Abstract
We performed a morphological and histomorphometric analysis of the use of either autografts, or of frozen or freeze-dried cancellous bone allografts in sheep. A cancellous bone defect was created in the lateral portion of the distal epiphysis of the left femur. Four groups of six animals were monitored for 3 months. In the first group, the cavity was filled with autograft, in the second with frozen allograft and in the third with freeze-dried allograft. In the last group, the cavity was not filled and served as control. A study of the host bone showed that the mean trabecular width of the peripheral osteoid was greatest in the control group, while the number of osteoblasts and osteoclasts was significantly lower in the freeze-dried allograft group. However, the different bone grafts that were used to fill the cavity showed a greater trabecular width and area in the autografts. Among the frozen allografts, these measurements were also greater than in the freeze-dried allograft group. The "erosion surface" of the freeze-dried allograft group was also found to be three times greater, and there were a larger number of osteoclasts and osteoclastic nuclei. We concluded that the "lyophilised" allografts were re-absorbed rapidly and that there were no major morphological differences between the frozen allografts and the autograft groups.
Résumé
Nous avons fait une analyse morphologique et histomorphométrique d'autogreffe et d'allogreffes spongieuses congelées ou lyophilisées chez le mouton. Un défaut d'os spongieux a été créé dans la portion latérale de l'épiphyse fémorale distale gauche. Quatre groupes de six animaux ont été suivi trois mois. Dans le premier groupe la cavité a été remplie d'autogreffe, dans le second elle a été remplie avec de l'allogreffe congelée et dans le troisième avec de l'allogreffe lyophilisée. Dans le dernier groupe la cavité n'a pas été remplie et a servi comme contrôle. Une étude de l'os de l'hôte a montré que la largeur moyenne du trabecule de l'ostéoïde périphérique était plus grande dans le groupe témoin tandis que le nombre d'ostéoblastes et d'ostéoclastes était notablement inférieur dans le groupe d'allogreffe lyophilisée. Cependant les greffes différentes qui ont été utilisées pour remplir la cavité ont montré une plus grande largeur de trabécules avec une plus grande surface dans les autogreffes. Pour l'allogreffe congelée ces dimensions étaient plus grandes que pour l'allogreffe lyophilisée. La surface de résorption de l'allogreffe lyophilisée à aussi été trouvé pour être trois fois plus grande et il y avait un plus grand nombre d'ostéoclastes et de noyaux ostéoclastiques. Nous avons conclu que les allogreffes lyophilisées avaient été résorbés rapidement et qu'il n'y avait pas de différence morphologique majeure entre les allogreffes congelées et les autogreffes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autologous bone grafts constitute the most natural method for reconstructing skeletal defects and cavities as they maintain their osteoconductive and osteoinductive properties. This allows integration of the graft without any risk of transmitting disease. However, the supply of bone is limited, and there is a risk of morbidity at the donor site. A cancellous bone autograft stimulates the appearance of osteogenic cells. These form new bone from fibrous tissue and they also arrange themselves along the transplanted bone trabeculae creating new bone in this area [1, 3].
The freezing of allografts keeps bone viable for a long period. It reduces the chance of immune reactions and makes bone of the right size and amount available at any time. When harvesting bone tissue [11], a set of legal requirements and regulations must be met in order to prevent the transmission of disease.
While the biological activity of allografts is inferior to that of autografts, it does follow the same histological sequence but needs more time for total integration [4, 8].
Several alternatives have been developed in order to avoid the limitations and complications of the use of bone grafts. These include the use of bone marrow in combination with bone grafts, growth factors and bone-graft substitutes [6, 21, 23, 26, 30]. Bone marrow has been used in combination with bone grafts in order to stimulate bone formation in skeletal defects and non-unions [24], but its effectiveness depends on the activity of the stem cells in the bone marrow aspirate.
The sequence of bone repair is closely related to the local vascular supply [4, 9, 16], and cancellous bone with its porous structure re-vascularises more quickly than cortical bone [4]. This results from the gradual growth of vessels in the medullary cavities [16, 19].
Several factors influence tissue transplants, and these include the structure of the tissue, the methods of preservation and storage and also the method of sterilisation. Many different methods are currently being used to preserve and to store specimens until they are required for implantation. While freezing bone at −20°C does not completely arrest enzymatic degradation, preserving bone at −70 to −80°C or in liquid nitrogen does decrease the immunogenicity of the graft [11].
In order to determine how the host bone reacts during the incorporation of a graft in a cavity, studies both within the graft as well as around the edges of the host bone are necessary. To do this, we performed in the distal epiphysis of the femurs of sheep a morphological and histomorphometric analysis of the integration of autografts and frozen and freeze-dried cancellous bone grafts, together with the reaction of the peripheral host bone.
Materials and methods
Twenty-four sheep (Ovis aries) aged 4–6 months and weighing 25–30 kg were used in the study.
A 1 cm diameter trephine of 2 cm in length was used to create a cavity in the external portion of the distal epiphysis of the left femur. This was filled with three different types of cancellous bone grafts (fresh autograft, frozen allograft, freeze-dried allograft) in three groups respectively of six animals. The cavity was left unfilled in a fourth group of six, which served as controls.
The donor sheep were of the same breed as the receptor sheep. The autografts were reinserted "upside-down" into the newly created cavity (from which they had been taken) immediately after extraction. The frozen allografts were used after freezing at −80°C for 6 weeks. To obtain the freeze-dried grafts, we froze the grafts at −80°C for 6 weeks and then freeze-dried them with a lyophilizer (Heto, Brikerod, Denmark), which produced the autografts at 5.3 Pa of pressure. Ninety percent of their water content was then removed by drying at −55°C for 36 h.
To study the bone formation in the host bone, we used four different fluorochromes as bone markers. These were administered intra-muscularly according to the following schedule: 2 weeks after surgery, calcein (green) (Sigma-Aldrich, Madrid, Spain); 4 weeks after surgery, alizarin (red) (Sigma); 6 weeks after surgery, xylenol (orange) (Fluka, Riedel-de Haën). Then, 2 months after surgery, oxytetracycline (yellow) (Duphacycline, Laboratories IVEN, Madrid, Spain) was used.
The animals were sacrificed 3 months after surgery by an intravenous injection of 5 mEq of potassium chloride and under sodium pentobarbital anaesthesia (1.5 mg/kg weight). The distal end of the femur was then removed and the cylindrical defect was divided into two parts, one for embedding in paraffin and the other for embedding (un-decalcified) in polymethylmethacrylate (PMMA). For the histological study, the specimens were fixed in formaldehyde 4% for 24 h and then decalcified in a solution of PVP-EDTA at 4°C. Once they had been decalcified, they were dehydrated using alcohols of increasing proof (70%, 80%, 96% and 100%). After 4 h in xylene they were embedded in paraffin at a temperature of 60°C. Specimens were sectioned at 4 μm, and stained with Masson's trichrome, hematoxylin and eosin.
To analyse the mineralisation using fluorochromes, the specimens were fixed in formaldehyde for 1 week and then dehydrated by using alcohols of increasing proof. After 1 week in PMMA-alcohol and 3 weeks in PMMA (Technovit 7200 VLC, Nordenstadt, Germany), they were sectioned with a diamond saw (Exakt, Nordenstadt, Germany) and trimmed to a thickness of 12 μm. After measuring the sections with ultraviolet light, the distance between the bone markers was measured and the bone formation index calculated (distance μm/days). Finally, they were stained with von Kossa's stain.
We used an image-analysing system (Leica Q 500 MC, Leica Cambridge Ltd., Cambridge,UK) to determine the histomorphometric parameters. With Masson's trichrome stain, the following parameters were measured: trabecular width, trabecular surface, trabecular erosion surface, index of trabecular erosion, number of osteoblasts, number of osteoclasts per field, number of osteoclast nuclei, index of bone re-absorption or the number of osteoclast nuclei/osteoclasts. With von Kossa's stain, the following investigations were made: osteoid width and osteoid-trabecular index. Fluorescence was used to measure bone formation index.
Two zones were studied in each specimen, the edges of the host bone and of the graft. Eight measurements were obtained per zone for each animal in each group. The fluorochrome markings were only measured in the host bone, as these markings did not penetrate the grafts in a homogenous manner. The statistical study of the groups was carried out by means of a one way ANOVA followed by Tukey B and high significant difference (HSD) tests and using the SPSS 9.0 statistical package for Windows (SPSS Inc., Chicago, IL, USA).
Results
Histology
The cavities in the control group were found to contain fibrous tissue of variable density, which increased from the periphery to the centre. The fibres were better orientated in the middle of the cavity but did not form any clear pattern toward the edges. In the peripheral trabeculae, more regenerative activity was observed, with many osteoblasts and few osteoclasts around the trabeculae. The autografts showed a large quantity of trabecular tissue with obvious signs of vitality in the form of a large number of osteoblast cells around the edges. We found few osteoclasts inside this type of bone graft (Fig. 1). In the frozen allografts, abundant fibrous tissue was present between the trabeculae, even in the central area of the defect, but only a few areas of ossification were observed in the middle of the cavity (Fig. 2).
The freeze-dried allograft group was found to have sparse formation of trabeculae inside the cavity and no signs of vitality. Giant multi-nucleate osteoclasts could be seen, mainly around the periphery. There were also ample lymphocytic infiltrate and major osteoclastic activity, the latter being related to an increase in bone reabsorption (Fig. 3).
Bone histomorphometry
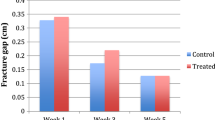
Trabecular width: Analysis of individual variables revealed very significant differences (p<0.01) between the frozen allograft and autograft groups on one hand and the freeze-dried allograft group on the other. In the host bone cavity edge, significant differences were found (p<0.05) between the trabecular width of the frozen allograft group and that of the control group (Table 1).
Trabecular surface: Highly significant differences were found (p<0.001) in the grafts between the freeze-dried group, which was the smallest, and the frozen and autograft groups. Around the host bone cavity edge, significant differences were found (p<0.05) between the frozen and autograft groups on the one hand and the control and freeze-dried graft groups on the other (Table 1).
Trabecular erosion surface: With regard to erosion defects, analysis of the individual variables in the cavity showed that the erosion surface in the freeze-dried graft group was three times greater than that in the autograft and frozen graft groups (p<0.001).
Index of trabecular erosion (%): Ratio of trabecular erosion surface and trabecular surface was 27.5% in the freeze-dried graft, 2.3% in the frozen allograft and 3.4% in the autograft. The differences between these groups were statistically very significant (p<0.01), with the greatest degree of erosion in the freeze-dried graft group.
Number of osteoblasts: The frozen allograft group was similar to the autograft group (18 osteoblasts per field), and both these numbers were higher than in the freeze-dried allograft group (5 osteoblasts per field). No significant differences between the frozen allograft and autograft were recorded, but highly significant differences (p<0.001) between these two groups and the freeze-dried graft group were noted. In the host bone cavity edge, highly significant differences (p<0.001) between the control group and the freeze-dried graft group were found, whereas there were no significant differences between the other groups (Table 1).
Number of osteoclasts per field: Statistically significant differences were found (p<0.05) inside the grafts between the autograft and the freeze-dried graft groups using analysis of individual variables. The freeze-dried group had the largest number of osteoclasts, and the smallest number was in the autograft group. In the host bone cavity edge, as inside the graft, statistically significant differences were found (p<0.05) between the autograft and the freeze-dried graft groups (Table 1).
Number of osteoclast nuclei: Highly significant differences were found (p<0.001) between the freeze-dried group, which had the largest number of nuclei, and the autograft and frozen groups. In the host bone cavity edge, statistically significant differences were found (p<0.05) between the autograft, control and frozen groups, and the freeze-dried group (Table 1).
Index of bone reabsorption: The ratio between the number of osteoclast nuclei and the number of osteoclasts per field was calculated. Inside the graft, this was much greater in the freeze-dried allograft group (11.41) than in the autograft (3.55) and in the frozen allograft (4.15) groups (p<0.001). However, in the host bone cavity edge, no statistically significant differences were found between the different groups (Table 1).
Osteoid width: No statistically significant differences were found between the groups. In the host bone cavity edge, statistically significant differences were found (p<0.05) between the autograft and freeze-dried graft groups, and the control group (Table 1).
Osteoid-trabecular index or ratio of the osteoid width and the trabecular width: In the graft, the differences were not statistically significant. In the host bone cavity edge, statistically significant differences appeared (p<0.05) between the control group and the freeze-dried and frozen graft groups, but there were no significant differences between the control group and the autograft group (Table 1).
Bone formation index: The process of bone formation in the host bone cavity edge, expressed by the bone formation index, was faster in the freeze-dried group than in the autografts, the control group, and the frozen allograft group, which in fact had the slowest bone formation (Table 1).
Discussion
As in earlier studies [8, 12, 20], we also found that in the cancellous bone graft the area and trabecular width of the freeze-dried group presented lower values than the control group, while the host bone of the control group presented lower values than in the freeze-dried group. In comparison with the results presented by Yano et al. [29], we found that the freeze-dried graft showed less osteogenic activity.
There were no striking histological differences between the frozen allograft and autograft groups, although it was noticeable that there was more bone regeneration activity in the former with an abundance of osteoblasts particularly in the peripheral areas.
The autograft has trabeculae that are each surrounded by a clear band of osteoblastic cells arranged in linear fashion, and the inter-trabecular spaces are occupied by a medullary tissue rich in vessels and blood cells. The osteocytes visible in the bone trabeculae all present a stained nucleus that proves their viability. Thus, this is a graft that adapts easily, is quickly integrated and follows a slow re-absorption process. The freeze-dried graft presents a smaller number of osteoblasts on its trabecular surface. The osteocytes of the allograft also present stained nuclei. As for the freeze-dried graft, its behaviour is radically different from that of the other two, as it is common to find abundant lymphocyte infiltrate with clear re-absorption of the graft leaving only small remains behind, which are reabsorbed immediately. In the autograft and the frozen graft, the activity observed is mainly osteoblastic, whereas in the freeze-dried graft the activity is osteoclastic.
Cancellous frozen bone graft is useful in orthopaedic surgery where there is bone loss because, as it consists of particulate cancellous bone and marrow, it can be used to fill irregular-shaped defects. These grafts have been widely studied and represent a minimal risk to the patient [11, 27]. Komender et al. [17] studied the influence of temperature on the mechanical properties of the graft and concluded that freezing at −78°C has no effect on the graft's mechanical properties. No changes were observed with torsion strength and high compression tests of bone allograft stored between −20°C and liquid nitrogen [22].
The main source of this kind of allograft is from femoral heads that have been removed during total hip replacement. The ease of procurement, the absence of complications and the success in achieving satisfactory fusion has led us to use "femoral-head allografts" in procedures such as scoliosis surgery, revision hip arthroplasty, etc.
In contrast to the results of Stevenson et al. [25], we found no re-absorption differences between cancellous bone allografts and autografts. In fact, the reaction of the host bone to these two kinds of graft was similar.
No major morphological differences were detected between the frozen allograft and autograft groups, although it was notable that there was more bone regeneration activity with an abundance of osteoblasts, above all around the periphery of the cavity [15].
The freeze-dried graft group was found to differ significantly from the other groups in that the graft was re-absorbed rapidly and with the appearance of osteoclasts or giant multi-nuclear cells. The literature is contradictory on this point [5, 10, 13, 14, 18], as some authors emphasise the osteoinductive properties of this type of graft [28], while others underline the poor results [7, 12] in both experimental and clinical studies. This is in agreement with the findings of our study.
The efficacy of the use of frozen cancellous bone allografts in clinical practice and their advantages are well known. Freezing had no obvious direct effect on incorporation of the graft, and the immunogenicity of the frozen cancellous bone allograft did not affect the outcome of the graft. In clinical terms, it is very important to bear in mind the different options available when bone grafting is indicated. We need grafts which combine synthetic scaffolds [2], or frozen allografts with biological properties which stimulate cell infiltration and new bone formation in order to avoid the limits of the autogenous cancellous bone imposed by morbidity and the quantity available.
References
Aspenberg P, Tägil M, Kristensson C, Lidin S (1996) Bone graft proteins influence osteoconduction. A titanium chamber study in rats. Acta Orthop Scand 67:377–382
Betz RR (2002) Limitations of autograft and allograft: new synthetic solutions. Orthopedics 25 [Suppl V]:561–570
Bruder SP, Fink DJ, Caplan AI (1994) Mesenchymal stem cells in bone development, bone repair, and skeletal regeneration therapy. J Cell Biochem 56:283–294
Burwell RG (1985) The function of bone marrow in the incorporation of a bone graft. Clin Orthop 200:25–141
Cook SD, Dalton JE, Prewett AB, Whitecloud TS (1995) In vivo evaluation of demineralized bone matrix as a bone graft substitute for posterior spinal fusion. Spine 20:877–886
Cook SD, Barrack RL, Shimmin A, Morgan D, Carvajal JP (2001) The use of osteogenic protein-1 in reconstructive surgery of the hip. J Arthroplasty 16 [Suppl I]: 88–94
Cornu O, Banse X, Docquier PL, Luyckx S, Delloye C (2000) Effect of freeze-drying and gamma irradiation on the mechanical properties of human cancellous bone. J Orthop Res 18:426–431
Czitrom AA (1992) Immunology of bone and cartilage allografts In: Czitrom AA, Gross AE (eds) Allografts in orthopaedic practice. Williams and Wilkins, Baltimore
DeLacure MD (1997) On the blood supply of microvascular bone transfers. Plast Reconstr Surg 99:356–365
Fabry G (1991) Allograft versus autograft bone in idiopathic scoliosis surgery: a multivariate statistical analysis. J Pediatr Orthop 11:465–468
Friedlaender GE (1991) Bone allografts: the biological consequences of immunological events. J Bone Joint Surg [Am] 73:1119–1122
Haas R, Haidvogl D, Donath K, Watzek G (2002) Freeze-dried homogeneous and heterogeneous bone for sinus augmentation in sheep. Part I: histological findings. Clin Oral Implants Res 13:396–404
Herron LD, Newman MH (1989) The failure of ethylene oxide gas sterilized freeze dried bone graft for thoracic and lumbar spinal fusion. Comments. Spine 14:496–500
Hopp SG, Dahners LE, Gilbert JA (1989) A study of the mechanical strength of long bone defects treated with various bone autograft substitutes: an experimental investigation in the rabbit. J Orthop Res 7:579–584
Kakiuchi M, Ono K (1996) Preparation of bank bone using defatting, freeze-drying and sterilization with ethylene oxide gas. Part II. Clinical evaluation of its efficacy and safety. Int Orthop 20:147–152
Kirkeby OJ (1991) Revascularisation of bone grafts in rats. J Bone Joint Surg [Br] 73:501–505
Komender J, Malczewska H, Komender A (1996) Bone banking for transplantation in orthopaedic reconstructions. Ann Transplant 1:70–72
Levine MJ, Boden SD (1996) Allograft and bone substitutes for the spine. Current Opinion in Orthopaedics 7: 41–47
Louisia S, Stromboni M, Meunier A, Sedel L, Petite H (1999) Coral grafting supplemented with bone marrow. J Bone Joint Surg [Br] 81:719–724
Mizutani A, Fujita T, Watanabe S, Sakakida K, Okada Y (1990) Experiments on antigenicity in allotransplanted cancellous bone. Int Orthop 14:243–248
Orr TE, Villars PA, Mitchell SL, Hsu HP, Spector M (2001) Compressive properties of cancellous bone defects in a rabbit model treated with particles of natural bone mineral and synthetic hydroxyapatite. Biomaterials 22:1953–1959
Pelker RP, Friedlander GE, Markham TC, Panjabi MM, Moen CJ (1984) Effects of freezing and freeze drying on biomechanical properties of rat bone. J Orthop Res 1:405–411
Rougraff BT, Kling TJ (2002) Treatment of active unicameral bone cysts with percutaneous injection of demineralized bone matrix and autogenous bone marrow. J Bone Joint Surg [Am] 84:921–929
Seitz WH, Froimson AI, Leb RB (1992) Autogenous bone marrow and allograft replacement of bone defects in the hand and upper extremities J Orthop Trauma 6:36–42
Stevenson S, Li XQ, Martin B (1991) The Fate of cancellous and cortical bone after transplantation of fresh and frozen tissue-antigen-matched and mismatched osteochondral allografts in dogs. J Bone Joint Surg [Am] 73:1143–1156
Tagil M, Jeppsson C, Aspenberg P (2000) Bone graft incorporation. Effects of osteogenic protein-1 and impaction. Clin Orthop 371:240–245
Tomford WW, Starkweather RJ, Goldman MH (1981) A study of the clinical incidence of infection in the use of banked allograft bone. J Bone Joint Surg [Am] 63:244–248
Wozney JM (2002) Overview of bone morphogenetic proteins. Spine 27(16) [Suppl I]: S2–S8
Yano H, Masumi S, Fukunaga T, Ikebe S (1993) Quantitative analysis of revascularization and new bone formation in experimental bone grafts. The use of an image input and processing system. Int Orthop 17:109–112
Yano H, Ohashi H, Kadoya Y, Kobayashi A, Yamano Y, Tanabe Y (2000) Histologic and mechanical evaluation of impacted morcellized cancellous allografts in rabbits: comparison with hydroxyapatite granules. J Arthroplasty 15:635–643
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leniz, P., Ripalda, P. & Forriol, F. The incorporation of different sorts of cancellous bone graft and the reaction of the host bone. A histomorphometric study in sheep. International Orthopaedics (SICOT) 28, 2–6 (2004). https://doi.org/10.1007/s00264-003-0461-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-003-0461-x