Abstract
We investigated the radiological and epidemiological data of 4,151 subjects followed up from 1976 to 2003 to determine individual risk factors for hip osteoarthritis (OA), hip pain and/or treatment by total hip replacement (THR). Pelvic radiographs recorded in 1992 were assessed for evidence of hip-joint degeneration and dysplasia. Sequential body mass index (BMI) measurements from 1976 to 1992, age, exposure to daily lifting and hip dysplasia were entered into logistic regression analyses. The prevalence of hip dysplasia ranged from 5.4% to 12.8% depending on the radiographical index used. Radiological hip OA prevalence was 1.0–2.5% in subjects <60 years of age and 4.4–5.3% in subjects ≥60 years of age. While radiological OA was significantly influenced by hip dysplasia in men and hip dysplasia and age in women, the risk of THR being performed was only influenced by BMI assessed in 1976. Hip-joint degeneration and treatment by THR do not necessarily share the same risk factors, and caution should be exercised in epidemiological studies in attributing one or the other as the end point of coxarthrosis.
Résumé
Nous avons enquêté sur des données radiologiques et épidémiologiques de 4.151 sujets suivi de 1976 à 2003 pour déterminer des facteurs de risque individuels d’arthrose de la hanche, de douleurs de la hanche et/ou du traitement par prothèse totale de hanche (PTH). Les radiographies pelviennes enregistrées en 1992 ont été réparties selon l’atteinte dégénérative de la hanche et la dysplasie. La valeur de l’index de masse corporelle séquentielle de 1976 à 1992, l’âge, l’activité quotidienne et la dysplasie de la hanche sont entrées dans une analyse de régression. La prédominance de la dysplasie de la hanche s’étend de 5,4% à 12,8% selon l’index radiographique utilisé. La prédominance de l’arthrose radiologique était de 1,0 à 2,5% chez les sujets de moins de 60 ans, et de 4,4 à 5,3% chez les sujets de 60 ans ou plus. Tandis que l’arthrose radiologique était significativement influencée par la dysplasie de la hanche chez les hommes, par la dysplasie et l’âge chez les femmes, le risque de réalisation d’une PTH était seulement influencé par l’index de masse corporelle mesuré en 1976. La dégénérescence de la hanche et le traitement par PTH ne partagent pas nécessairement les mêmes facteurs de risque, et la prudence dans les études épidémiologiques devrait être de nommer l’un ou l’autre comme l’événement final de la coxarthrose.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Being overweight, gender and occupational exposure to heavy lifting are significant risk factors for knee osteoarthritis (OA), but similar risk factors have not been as convincingly identified in hip OA [2–4]. This, in our view, is due to methodological problems: a lack of consensus in definitions of radiological OA, the use of radiographic material recorded for other purposes and lack of knowledge of the normal age- and gender-related hip-joint morphology in asymptomatic subjects. Recently, this knowledge has become available, and increased accuracy in determining radiological and symptomatic hip OA in epidemiological studies has resulted [14, 15, 17]. Further controversy concerns the definition of end-stage coxarthrosis. Some authors have used total hip replacement (THR) as the endpoint; others have used radiological criteria only [9, 23]. THR is strictly a pain-relieving procedure, and orthopaedic surgeons have individual criteria for offering the procedure.
In the present study of the Copenhagen Osteoarthritis Study Cohort (4,151 subjects), we investigated sequential measurements of body mass index (BMI) (1976–1992), occupational exposure to repeated daily lifting and hip dysplasia in standardised pelvic radiographs. Radiological evidence of hip OA was assessed using Croft’s classification, and Lanyon’s hip OA discriminator of minimum joint-space width (JSW) ≤2.0 mm [5, 17]. All patients’ records from participants undergoing THR between 1992 and 2003 were reviewed. We evaluated the importance of ageing, gender, increased BMI, hip dysplasia and occupational exposure to daily lifting as risk factors for (1) self-reported pain in the hip joint, (2) radiological hip-joint degeneration and (3) the risk of THR.
Materials and methods
The Copenhagen City Osteoarthritis Study (CCOS)
The Copenhagen City Osteoarthritis Study (CCOS) is a sub-study of the Copenhagen City Heart Study (CCHS). The CCHS is a longitudinal survey of an adult, Caucasian cohort randomly selected from the county of Österbro in Copenhagen. The survey has registered general health factors since 1976.
In 1992 antero-posterior (AP) pelvic and lateral lumbar spine radiographs were recorded in 1,533 men and 2,618 women. Radiographs were obtained standing. Feet pointed straight forward; the lower extremities were positioned in neutral abduction–adduction. In AP pelvic radiographs, the X-ray beam was centred two fingerbreadths over the symphysis pubis. The X-ray beam in lateral lumbar spine radiographs was centred at the apical mid-point of the iliac crest. Tube-to-film distance was 120 cm in all cases. Pelvic rotation during X-ray was assessed using Tönnis’ foramen obturator index (FOI), in which the horizontal width of the right obturator foramen was divided by left obturator foramen width [22].
Radiographic features of hip-joint degeneration
JSW was measured at three locations of the articulation. Minimum JSW was selected as the smallest of these measurements. The authors used two criteria in assigning definite OA to the joint: (1) a minimum JSW value of ≤2.0 mm (equalising mean minimum JSW÷2 standard deviations), regardless of osteophyte formation, subchondral sclerosis or subchondral cysts, according to Lanyon et al., and (2) Croft’s global OA classification, with grades 0–2° designating absent or discrete degeneration and grades 3–5° designating definite OA [5]. One observer (SJ) performed all measurements and classifications using a 0.1 mm-graded magnifying glass (Peak, Tokyo, Japan).
Radiological definition of hip dysplasia
Acetabular morphology was assessed by the acetabular depth ratio (ADR), (cut-off value set at ≤25%). The containment of the femoral head was assessed by the centre-edge (CE) angle (cut-off value set at ≤20°) and the femoral-head extrusion index (FHEI) (cut-off value set at ≥25%) (Fig. 1) [11, 24]. All hip dysplasia assessment was done by a single observer (SJ).
Radiological indices of hip dysplasia. The centre-edge angle describes the angle between a perpendicular line to the horizontal teardrop line drawn through the centre of the femoral head (C) and a line from C to the lateral edge of the acetabulum. The acetabular depth ratio (ADR) describes the percentage of the distance A–B of the distance D–B. The femoral-head extrusion index describes the percentage of the distance H′ (part of the head uncovered by the bony acetabulum) of the distance H′+G′ (femoral-head diameter).
Physical and occupational parameters
At the CCHS first (I) and third (III) examinations of 1976 and 1992, body mass index (BMI/kg/m2) was calculated. The CCHS III questionnaire recorded the nature and duration of occupation since leaving school. For each occupation, the level of repeated lifting was recorded according to the guidelines of The Danish National Board of Industrial Injuries: (1) primarily seated occupation, (2) standing, walking occupation, no repeated lifting, (3) daily repeated lifting equivalent to 50×20 kg, or 20×50 kg, (4) repeated daily lifting equivalent to 50–100×20 kg or 20–50×50 kg, (5) repeated daily lifting equivalent to 100–250×20 kg or 50–100×50 kg.
Self-reported hip pain
At the CCOS baseline examination (1992) the subjects were asked the following question: “Have you experienced recurrent hip pain or deep groin pain during the last 12 months”?
Exclusion of radiographs
In a previous cadaver study we found that extreme pelvic rotation and inclination/reclination had significant influence on hip dysplasia assessment [12]. To stay inside ±3° of error of measurements of the CE angle, FOI inclusion limits of 0.7–1.8 were applied to radiographs. Furthermore, radiographs with pelvic inclination/reclination outside 2 SD of the mean were omitted from the study. Median pelvic inclination was 38° (0–82°), and 1 SD was 9.4°, according to lateral lumbar spine radiographs. Inclusion limits of pelvic inclination thus ranged from 19° to 56°.
Exclusion of subjects
The following exclusion criteria were applied: (1) former surgical treatment of either hip, (2) former fractures of either hip, (3) former treatment of childhood hip disorders, and (4) a history of inflammatory arthritis of any joint.
Reproducibility
Intra-observer reproducibility radiological assessments were evaluated by blinded re-reading of a subset of 100 radiographs 4 weeks after first reading (SJ).
Statistical analysis
Gender-related differences in radiological or physical parameters were investigated by independent samples t tests. The relationships between BMI and minimum JSW were investigated by linear regression analysis and Spearman’s correlation coefficients. The relationships between BMI (1976), BMI III (1992) and Δ BMI (1976–1992) and self-reported hip pain (1992) were investigated by independent samples t tests. Differences in BMI (1976) and BMI III (1992) between subjects who did receive THR and those who did not were investigated by independent samples t tests. The inter-relationships between OA discriminators and dysplasia indices were investigated by χ2 analyses with odds ratios (OR) of risk. Continuous variables, such as age, BMI and years of exposure to repeated daily lifting were tested against minimum JSW (≤2.0 mm), Croft OA grades 3–5° and ±THR by multiple regression analyses. In simple calculations, a significance level of p<0.05 was employed. In multiple regression analyses, the significance level was adjusted to p<0.004 (Bonferroni’s adjustment). All statistical analyses were performed with the SPSS 12.0 statistical software (SPSS Inc., Chicago, IL, USA).
Results
Inclusion and follow up
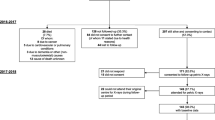
Two hundred and sixty-one sets of radiographs (6.2%) were excluded because pelvic rotation or inclination/reclination exceeded exclusion limits. Furthermore, 236 subjects (5.6%) were excluded due to individual exclusion criteria. Finally, 1,365 men and 2,286 women with a mean age of 62 (range, 22–93) years were included. Mean BMI follow-up period between CCHS I in 1976 and CCHS III in 1992 was 15.4 years. Mean THR follow-up between CCHS III in 1992 and the osteoarthritis sub-study of 2003 (CCOS) was 8.3 years (range, 0.3–10.7 years). In the CCOS observation period between 1992 and 2003, 354 men and 388 women had died (18.1%).
Reproducibility and inter-relationships of radiological parameters
Intra-reader repeatability of Croft overall OA grade was moderate: κ=0.56 for right hips and κ=0.46 for left hips. Dichotomised into grades 0–2° denoting absent or slight OA, and grades 3–5° denoting definite OA, kappa values increased to κ=0.65 for right hips and κ=0.65 for left hips. Intra-reader repeatability of measurements of minimum JSW and hip dysplasia indices was acceptable: intra-class correlation coefficients of minimum JSW were r=0.91 for right hips and r=0.87 for left hips. Intra-class coefficients of dysplasia indices ranged between 0.80 and 0.91. The inter-relationship between the single OA discriminator of minimum JSW ≤2.0 mm and Croft grades 3–5° was found to be good; right hip significance was p<0.001, OR=78.4 (95% CI 50.0–122.8) and left hip significance was p<0.001, OR=69.5 (95% CI 44.0–109.9). We found significant inter-relationships between the individual radiological indices of dysplasia: p values in each analysis <0.001; OR ranging from 10.9 to 81.0.
Prevalence of hip OA and dysplasia
We found gender-related differences in acetabular morphology with male acetabulae being marginally more dysplastic than female acetabulae. For all practical purposes, we found these differences negligible (Table 1). The prevalence of hip dysplasia ranged from 5.4% to 12.8% depending on the index applied. Radiological hip OA prevalence was 1.0–2.5% in subjects <60 years of age and 4.4–5.3% in subjects ≥60 years of age, according to minimum JSW ≤2.0 mm or Croft grades 3–5°.
Self-reported pain and physical and occupational parameters
Summarised in Table 1.
Total hip replacements
In the mean 8.3-year follow-up period between 1992 and 2003, 66 subjects had had THR performed; 50 were for primary OA; a THR incidence of 146/100,000 persons for primary OA (20 THR/25 men and 30 THR/26 women). Of 264 hips at the outset of the study (1992) with minimum JSW ≤2.0 mm, THR had been performed in 25 hips (9.4%), and of 235 hips with Croft grades 3–5°, THR had been performed in 22 hips (9.3%).
Body mass index
BMI was significantly higher in men than women. However, BMI increased significantly more in women than men between 1976 and 1992 (Table 1). We found no significant relationships between BMI I (1976), BMI III (1992) or Δ BMI (1976–1992) and minimum JSW in men, but did find a significant relationship between Δ BMI and minimum JSW reduction in women (Table 2). It seems reasonable to conclude that weight loss may delay the age-related JSW reduction in women documented in several studies. We found significant relationships between BMI I (1976) and BMI III (1992) and self-reported hip pain and groin pain in both genders (p ranging from <0.001 to 0.04) while Δ BMI had no effect on self-reported pain in or around the hip joint. BMI I (1976) and BMI III (1992) were significantly higher in subjects of both genders undergoing THR (p<0.001). Even if joint degeneration develops over several years, it seems reasonable to conclude that cohort subjects undergoing THR between 1992 and 2003 already had comparatively higher BMI in 1976.
Multiple logistic regression analyses
The continuous variables of age, indices of hip dysplasia, years of varying exposure to repeated daily lifting, BMI I and Δ BMI were tested against Croft OA grades 3–5°, minimum JSW ≤2.0 mm, and ±THR by multiple regression analyses. The results are presented in Table 3. The significance level was set at 0.004. In summary: while the radiological OA indices of Croft grades 3–5° or minimum JSW ≤2.0 mm were significantly affected by the degree of hip dysplasia in men and hip dysplasia and age in women; the risk of THR being performed between 1992 and 2003 was only affected by BMI I assessed in 1976 in both genders.
Discussion
In this study, we investigated ageing, BMI, occupation and hip dysplasia as potential risk factors for (1) the development of radiological hip osteoarthritis, (2) self-reported hip pain and (3) the risk of THR. We found that ageing and hip dysplasia were significant risk factors for radiological hip OA in women and hip dysplasia alone a risk factor for radiological hip OA in men while occupation and BMI were not significant in either gender. With regard to THR, we found that increased BMI assessed 15 years before radiological examination was a significant risk factor for THR and hip pain. Furthermore, we found that weight loss observed during a mean follow-up period of 15.4 years did tend to delay JSW reduction in women. Occupational exposure to repeated daily lifting in this urban cohort was not found to be a significant risk factor for either radiological hip osteoarthritis or THR.
As mentioned earlier, individual orthopaedic surgeons have individual criteria for recommending patients for THR, and we do not find it reasonable in epidemiological studies to use THR as the end point for hip OA. Methodological inconsistencies have marked the clinical epidemiology of hip OA for decades. These difficulties have three main sources: (1) the use of urograms and colon radiographs as source material in hip OA studies [20]; (2) the use of radiological classifications such as Kellgren & Lawrence’s classification, which implicitly assume a chronological sequence of degeneration. This sequence has not been evident in the literature and puts comparatively too much weight on the formation of subchondral sclerosis and osteophytes, which are most commonly found in men, and postmenopausal hormone substitution in women [16]. Furthermore, global radiological OA classifications have generally poor intra- and inter-reader repeatability while the single assessment of JSW has high intra-class coefficients in most studies and has proven to reflect clinical status accurately [7, 8]; and (3) the hitherto ignorance of the normal age- and gender-related variation of JSW in asymptomatic subjects. Cut-off values of pathologically reduced minimum JSW have varied in the literature between 1.5 and 4.0 mm [6, 10]. In this and earlier studies, we used the recommendation by Lanyon et al. of a minimum JSW cut-off value of 2.0 mm, which equalises mean minimum JSW÷2 SD.
In this study, we found that relatively few cohort subjects with definite radiological hip OA had THR during a mean follow-up period of 8.3 years (25/264 with minimum JSW ≤2.0 mm=9.4%). Those who did had comparatively higher BMI and comparatively more hip pain. While weight or obesity have been found to be major risk factors for knee OA, the evidence of a consistent association between weight and hip OA has not been shown. Cooper et al. found that weight was a significant independent risk factor among 210 men and 401 women listed for THR [4]. In a study of 1,021 men and women listed for THR, Marks & Allegrande reached the same conclusion [19]. However, using radiological criteria of hip OA only, Tepper & Hochberg did not find an association between hip OA and weight or obesity [21]. In a systematic survey of the literature, Lievense et al. found a moderate association between weight and hip OA with odds ratios in the best-executed studies in the vicinity of 2.0 [18].
The relationship between heavy physical workloads over prolonged periods of time and the development of hip OA has been the focus of many studies. In a case-controlled study of occupational lifting and hip OA, Coggon et al. found no association among women but an association among men [3]. The strongest evidence of an association between excessive physical workloads and hip OA has been in rural populations, where mixed farming for decades has been related to hip OA development [1]. Again, studies were based on urograms.
In a previous longitudinal case-controlled study, we established that subjects with mild-to-moderate hip dysplasia do not report more pain than normal subjects [13]. While hip dysplasia is significantly associated to hip OA, we did not find an association between hip dysplasia and THR in this study.
We conclude that while radiological evidence of degeneration and treatment by THR are two sides of the same condition, they do not necessarily share the same risk factors, and caution should be exercised in epidemiological studies in attributing one or the other as the natural end point.
References
Axmacher B, Lindberg H (1993) Coxarthrosis in farmers. Clin Orthop 82–86
Coggon D, Croft P, Kellingray S, Barrett D, McLaren M, Cooper C (2000) Occupational physical activities and osteoarthritis of the knee. Arthritis Rheum 43:1443–1449
Coggon D, Kellingray S, Inskip H, Croft P, Campbell L, Cooper C (1998) Osteoarthritis of the hip and occupational lifting. Am J Epidemiol 147:523–528
Cooper C, Inskip H, Croft P, Campbell L, Smith G, McLaren M, Coggon D (1998) Individual risk factors for hip osteoarthritis: obesity, hip injury, and physical activity. Am J Epidemiol 147:516–522
Croft P, Cooper C, Wickham C, Coggon D (1990) Defining osteoarthritis of the hip for epidemiologic studies. Am J Epidemiol 132:514–522
Danielsson LG (1964) Incidence and prognosis of coxarthrosis. Acta Orthop Scand Suppl 66:1–61
Dougados M, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, Vignon E (1996) Radiological progression of hip osteoarthritis: definition, risk factors and correlations with clinical status. Ann Rheum Dis 55:356–362
Dougados M, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, Vignon E (1997) Radiographic features predictive of radiographic progression of hip osteoarthritis. Rev Rhum Br 64:795–803
Dougados M, Gueguen A, Nguyen M, Berdah L, Lequesne M, Mazieres B, Vignon E (1999) Requirement for total hip arthroplasty: an outcome measure of hip osteoarthritis? J Rheumatol 26:855–861
Hansson G, Jerre R, Sanders SM, Wallin J (1993) Radiographic assessment of coxarthrosis following slipped capital femoral epiphysis. A 32-year follow-up study of 151 hips. Acta Radiol 34:117–123
Heyman CH, Herndon CH (1950) Legg–Perthes disease. A method for the measurement of the roentgenographic result. J Bone Joint Surg Am 32:767–778
Jacobsen S, Sonne-Holm S, Lund B, Søballe K, Kiær T, Rovsing H, Monrad H (2004) Pelvic orientation and assessment of hip dysplasia in adults. Acta Orthop Scand 75:721–730
Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B (2005) Joint space width in hip dysplasia. J Bone Joint Surg Br Accepted for publication
Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B (2004) Factors influencing hip joint space in asymptomatic subjects. Osteoarthr Cartil 12:698–703
Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B (2004) The distribution and inter-relationships of radiologic features of osteoarthrosis of the hip. Osteoarthr Cartil 12:704–710
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthritis. Ann Rheum Dis 16:494–502
Lanyon P, Muir K, Doherty S, Doherty M (2003) Age and sex differences in hip joint space among asymptomatic subjects without structural change: implications for epidemiologic studies. Arthritis Rheum 48:1041–1046
Lievense AM, Bierma-Zeinstra SM, Verhagen AP, van Baar ME, Verhaar JA, Koes BW (2002) Influence of obesity on the development of osteoarthritis of the hip: a systematic review. Rheumatology 41:1155–1162
Marks R, Allegrante JP (2002) Body mass indices in patients with disabling hip osteoarthritis. Arthritis Res 4:112–116
Smith RW, Egger P, Coggon D, Cawley MI, Cooper C (1995) Osteoarthritis of the hip joint and acetabular dysplasia in women. Ann Rheum Dis 54:179–181
Tepper S, Hochberg MC (1993) Factors associated with hip osteoarthritis: data from the First National Health and Nutrition Examination Survey (NHANES-I). Am J Epidemiol 137:1081–1088
Tonnis D (1976) Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Ortop 119:39–47
Vingård, E (1991) Overweight predisposes to coxarthrosis. Acta Orthop Scand 62:106–109
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Orthop Scand Suppl 58:1–132, (Stockholm; P.A. Norstedt & Söner)
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacobsen, S., Sonne-Holm, S. Increased body mass index is a predisposition for treatment by total hip replacement. International Orthopaedics (SICOT) 29, 229–234 (2005). https://doi.org/10.1007/s00264-005-0658-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-005-0658-2