of the 14 patients definitely would recommend the surgery and two probably would recommend it (question 11).
Discussion
Motor strength and pulmonary function are the key issues of function and QOL in patients with DMD, while scoliosis surgery has been highly effective in stabilising the spine and maintaining comfort and sitting balance [1–5, 7, 10, 13, 15–18, 20, 22]. Scoliosis surgery should be early enough in the course of the underlying disease, when cardiac and pulmonary function is sufficient, so that patients can be anaesthetised and operated relatively safely in order to reduce the likelihood of major complications [1, 3, 22].
Due to the profound cardiopulmonary compromise of the patients, they are more susceptible to postoperative pneumonia, prolonged ventilator dependence, cardiac failure and even death [1, 5, 16, 20]. We routinely provide the preoperative information and guidance (informed consent) concerning this high pulmonary risk scoliosis surgery for the patients/parents at the time of admission.
Although potential risks and peri/postoperative complications should be considered, there has been also overwhelming support for the beneficial effect of scoliosis surgery on general well-being of the patient. Despite the magnitude of this surgery, the successful outcome of an operation for DMD scoliosis has been considered beneficial by most patients and their principal care providers [1, 5, 7]. The patient's function will be worse because of the progressively deteriorating nature of the disease as well as further progressive scoliosis if surgery is not performed. Therefore, we have recommended this surgery even if the patient presents late and is at high risk. However, surgery should be discussed thoroughly and we are of the opinion that the decision whether the patient will undergo surgery or not must be made by the patients/parents after sufficient discussion.
Pulmonary complications in the peri/postoperative period in DMD patients have been reported to be frequent [1, 16, 18, 21]. Higher pulmonary complications have been reported when the FVC is <30% [7, 8, 10, 19].
Pneumonia, respiratory arrest, pneumothorax as well as difficulties in weaning from the respirator have been reported [1, 8, 16, 19, 21]. Thus, many surgeons have recommended scoliosis surgery only for patients who have a FVC of at least 35–40% [7, 18, 21]. To prevent pulmonary complications and to increase pulmonary function, we recommend preoperative respiratory muscle training using threshold IMT when the patient decides to undergo surgery.
Thus, scoliosis surgery in patients with DMD is challenging, and yet the authors’ contention has been that the rate of complications with scoliosis surgery in patients with DMD and poor pulmonary function is low and that the surgery is substantial. However, there has been concern that patients/parents may not believe the scoliosis surgery to be of significant benefit, considering the magnitude of the surgery, high rates of complication and mortality and the generally downhill course of the underlying neuromuscular disorders. This study shows that our patients have been managed successfully with no major complication. Although many studies have reported that the role of scoliosis surgery in patients with DMD is to prevent or retard deterioration of function and sitting balance rather than to improve it because DMD is a progressively deteriorating myopathic disorder [1, 15–22], this study also shows most parents/patients believed that high risk scoliosis surgery improved their function, sitting balance and QOL. The authors were surprised with the strongly positive perceptions of most of the patients/parents with DMD scoliosis and high risk pulmonary dysfunction.
There have been few QOL measures appropriate for DMD scoliosis. In 1999, Bridwell et al. [5] devised a questionnaire that assessed patient function, pain, cosmesis, self-image, and the QOL for flaccid neuromuscular (Duchenne muscular dystrophy and spinal muscular atrophy) scoliosis patients. In their work, they reported that most patients/parents believed scoliosis surgery improved patient function, cosmesis, sitting balance and QOL. The authors modified their questionnaire and devised our simple questionnaire that assessed patient function, the QOL and satisfaction.
With the results of this study, most patients/parents believed scoliosis surgery improved function, sitting balance and QOL with a long-term follow-up. The favourable results related to QOL and overall satisfaction. However, DMD is a flaccid neuromuscular disorder in which gradual deterioration is the hallmark, and thus the less favourable evaluations appeared to concern function.
It may be that it reflects the progressively deteriorating nature of the disorder. Balanced sitting posture was achieved in all patients except for three who had postoperative pelvic obliquity of >15°. These three patients probably should have had pelvic fixation. However, they reported improvement in sitting balance and did not complain of difficulties in sitting. The coronal balance has been reported to be the most important parameter affecting sitting [4]. With a mean of 65% correction, our study shows good results for coronal deformity despite preoperative severe scoliotic curvature. Thus, the sitting balance appeared to be improved and maintained in our patients.
It is interesting to note that all patients reported improvement of pulmonary function, although there was a significant decrease in %FVC in all patients at the last follow-up. While pulmonary function deterioration is primarily due to respiratory muscle weakness, the negative mechanical effects of the deformed thorax on the underlying lung has been suggested. The authors believe that chest wall deformity and respiratory tract deformity caused by spinal deformity are effectively treated by correcting spinal deformity and thereby patients felt improvement of pulmonary function.
Because of the absence of control groups, the authors can not contribute to the controversy whether scoliosis surgery affects the rate of decline of pulmonary function in DMD patients. Most studies could not document positive effects of scoliosis surgery on pulmonary function [12, 14, 19]. Beneficial effects of scoliosis surgery on pulmonary function have been reported in only a few studies [6, 24]. Recently, Velasco et al. [24] showed positive effects of posterior spinal stabilisation on pulmonary function by showing slowed rate of %FVC decline from 8.0% per year before surgery to 3.9% per year after surgery with a long-term follow-up. Koessler et al. [9] have shown that inspiratory muscle training in patients with DMD improves inspiratory muscle function and that the training leads to a stabilisation of %FVC even in the long-term of two years. Although our patients were encouraged to continue inspiratory muscle training to stabilise or retard %FVC decline even after surgery, there was a continuous %FVC decline in all patients and the rate of %FVC decline was 3.6% per year with a mean follow-up of three years five months. This value compares favourably with Velasco’s result even though the number of our cases is too small.
In conclusion, %FVC in patients with severe scoliosis secondary to Duchenne muscular dystrophy increased after preoperative inspiratory muscle training prior to scoliosis surgery. Scoliosis surgery in this group of patients presented no increased risk of major complications. There was no mortality. In all cases, patients were extubated immediately after surgery in the operating room and no respiratory support was required in the peri/postoperative period. All-screw constructions and fusion to L5 in DMD patients with severe spinal deformity and high pelvic obliquity offered the ability to correct scoliotic curvature and pelvic obliquity initially, intermediate and long-term. All patients were encouraged to continue inspiratory muscle training after surgery. The mean rate of %FVC decline after surgery was 3.6% per year. Most patients/parents believed scoliosis surgery improved their function, sitting balance and quality of life even though patients were at high risk for major complications. Patient satisfaction was also high. They benefitted from scoliosis surgery.
References
Askin GN, Hallettv R, Hare N, Webb JK (1997) The outcome of scoliosis surgery in the severely handicapped child: an objective and subjective assessment. Spine 22:44–50
Bell DF, Moseley CF, Koneska J (1989) Unit rod segmental instrumentationin the management of patients with progressive neuromuscular spinal deformity. Spine 14:1301–1307
Bonnett C, Brown JC, Perry J, Nickel VL, Walinski T, Brooks L, Hoffer M, Stiles C, Brooks R (1975) Evolution of treatment of paralytic scoliosis at Ranchos Los Amigos Hospital. J Bone Joint Surg Am 57:206–215
Braun N, Narinder SA, Rochester DF (1983) Respiratory muscles and pulmonary function in polyositis and other proximal myopathies. Thorax 38:616–623
Bridwell KH, Baldus C, Iffrig TM (1999) Process measures and patient/parent evaluation of surgical management of spinal deformities in patients with progressive flaccid neuromuscular scoliosis (Duchenne’s muscular dystrophy and spinal muscular atrophy). Spine 24:1300–1309
Galasko CBS, Delany C, Morris P (1992) Spinal stabilization in Duchenne muscular dystrophy. J Bone Joint Surg Br 74:210–220
Gill I, Eagle M, Mehta JS, Gibson MJ (2006) Correction of neuromuscular scoliosis in patients with preexisting respiratory failure. Spine 31:2478–2483
Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K (2005) Scoliosis correction with pedicle screws in Duchnne muscular dystrophy. Euro Spine J 17:255–261
Koessler W, Wanke T, Winkler G, Nader A, Toifl K, Kurz H, Zwick H (2001) 2 years’ experience with inspiratory muscle training in patients with neuromuscular disorders. Chest 120:765–769
Kurz LT, Mubarak SJ, Schultz P, Park SM (1983) Leach J (1983) Correlation of scoliosis and pulmonary function in Duchenne muscular dystrophy. J Pediatr Orthop 3:347–355
Leith DE, Bradley M (1976) Ventilatory muscle strength and endurance training. J Appl Physiol 41:508–516
Marsh A, Edge G, Lehovsky (2003) Spinal fusion in patients with Duchenne’s muscular dystrophy and a low forced vital capacity. Euro Spine J 12:507–512
Mercado E, Alman B, Wright G (2007) Does spinal fusion influence quality of life in neuromuscular scoliosis? Spine 19S:120–125
Miller RG, Chalmers AC, Dao H, Filler-Katz A (1991) The effects of spine fusion on respiratory function in Duchenne muscular dystrophy. Neurology 41:38–45
Oda T, Shimizu N, Yonenobu K, Ono K, Nabeshima T, Kyoh S (1983) Longitudinal study of spinal deformity in Duchenne muscular dystrophy. J Pediatr Orthop 13:478–488
Padman R, McNamara R (1990) Postoperative pulmonary complications in children neuromuscular scoliosis who underwent posterior spinal fusion. Del Med J 62:999–1003
Rawlins BA, Winter RB, Lonstein JF (1990) Reconstructive spinal surgery in pediatric patients with major loss in vital capacity. J Pediatr Orthop 16:284–292
Sakai DN, Hsu JD, Bonnett DA, Bonnett DA, Brown CJ (1997) Stabilizationnof the collapsing spine in Duchenne muscular dystrophy. Clin Orthop 128:256–260
Shapiro F, Specht L (1983) The diagnosis and orthopaedic treatment of inherited muscular diseases of childhood. J Bone Joint Surg Am 75:439–445
Sticker U, Moser H, Aebi M (1996) Predominantly posterior instrumentation and fusion in neuromuscular and neurogenic scoliosis in children and adolescents. Euro Spine J 5:101–106
Sussman MD (1984) Advantage of early spinal stabilization and fusion in patients with Duchenne muscular dystrophy. J Pediatr Orthop 4:532–538
Swank SM, Brown JC, Perry RE (1982) Spinal fusion in Duchenne’s muscular dystrophy. Spine 7:484–491
Takaso M, Nakazawa T, Imura T, Takahira N, Itoman M, Takahashi K, Yamazaki M, Otori S, Akazawa T, Minami S, Kotani T (2009) Surgical management of severe scoliosis with high-risk pulmonary dysfunction in Duchenne muscular dystrophy. International Orthop. doi:10.1007/s0026400907647
Velasco MV, Colin AA, Zurakowski D, Darras BT, Shapiro F (2007) Posterior spinal fusion for scoliosis in Duchenne muscular dystrophy diminishes the rate of respiratory decline. Spine 32:459–465
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Takaso, M., Nakazawa, T., Imura, T. et al. Surgical management of severe scoliosis with high risk pulmonary dysfunction in Duchenne muscular dystrophy: patient function, quality of life and satisfaction. International Orthopaedics (SICOT) 34, 695–702 (2010). https://doi.org/10.1007/s00264-010-0957-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-0957-0