Abstract
The use of impacted morselized cancellous bone grafts in conjunction with cementless hemispherical acetabular cups for treatment of AAOS type II acetabular cavitary deficiencies was evaluated in a retrospective study of 23 primary and 24 revision total hip arthroplasties, at a mean follow-up of 7.9 and 8.1 years, respectively. All primary hips received autografts, while all revision hips received allografts. Modified Harris Hip Scores for primary and revision hip replacements increased from a pre-operative mean of 37 and 47 to a postoperative mean of 90 and 86, respectively. All 23 autografts and 23 out of 24 cancellous allografts were radiographically incorporated without evidence of resorption. There were no instances of infection, component migration, or cases requiring subsequent acetabular revision. We conclude that impacted morselized cancellous bone-graft augmentation of cementless cups is a viable surgical option for AAOS type II cavitary acetabular defects.
Résumé
L’utilisation de greffes impactées morcelées en adjuvant d’une cupule non cimentée hémisphérique dans le traitement des pertes de substances osseuses acétabulaires de type AAOS II a été évaluée lors d’une étude rétrospective portant sur 23 prothèses primaires et 24 prothèses de révision avec un suivi moyen de 7.9 ans et 8.1 ans. Toutes les prothèses primaires ont été traitées par auto greffes alors que les révisions ont été traitées par allogreffes. Le score de Harris modifié pour les prothèses primaires et pour les révisions a été respectivement en préopératoire de 37 et 47 et s’est amélioré en postopératoire à 90 et 86. Les 23 auto greffes et les 23 sur 24 allogreffes ont été incorporées radiologiquement sans résorption. Il n’y a pas eu d’infection, pas de migration de la cupule, aucune révision acétabulaire. Nous pouvons conclure que la greffe impactée morcelée en conjonction avec la mise en place d’une cupule sans ciment est une procédure chirurgicale fiable pour le traitement des pertes de substances osseuses cavitaires de type AAOS II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The primary goal of cementless acetabular component implantation in total hip arthroplasty (THA) is to provide a well-fixed component, creating an environment for long-term implant stability and eventual biological fixation. Acetabular bone stock deficiency encompasses a broad spectrum of deformities, including segmental defects, cavitary defects, and pelvic discontinuity. These defects can be encountered in both the primary and revision hip arthroplasty. Revision of acetabular components in particular has become more challenging due to loss of acetabular bone stock from earlier procedures or osteolysis. Restoration of existing bone deficits for future surgical needs is an increasingly important consideration.
Cavitary defects can be addressed by a number of techniques, including creating a high hip center [19] and/or medialization of the cup [5]. Unfortunately, these techniques may adversely alter normal joint biomechanics. Alternatively, the defect can be filled by any of a number of substances to allow more anatomic positioning of the component—including metallic components such as “double bubble” or jumbo cups [10], modular porous metal augments [15]—or with bulk or morselized bone graft. Once the defect is packed with cancellous graft, either a cemented polyethylene [21, 24] or cementless titanium hemispherical component [9] can be inserted. The use of morselized cancellous bone graft for cavitary defects in the acetabulum is well established in practice, especially for acetabular revisions [8, 16]; however, the authors are unaware of any study that has been reported in the use of morselized cancellous bone graft for cavitary acetabular defects in primary THAs.
This study reviewed the experience at the authors’ institution using cancellous grafts in conjunction with cementless hemispherical acetabular components in the management of AAOS type II (cavitary) defects [2] in both the primary as well as the revision setting. In type II cavitary defects, adequate host peripheral bone is present in the anterior and posterior columns to allow implantation of press-fit hemispherical components without structural grafting. Central cavitary defects in either the superior weight-bearing dome or medial wall were treated with cancellous autograft or allograft to augment existing bone stock. Supporting and restoring these central defects is critical to preventing long-term axial migration of the components [3].
Materials and methods
Institutional Review Board approval and patient consent were obtained prior to the start of this study. A retrospective analysis of 23 consecutive primary THAs performed in 20 patients and 24 consecutive revision THAs in 24 patients with AAOS type II cavitary defects filled with impacted morselized cancellous allograft bone over a 10 year period was performed. Three patients in the revision group died before the time of the review; all of these patients were followed up on a regular basis until their death (at 32, 74, and 146 months postoperatively) and were included in the study. There were 6 males and 14 females in the primary THA group and 7 males and 17 females in the revision THA group. The average age of patients undergoing primary THA was 62 years (range 28–83) and the average age of patients undergoing revision THA was 54 years (range 30–87). Preoperative diagnosis in the primary THA group was primary osteoarthritis in 9 hips, rheumatoid arthritis in 10 hips, osteoarthritis secondary to avascular necrosis in 1 hip, and osteoarthritis secondary to congenital dysplasia in 3 hips. Prerevision diagnosis in the revision THA group was osteoarthritis in 10 hips, rheumatoid arthritis in 10 hips, avascular necrosis in 3 hips, and congenital dysplasia in 1 hip. Reasons for revision THA were aseptic loosening in 22 hips, catastrophic polyethylene wear in 1 hip, and infection in 1 hip.
Autograft was used in all 23 primary hip replacements, and allograft was used in all 24 revision THAs. Cases requiring additional bulk allograft were excluded. Intraoperative records were reviewed to determine the source (autograft vs. allograft) and type of bone graft used. Cancellous graft was obtained by using acetabular reamers, and additional bone was obtained from the proximal femoral metaphysis if needed. All allograft bone (femoral heads harvested sterile, frozen, and not irradiated) in the study was obtained from the Musculoskeletal Transplant Foundation (Edison, NJ, USA).
The posterolateral approach was used in 17 primary THAs and 15 revision THAs; the lateral approach was used in the remaining 6 primary THAs and 9 revision THAs. For both primary and revision cases after the capsule was entered the acetabular bed was reamed to bleeding bone. Morselized graft (from acetabular reaming) was hand compressed into a ball and placed into the contained acetabular defect; in some cases thin (less than 3 mm) wafers of cancellous bone were obtained from the femoral neck using an oscillating saw, decorticated, and placed in the defect along with cancellous graft. The appropriately sized acetabular component was placed into the acetabulum and tapped into position. Multiple light hammer blows were used during this process to impact the graft and allow for fluid to be forced from the morselized bone graft. Acetabular sockets were underreamed by 1 to 2 mm and the component was press-fitted into place. Greater than two-thirds rim fit of the cup to host bone was obtained in all cases. Additional screw augmentation was used as determined by the surgeon at the time of implantation.
Preoperative and final follow-up modified Harris Hip Scores [11], as well as complications, were recorded. The Student t-test was used to compare pre- and postoperative hip scores (significance, p<0.05). Kaplan-Meier survivorship analysis with 95% confidence intervals was used to implant survivorship.
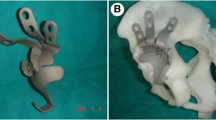
Preoperative, immediate postoperative, and final follow-up anterior-posterior radiographs of the pelvis were reviewed (Fig. 1). Variations in magnification were corrected using the known diameter of the femoral head as an internal reference. Preoperative films were classified according to AAOS acetabular deficiency [2]; the radiographic classification was confirmed from the operative report. Component height, horizontal position, and acetabular component inclination were recorded [3, 12, 14]. An implant was considered radiographically loose if there was a >2-mm radiolucency in any Charnley zone, component migration in vertical or horizontal position of >2 mm, any radiolucency in two contiguous Charnley zones, or a change in inclination of >4°. Bone graft was considered incorporated if remodeling and trabecular bone formation were observed after an initial increase in radiodensity.
Results
Forty-seven THAs were followed up clinically and radiographically with a mean follow-up of 7.9 years (94.3 months (range 34–198 months)) in the primary group and 8.1 years (96.7 months (range 31–202 months)) in the revision group.
In the revision acetabulum cases, 17 were performed in conjunction with a femoral revision, and 7 were isolated acetabular revisions. Additional screw augmentation (1–4 screws) was used in 16 of the 47. Eleven primary and 9 revision cases used morselized cancellous bone alone, while 12 primary cases and 15 revision cases had additional corticocancellous femoral head wafers applied to the medial deficiency, with the remaining void packed with morselized cancellous bone.
Nine of 23 primary and 14 of 24 revision hips were permitted weightbearing as tolerated with assistive device from the first postoperative day as per surgeons’ standard protocol. The remaining patients were instructed in protected weightbearing (single-leg stance with device) for the first 6 to 12 weeks on the affected limb. Once adequate incorporation was noted on follow-up films, patients progressed to weightbearing as tolerated with an assistive device as needed.
Modified Harris Hip Scores in the primary group increased from a preoperative mean of 36.5 (range 18–64) to a postoperative mean of 90.3 (range 58–100) (p<.01). Twenty-one of 23 of the primary group had a modified Harris Hip Score of good to excellent (>80) at the most recent follow-up. Scores in the revision group increased from a preoperative mean of 47 (range 18–75) to a postoperative mean of 86 (range 59–100) (p<.01). Twenty-two of 24 (92%) of the revision patients had a modified Harris Hip Score of good to excellent (>80) at most recent follow-up.
Immediate and final follow-up radiographs were evaluated. All grafts appeared to be well incorporated at the time of final radiographic follow-up (Fig. 1). While time to initial formation of trabeculae in the grafted area was not specifically recorded, most grafts tended to show a characteristic increase and then decrease in density with subsequent trabecular pattern by 6 months. Once formed, none of these regions showed a later loss of density or trabeculae in the grafted region.
Nonprogressive radiolucent lines (all <2 mm) [17] were noted in acetabular Charnley zones at the following rates: in the primary group 17% in zone I, none in zone II, and 4% in zone III; in the revision group, 33% in zone I, 8% in zone II, and 8% in zone III. In none of the primary cases and 8% of revision cases were lines visible in two contiguous Charnley zones (Fig. 2).
A radiolucent line of >2 mm was detected in all Charnley acetabular zones in a single patient. This patient, with revision THA, had a 1 mm lucency in zone I as well as a 2 mm lucency in zones II and III at 64 months follow-up. The patient was asymptomatic, with a Harris Hip Score of 97. This patient would be considered loose by the criteria used by Garcia [9]; however, given the excellent clinical result, this may represent a fibrous-ingrowth stable implant. Five other revision cases had a 1–2 mm lucency in zone I and a 1–2 mm lucency in part of zone II. These patients were also asymptomatic at an average of 85.6 (range 32–138) months follow-up with a mean modified Harris Hip Score of 84. Of the remaining hips, 91.3% of primary hips and 87.5% of revision hips had no lucent zones of >2 mm at final follow-up.
All lucencies were nonprogressive over the course of the study follow-up, and no components showed evidence of axial migration of >4 mm or change in tilt of >4°. Mean inclination of the components was 47.2° in the primary group and 43.5° in the revision group. None was clinically loose nor underwent acetabular revision.
Survivorship analysis was performed for both the primary and revision THA patients. There was 100% survival with either revision or radiographic loosening as an endpoint in all 23 hips undergoing primary THA. In the 24 revision THA patients treated with impacted allograft there was 100% survival at 10 years with revision as the endpoint. When radiographic evidence of loosening was used as an endpoint, there was 80% survival at 10 years (95% confidence interval 59–99%).
Discussion
The purpose of this study was to identify a group of patients treated with a similar technique at a single institution in order to focus on the outcome of impacted morselized cancellous grafts with cementless hemispherical components in the presence of cavitary defects. The results of impacted morselized cancellous allograft with autograft were not compared because these two bone graft sources were used in the distinctly different circumstances of primary and revision THA. This is the only study, as far as the authors are aware, about the outcomes of morselized cancellous bone graft for acetabular cavitary defects in primary THAs. In both primary and revision groups we had excellent mid-term results with no clinical failures and one nonprogressive, asymptomatic radiographic lucency of >2 mm. In addition, acetabular cup inclination was not compromised by the need to achieve rim fit to host bone; implants were placed near the desired abduction angle of 45° [9]. These results are encouraging for both the clinical improvement of patients as well as the radiographic restoration of acetabular bone stock.
Cementless cups are generally accepted to be a viable option for primary as well as revision hip arthroplasties. In a recent study by Valle [23], there was a 98% survival in 308 hips with a cementless porous-coated cup for primary hip replacements in the intermediate term. Similarly, Della Valle [4] showed that the use of cementless porous-coated cups have a 96% survival in terms of aseptic loosening at 15 years; similar results have been reported by other authors over the last decade [6, 7, 20].
Our results compared favorably to other series where contained acetabular defects were treated with impaction bone grafting and cemented acetabular cups. In 35 consecutive THA revision cases in patients with rheumatoid arthritis which were treated with impacted morselized allograft for contained acetabular defects, Scheurers [18] demonstrated 80% survivorship at 8 years. Welten [24] also reported 94% survival—with revision as the endpoint at 12.3 years—of impacted morselized allograft in the revision setting in 69 acetabular revisions. Slooff [22] reported on 47 total hip arthroplasties treated with cancellous packing and cemented polyethylene acetabular components in a heterogeneous population of both cavitary and combined defects. Using re-revision as an endpoint, he reported a 6% (3 patients) failure rate at mean 12-year follow-up [24]. Three additional components were radiographically loose, however, and one component was infected. Slooff [21] previously reported on this cohort of patients and noted four (5%) clinical failures and six (7%) cases of radiographic loosening out of 88 hips at 5 years follow-up [21].
There are few reports on the use of morselized bone graft and cementless cups. Garcia-Cimberto et al. reported on a heterogeneous population of 65 revision acetabular cups in which bone grafts (a combination of morselized and bulk grafts) and porous-coated cementless cups were used at a mean 8-year follow-up [9]. These authors noted an 11% re-revision rate and 22% poor clinical results. Seventy percent of cups had a radiolucency in one or more DeLee and Charnley zones. In a subpopulation of cases with less than 50% host bone-implant contact, however, they reported a 100% failure rate; Garcia-Cimberto [9] concluded that cementless components are contraindicated in this group with less than 50% host bone contact. Etienne et al. reported on 108 hips revised for acetabular osteolysis with morselized allografts and cementless cups; 95% were clinically and radiologically successful at a mean follow-up of 85 months [8]. They found that all cavitary defects had radiological incorporation except for two cases where noncircumferential radiolucencies were observed.
A study on morselized allograft in acetabular revision by Kligman et al. [13] investigated the difference in outcomes between 30 hips with morselized cortical allograft versus 30 matched hips with morselized cancellous allograft. At a mean of 7.4 years, they found that there was more cup migration (>5 mm) in the group which had cancellous bone graft than that which had cortical bone graft, and they hypothesized that cortical bone graft was superior to cancellous bone graft biomechanically. Bolder et al. [1] showed that smaller graft size led to greater migration and loss of initial stability in a cadaveric and synthetic pelvic model study. However, the cups in both the above studies were cemented polyethylene cups and not cementless cups, as in our study. Results from this study would suggest that these data are not applicable to the use of cancellous graft with cementless cups. We hypothesize that if there is good rim fixation with supplemental screw fixation as necessary, then the host bone and not the graft can maintain initial cup stability independent of the graft’s material properties to prevent component migration.
References
Bolder SB, Schreurs BW, Verdonschot N, van Unen JM, Gardeniers JW, Slooff TJ (2003) Particle size of bone graft and method of impaction affect initial stability of cemented cups: human cadaveric and synthetic pelvic specimen studies. Acta Orthop Scand 74:652–657
D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, Steinberg ME, Stulberg SD, Wedge JH (1989) Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res 126–137
DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 20–32
Della Valle CJ, Berger RA, Rosenberg AG, Galante JO (2004) Cementless acetabular reconstruction in revision total hip arthroplasty. Clin Orthop Relat Res 96–100
Dorr LD, Tawakkol S, Moorthy M, Long W, Wan Z (1999) Medial protrusio technique for placement of a porous-coated, hemispherical acetabular component without cement in a total hip arthroplasty in patients who have acetabular dysplasia. J Bone Jt Surg Am 81:83–92
Dorr LD, Wan Z (1995) Ten years of experience with porous acetabular components for revision surgery. Clin Orthop Relat Res 191–200
Engh CA, Glassman AH, Griffin WL, Mayer JG (1988) Results of cementless revision for failed cemented total hip arthroplasty. Clin Orthop Relat Res 91–110
Etienne G, Bezwada HP, Hungerford DS, Mont MA (2004) The incorporation of morselized bone grafts in cementless acetabular revisions. Clin Orthop Relat Res 241–246
Garcia-Cimbrelo E (1999) Porous-coated cementless acetabular cups in revision surgery: a 6- to 11-year follow-up study. J Arthroplasty 14:397–406
Gustke KA (2004) Jumbo cup or high hip center: is bigger better? J Arthroplasty 19:120–123
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Jt Surg Am 51:737–755
Johnston RC, Fitzgerald RH Jr, Harris WH, Poss R, Muller ME, Sledge CB (1990) Clinical and radiographic evaluation of total hip replacement. A standard system of terminology for reporting results. J Bone Jt Surg Am 72:161–168
Kligman M, Padgett DE, Vered R, Roffman M (2003) Cortical and cancellous morselized allograft in acetabular revision total hip replacement: minimum 5-year follow-up. J Arthroplasty 18:907–913
Massin P, Schmidt L, Engh CA (1989) Evaluation of cementless acetabular component migration. An experimental study. J Arthroplasty 4:245–251
Nehme A, Lewallen DG, Hanssen AD (2004) Modular porous metal augments for treatment of severe acetabular bone loss during revision hip arthroplasty. Clin Orthop Relat Res 201–208
Paprosky WG, Magnus RE (1994) Principles of bone grafting in revision total hip arthroplasty. Acetabular technique. Clin Orthop Relat Res 147–155
Salvati EA, Im VC, Aglietti P, Wilson PD Jr (1976) Radiology of total hip replacements. Clin Orthop 74–82
Schreurs BW, Thien TM, de Waal Malefijt MC, Buma P, Veth RP, Slooff TJ (2003) Acetabular revision with impacted morselized cancellous bone graft and a cemented cup in patients with rheumatoid arthritis: three to fourteen-year follow-up. J Bone Jt Surg Am 85-A:647–652
Schutzer SF, Harris WH (1994) High placement of porous-coated acetabular components in complex total hip arthroplasty. J Arthroplasty 9:359–367
Silverton CD, Rosenberg AG, Sheinkop MB, Kull LR, Galante JO (1996) Revision of the acetabular component without cement after total hip arthroplasty. A follow-up note regarding results at seven to eleven years. J Bone Jt Surg Am 78:1366–1370
Slooff TJ, Buma P, Schreurs BW, Schimmel JW, Huiskes R, Gardeniers J (1996) Acetabular and femoral reconstruction with impacted graft and cement. Clin Orthop 108–115
Slooff TJ, Schimmel JW, Buma P (1993) Cemented fixation with bone grafts. Orthop Clin North Am 24:667–677
Valle AG, Zoppi A, Peterson MG, Salvati EA (2004) Clinical and radiographic results associated with a modern, cementless modular cup design in total hip arthroplasty. J Bone Jt Surg Am 86-A:1998–2004
Welten ML, Schreurs BW, Buma P, Verdonschot N, Slooff TJ (2000) Acetabular reconstruction with impacted morcellized cancellous bone autograft and cemented primary total hip arthroplasty: a 10- to 17-year follow-up study. J Arthroplasty 15:819–824
Acknowledgements
The authors are grateful for the contributions of Larry Specht, MD, William L. Jaffe, MD, and Joseph D. Zuckerman, MD.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pereira, G.C.T., Kubiak, E.N., Levine, B. et al. Cavitary acetabular defects treated with morselized cancellous bone graft and cementless cups. International Orthopaedics (SICO 31, 445–450 (2007). https://doi.org/10.1007/s00264-006-0220-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-006-0220-x