Abstract
The potential of mesenchymal stromal cells (MSCs) to inhibit anti-tumor immunity is becoming increasingly well recognized, but the precise steps affected by these cells during the development of an anti-tumor immune response remain incompletely understood. Here, we examined how MSCs affect the steps required to mount an effective anti-tumor immune response following administration of adenovirus Fas ligand (Ad-FasL) in the Lewis lung carcinoma (LL3) model. Administration of bone marrow-derived MSCs with LL3 cells accelerated tumor growth significantly. MSCs inhibited the inflammation induced by Ad-FasL in the primary tumors, precluding their rejection; MSCs also reduced the consequent expansion of tumor-specific T cells in the treated hosts. When immune T cells were transferred to adoptive recipients, MSCs impaired, but did not completely abrogate the ability of these T cells to promote elimination of secondary tumors. This impairment was associated with a modest reduction in tumor-infiltrating T cells, with a significant reduction in tumor-infiltrating macrophages, and with a reorganization of the stromal environment. Our data indicate that MSCs in the tumor environment reduce the efficacy of immunotherapy by creating a functional and anatomic barrier that impairs inflammation, T cell priming and expansion, and T cell function—including recruitment of effector cells.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Immunotherapy is an appealing modality to treat cancer because inaccessible and therapy-resistant tumors can be targeted and destroyed by immune effector cells. Clinically significant anti-tumor immunity can be reliably generated by delivering Fas ligand (FasL) locally into the tumor environment using replication-deficient adenovirus (Ad) vectors [1–5]. While the ectopically expressed FasL promotes destruction of the primary tumor through an innate response mediated by infiltrating macrophages and neutrophils [1, 6–8], the response to distant tumors is T cell-dependent [5, 7, 9]. A unique aspect of Ad-FasL-based immunotherapy is that efficacy is not dependent on Fas receptor (CD95) expression by tumor cells. Rather, neutrophil-mediated tumor cell death increases the amount of autoantigen debris, and FasL-dependent apoptosis of neutrophils induces interferon (IFN)-stimulated genes that are important for cross-presentation [10] and for the ensuing antigen-presenting cell (APC) activation [11]. Antigen presentation then leads to the activation of tumor-specific cytolytic T cells, which are the ultimate effectors that target metastatic disease distant to the site of FasL administration. Ad-FasL thereby triggers a systemic effect that allows expansion of tumor-specific T cells, limiting local recurrence and distant metastasis [5, 7, 9, 12]. Experimentally, this response can be evaluated by adoptive transfer [9], while clinically the response can be assessed based on prevention or delay of disease progression, including metastasis and relapse [2].
We recently translated this treatment to a spontaneous model of canine bone cancer where it enhanced the expected disease-free interval and overall survival by 60 % and led to long-term survival of >40 % of responding patients [2]. It was encouraging that an effective response was achievable in such a large percentage of treated dogs, and this compared favorably with the approximate 7–15 % of tumor-bearing rodents where there is tumor “escape” and progression after treatment with Ad-FasL [1, 9]. However, an immunosuppressive barrier might have diminished the capacity of immune effector cells to activate and expand, to migrate into the tumor, or to recognize tumor cells and kill them in the animals where a treatment effect was not observed. This dichotomy underscores the need to understand mechanisms that can lead to failure of this therapy specifically and of immune-based therapies in general.
Mesenchymal stromal cells (MSCs) form integral constituents of the tumor microenvironment. MSCs give rise to fibroblasts, pericytes, myofibroblasts, tumor-associated fibroblasts, and endothelial cells, which together produce interleukin (IL)-6, IL-10, chemokine C–C motif ligand (CCL)-5, vascular endothelial growth factor (VEGF), and other factors [13, 14]. They create a favorable environment for tumor growth and metastasis by modulating angiogenesis, inflammation and immunity. MSCs also are believed to promote immune tolerance; they display suppressive effects on both innate and humoral immune effector cells and increase the production or activity of regulatory T cells (Tregs) [14–16]. In fact, MSCs can help tumors break allogeneic barriers, and, when provided exogenously, they can ameliorate severe immune attack such as that seen in graft-versus-host disease [17, 18]. However, the precise role of stromal cells in maintaining an immunosuppressive environment in the tumor remains incompletely understood [14].
Here, we tested the hypothesis that mesenchymal stromal cells in the tumor microenvironment act at multiple levels to support an immunosuppressive barrier that attenuates inflammation, inhibits priming of tumor-specific T cells, and impedes infiltration into and killing of the tumor by immune effector cells.
Materials and methods
Cells
LL3 cells were obtained from ATCC (Manassas, VA) and maintained in culture as described [9]. Parental LL3 cells were modified to express firefly luciferase (Luc) and green fluorescent protein (GPF) using the Sleeping Beauty transposon system [19]. We cloned Luc/GFP+ cells by limiting dilution and established two independent clones, called LL3-G/L_H1 and LL3-G/L_H2, with two and five integration sites, respectively (Suppl. Fig. 1). Both clones showed growth kinetics comparable to the parental cell line in vitro; in addition, LL3-G/L_H2, which was selected based on its stronger signal for in vivo imaging, showed comparable capacity to form tumors in vivo (Suppl. Fig. 2). MSCs were obtained from a commercial source (Invitrogen/Life Technologies, Grand Island, NY) or prepared using conventional methods from bone marrow of 8-week-old C57BL/6 (B6) mice [19]. MSCs purchased commercially (passage 8) were thawed, passaged, and phenotyped following the manufacturer’s recommendations prior to use in experiments. Consistent with expected cellular phenotype, both primary and commercially obtained MSCs uniformly expressed high levels of CD44, CD90, CD29, and SCA-1 and were weakly positive for CD34. Fas expression in MSCs was confirmed by flow cytometry using the Jo2 antibody (BD Biosciences, San Jose, CA). These cells were used within the first 12 passages with similar results whether they were commercially obtained cells or generated from primary bone marrow cells. For some experiments, MSCs were transfected with an expression vector encoding tdTomato (generously provided by Dr. Dan Kaufman, University of Minnesota) or transduced with a lentivirus encoding RFP and expanded for 2 passages prior to selection of red fluorescent cells.
Production of Ad-FasL
The viral clone used for these studies has been described previously [2, 9, 20]. Briefly, HEK 293-crmA cells were infected with Ad-FasL. Infectious virus was purified from the cell cultures using routine CsCl banding methods and concentrated in stabilization buffer containing 50 % v/v glycerol.
Cell viability
Cells were evaluated by routine microscopy using an Olympus IX71 inverted microscope equipped with epifluorescence. Detachment from the plate and inability to form confluent monolayers were subjective indicators of reduced viability. Viability also was quantified with the MTS (3-(4, 5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) assay using CellTiter 96® AQueous One Solution Cell Proliferation Assay Kit (Promega, Madison, WI). Briefly, triplicate wells of 1 × 104 cells for each condition were cultured in 100 μl of complete medium in 96-well plates; after 24 and 48 h, 20 μl of MTS solution was added to each well and cells were incubated for another 4 h before measuring absorbance at 490 nm using a Wallac Victor2 1420 Multilabel Counter (Perkin Elmer, Waltham, MA).
In vivo tumor growth
A dose response (100,000–500,000 cells per mouse) was used to determine the growth kinetics of LL3-G/L and parental LL3 cells. For all other experiments, 500,000 tumor cells in 100 µl of sterile saline solution were inoculated subcutaneously into the left flank of B6 mice. Transduction of Ad-FasL into LL3 cells (500:1 multiplicity of infection) was used to promote tumor rejection in vivo and to generate anti-tumor responses [9, 21]. LL3 cells are impervious to Fas-mediated signaling and do not undergo apoptosis upon expression of or exposure to FasL [21]. As indicated in results, mice were administered 500,000 MSCs concomitantly with tumor cells in 200 µl of sterile saline solution and followed for 28–39 days until the experimental endpoint. For each variable, a minimum of 13 mice and a maximum of 29 mice in total were examined in seven separate experiments. For each experiment, the minimum and maximum numbers of animals receiving paired treatments were, respectively, three and eight. Each experiment was terminated based on the University of Minnesota Institutional Animal Care and Use Committee Guideline on Tumor Endpoint Criteria. Animals in each experiment were humanely killed at the time when the first animal in the cohort reached any endpoint criteria or within 24 h of reaching it at the latest. Data for each experiment were analyzed independently, except for results reporting rates of tumor engraftment and survival, which are presented as observations from pooled experiments.
Tumor growth was monitored using the Xenogen IVIS 100 imaging system (Caliper Life Sciences, Hopkinton, MA, USA) as described [22]. Briefly, animals were imaged 24 h after the initial injection and every 3–7 days thereafter to detect luciferase activity. Within 10 min after mice were injected with D-luciferin and anesthetized by isoflurane inhalation, images were taken and then analyzed with Living Image software (Caliper Life Sciences).
For adoptive transfers, T cells were isolated from donor spleens by negative selection as described previously [9] using the MACS Pan T-cell isolation system (Miltenyi Biotec, San Diego, CA). As we showed before [9], the different treatments did not significantly affect the total number of mononuclear cells recovered from spleens, the total number of lymphocytes present in the mononuclear cell preparations, or the final frequency or ratio of CD4 and CD8 cells obtained from the donors. Three million CD3+ cells were injected into the tail vein of four immunocompetent (wild type) B6 recipients per group and “parked” in the mice for 14 days, at which time the mice were challenged with LL3 cells as described above. Tumor volume was determined by measurement of cross-sectional diameters (length and width) using digital calipers, based on the formula L × W 2 × 0.52 [9].
Mice were housed, treated, and handled using stringent criteria of animal health and welfare with approval from and in accordance with guidelines of the University of Minnesota Institutional Animal Care and Use Committee (protocol 1102A95733).
Histopathology and immunohistochemistry
Tumors were fixed by immersion in 10 % neutral-buffered formalin for 24 h and subsequently transferred to 70 % ethanol for routine processing and long-term preservation. A board-certified veterinary pathologist (TDO) characterized the tissue histopathology in tumor sections, and when tumors were not grossly detectable, sections from the injection site were stained with hematoxylin and eosin. Inflammation and necrosis in the tumors were characterized using a semiquantitative scale (0–4+) where each section was assigned a score for each category, where 0 = none seen and where 1–4 were graded from minimal (1) to moderate (2) to abundant (3) to severe (4) using pathological criteria applicable to the tissue in question [2]. These pathological scores were then used to assess correlations with measured tumor volume.
Immunohistochemistry (IHC) to detect expression of CD3, Foxp3, B220, Gr-1, CD31, F4/80, arginase I/II [23], inducible nitrous oxide synthase (iNOS), IFNγ, macrophage chemoattractant protein-1 (MCP-1)/CCL2, Rantes/CCL5, IL-10, IL-17, and tumor growth factor-ß (TGF-ß) was done by the Comparative Pathology Shared Resource of the Masonic Cancer Center and by the BioNet Histology Research Laboratory of the University of Minnesota Academic Health Center. Quantification of T cells in IHC-stained sections was done using the Aperio system [24].
Statistics
Tumor growth over time was analyzed using repeated measures analysis of variance. Differences between paired samples were examined using the Student’s T test (for normally distributed populations) or the Mann–Whitney U test (for populations that were not normally distributed). Comparisons of tumor growth rate between and among groups were done using Fisher’s exact test. Correlation between variables was determined using the Pearson correlation.
Results
Mesenchymal stromal cells enhance growth and survival of syngeneic LL3 tumors
The potential for MSCs to inhibit specific phases in the generation of anti-tumor responses is not fully understood. To address this, we initially investigated how exogenous, bone marrow-derived murine MSCs affected growth of syngeneic LL3 tumor cells in immunocompetent B6 mice. In this model, LL3-G/L engraftment and survival were measurable at the experimental endpoint based on luminescent emission in 19 of 20 (95 %) mice receiving tumor cells alone. Administration of MSCs alone did not cause tumors in any animal (0 of 13). However, mice that were injected with MSCs and LL3-G/L cells at the same time showed significantly accelerated (p < 0.05) tumor growth with formation of larger tumors (Fig. 1a). MSCs labeled with tdTomato persisted in the tumor microenvironment admixed with LL3-G/L cells for the duration of the experiment (Fig. 1b).
MSCs enhance growth of LL3 cells and persist in the tumor environment. a Mice (4/group) were inoculated with tdTomato-labeled MSCs (5 × 105, dashed), LL3-G/L cells (5 × 105, dotted), or both (solid) as indicated in the legend, and tumor growth was measured using in vivo luciferase emission. LL3 tumor growth rate was accelerated, and size was significantly increased (p < 0.05) in mice that received MSCs. Similar data were obtained in seven independent experiments. b Photomicrographs were obtained using confocal fluorescent microscopy (merged images) from a representative tumor (frozen section) of a mouse inoculated with LL3-G/L cells+ MSCs. Green arrows denote LL3 cells and red arrows denote MSCs. Nuclei are counterstained with DAPI. Unlabeled cells represent host stroma
Mesenchymal stromal cells are resistant to FasL-mediated cell death and interfere with FasL-mediated rejection of primary tumors
The intratumoral Ad-FasL system allowed us to examine the effect of MSCs on primary tumor rejection and on expansion of tumor-specific T cells in the host, and on T cell-mediated killing in adoptive recipients [1]. First, we established whether MSCs were sensitive to FasL in vitro, as we surmised that if FasL led to apoptosis of MSCs, they would be unlikely to interfere with the therapeutic effects of FasL. MSCs were cultured side by side with Fas-sensitive indicator OSCA-32 canine osteosarcoma cells as a control [2]. Figure 2a shows that transduction of MSCs and OSCA-32 cells with Ad5 was comparable. However, unlike OSCA-32 cells that died rapidly upon exposure to Ad-FasL (Fig. 2a) or to trimeric recombinant Super-FasL (Fig. 2b), MSCs did not show either morphologic evidence of apoptosis (Fig. 2a) or decreased viability (Fig. 2b). MSCs expressed comparable levels of Fas receptors on their surface to splenocytes (Suppl. Fig. 3), suggesting that resistance to FasL-mediated apoptosis was due to intrinsic mechanisms unrelated to Fas receptor expression [21, 25, 26].
MSCs are resistant to apoptosis mediated by trimeric “Super-FasL.” a OSCA-32 cells and MSCs were cultured in 6-well plates for 18 h followed by transduction with Ad-mCherry or Ad-FasL-mCherry. Phase contrast (left) and epifluorescent (right) photomicrographs were taken 24 h later. Magnification ×100. b OSCA-32 cells and MSCs were cultured in 96-well plates in the presence of increasing concentrations (0–2 ng/ml) of trimeric, soluble FasL (“Super-FasL”). Cell viability was determined at 24 and 48 h using the MTS assay
The resistance to FasL-mediated death suggested that MSCs could interfere with Ad-FasL immunotherapy. Thus, we assessed the effect of MSCs on rejection of primary tumors induced by ectopic Ad-FasL. Mice received LL3-G/L cells transduced with Ad-Cherry (control) or LL3-G/L cells transduced with Ad-FasL with or without concurrent administration of MSCs. Luminescent emission signals detectable in mice from each group at day +1 (24 h after injection) were equivalent. The average area for each group (photons) ranged from 4.1 × 105 (±2.9 × 105) to 6.3 × 105 (±7.0 × 105). A small but significant increase (p = 0.03) in tumor growth was detectable within a week in mice that received LL3-G/L cells alone, whereas significant regression (p = 0.002) to levels at or below the threshold of detection for luciferase activity was noted within 5–8 days in mice that received LL3-G/L cells transduced with Ad-FasL (Fig. 3a). A significant increase (p = 0.003) in tumor growth was seen in mice that received both LL3-G/L cells and MSCs as compared to mice that received LL3-G/L cells alone, which was consistent with the effect of MSCs to accelerate tumor growth described above (Fig. 1a). Finally, a significant increase in tumor growth also was seen in mice that received LL3-G/L cells transduced with Ad-FasL and MSCs together, as compared to mice that received LL3-G/L cells alone (p = 0.003), as well as mice that received LL3-G/L cells transduced with Ad-FasL (p = 0.0005) (Fig. 3a). The rate of progression was variable, with some mice showing only modest increases in tumor growth and some mice showing dramatic acceleration of tumor growth. These findings persisted throughout the course of disease progression, with mice receiving LL3-G/L cells transduced with Ad-FasL showing significantly reduced (p < 0.001) or absent tumor burden as compared to mice that received LL3-G/L cells alone and mice receiving LL3-G/L cells and MSCs, with or without Ad-FasL showing significantly greater (p = 0.05) tumor growth (Fig. 3b). In general, tumor size was inversely correlated to the observed degree of tumor inflammation (Pearson correlation—0.7).
MSCs inhibit tumor rejection by FasL in primary recipients. a Dot plot showing luminescence for individual mice (groups of 5) injected with LL3-G/L cells, LL3-G/L cells transduced with Ad-FasL, LL3-G/L cells and MSCs, or LL3-G/L cells transduced with Ad-FasL and MSCs after 8 days. The dotted line represents the threshold of detectable luciferase emission after a 5-min exposure. Data show one of the seven experiments done with comparable results. *p = 0.03 when compared to emission at day 1. **p < 0.003 when compared to emission at day 1. ‡ p = 0.05; ‡‡ p = 0.01. b Bar graph showing mean (±SD) tumor volume for each group of mice at the experimental endpoint (day 36). Data show one of the five experiments done with comparable results. ‡ p = 0.05; ‡‡ p = 0.01. Tumor burden measured by luminescent emission or based on tumor volume was significantly lower (p < 0.01) in mice that received LL3-G/L cells transduced with Ad-FasL than in mice from all other conditions
Mesenchymal stromal cells interfere with expansion of tumor-specific T cells
We addressed both T cell expansion in the primary host and effective T cell-dependent killing through adoptive transfer experiments. The frequency of tumor-specific T cells in a naïve host is below the effective level that can reject a tumor; therefore, when cells are injected into a syngeneic host, a tumor will form with predictable kinetics (see Fig. 1; Suppl. Fig. 2). Tumor rejection in the primary host in the Ad-FasL system is mediated both by innate inflammation and subsequent adaptive immunity [1, 5, 7, 9, 21]. Thus, clonal expansion of tumor-specific T cells induced by this inflammation can be assessed by re-challenging the same animal, or in a “cleaner” experiment, by adoptive transfer of these cells into a naïve host that can be T cell-deficient or T cell replete. T cell-deficient recipients generally improve the outcome because the adoptively transferred cells can undergo homeostatic expansion and do not need to compete against endogenous T cells. There also are no endogenous Tregs in this system. Hence, immunoreplete recipients were used for these experiments in order to provide the most rigorous means to confirm expansion of tumor-specific T cells in the donors.
We challenged donors with LL3 cells transduced with control adenovirus or with Ad-FasL, and with or without concurrent administration of MSCs. After 21 days, 3 × 106, T cells were isolated from donor spleens, transferred into adoptive recipients, and “parked” for 2 weeks prior to re-challenge with LL3 cells with or without MSCs (Fig. 4a). LL3 tumors grew unencumbered in recipient mice receiving adoptively transferred naïve T cells. Exposure to LL3 cells in the donors was similarly insufficient to generate a T cell response that could reproducibly reject tumors in the adoptive recipients. In contrast, providing Ad-FasL with the tumor (which promoted tumor rejection, Fig. 3) to the donor hosts significantly reduced (p = 0.04) tumor growth in the adoptive recipients. In this experiment, one of the four animals showed tumor escape and developed a ~400 mm3 tumor (approximately the same size as the median for animals in Groups 1 and 2). The presence of MSCs in the primary host tumor inhibited T cell priming, T cell expansion, or both: T cells from donors that received LL3 cells transduced with Ad-FasL concurrently with MSCs were less effective at controlling tumor growth in the adoptive recipient (compare Fig. 4a, Groups 3 and 5). It is important to note that despite the inability of FasL to create an innate response that could eliminate the primary tumor when donor mice received MSCs (Fig. 3), a T cell response that showed therapeutic benefit was observed in the adoptive transfer setting where tumor growth was significantly retarded in the recipients (compared to mice that received naïve T cells), even though every mouse in Group 5 developed small, measurable tumors (~100–200 mm3). It is also worth noting that in this case, no MSCs were administered to the recipient mice, so the effect of the exogenous MSCs could only have occurred in the primary hosts.
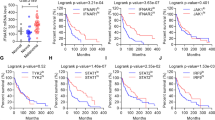
MSCs inhibit T cell expansion in primary hosts and infiltration of tumors by immune effector cells in secondary hosts. a Primary hosts were challenged with LL3 tumor cells with or without Ad-FasL and MSCs as indicated (T cell source or donor). After 14 days, spleen cells were harvested from donors, and T cells prepared using magnetic beads (>98 % pure) were adoptively transferred to immunocompetent recipients. After 14 days, the recipients were challenged with LL3 tumor cells with or without MSCs and followed for 36 days. At the end of the experiment, tumors were harvested to determine tumor volume and for histologic analysis. Dot plot shows tumor burden for individual mice in each group. *p < 0.05. b T cells in tumor sections from mice in Groups 5 and 6 from (a) were quantified using an Aperio system in sections stained with anti-CD3. Results were similar when the escaped tumor from Group 3 (a) was compared to tumors from Group 4. *p < 0.05
Mesenchymal stromal cells inhibit T cell-mediated tumor killing and alter the organization of the tumor environment
This approach also allowed us to examine the effect of MSCs on T cell-mediated tumor killing and on infiltration of immune effector cells into the tumor. For this, we compared conditions where the adoptively transferred T cells rejected or reduced tumor cell growth in the recipients (Fig. 4a, and Groups 3 and 5) to those where MSCs were provided to recipients along with tumor cells (Fig. 4a, Groups 4 and 6). In both conditions, there was increased tumor growth beyond the respective controls, suggesting that adoptively transferred T cells were unable to mount effective anti-tumor responses when MSCs were co-administered with tumor cells to the recipients.
To address the mechanisms that accounted for this effect of MSCs, we evaluated tumor necrosis and inflammation in H&E-stained slides [2, 21], and we used IHC to examine the cellular composition of the tumors. Inflammatory tumor infiltrates included relatively few Tregs, B cells, and granulocytes in all of the mice, with no difference between groups of recipients that did or did not receive MSCs with the secondary tumor challenge (Suppl. Fig. 4). As shown in Fig. 4b, there was a small but significant difference in the number of total T cells found in tumors of recipient mice that received MSCs (Groups 4 and 6) and those mice that did not (Groups 3 and 5). We did not believe that the relatively small difference in T cell numbers was sufficient to explain the dramatic differences in tumor growth and instead considered that the effect of T cells might be indirect or that the MSCs were affecting other aspects of tissue organization or tumor growth. There were no differences in the amount or intensity of CD31 staining (microvascular density, Suppl. Fig. 4). However, the distribution of T cells in tumors of recipient mice that received MSCs (Groups 4 and 6) was suggestive of vascular retention, while T cells in tumors from mice that did not receive MSCs (Groups 3 and 5) supported stromal infiltration (Suppl. Fig. 4). There were also quantitative and topographic differences in the staining patterns, suggesting that the anatomic organization of the tumor was different in the presence of MSCs. The most striking difference between these groups was tumor infiltration by host macrophages (Fig. 5).
MSCs alter the organization of the tumor environment. Tumors from two representative mice of Groups 5 and 6 from Fig. 4a were immunostained for infiltrating macrophages (F4/80), for arginase-producing cells, and for iNOS-producing cells. Similar results were seen when the escaped tumor from Fig. 4a, Group 3 was compared to tumors from Fig. 4a, Group 4
Heavy macrophage infiltrates were present at the periphery and extended into the stroma of tumors from mice that received T cells from Ad-FasL-treated donors, but they were greatly reduced or absent from the periphery and stroma of tumors from recipient mice that received MSCs. We examined whether levels and localization of pro-inflammatory and chemotactic cytokines IL-17, IFNγ, Rantes/CCL5, and MCP-1/CCL2, or anti-inflammatory cytokines IL-10 and TGF-ß could account for these differences. The data showed that, at least at the tumor endpoint, exogenous MSCs did not appreciably reduce the number of mononuclear cells producing IFNγ or MCP-1/CCL2, and they did not significantly alter the number of IL-17+ lymphocytes or IL-17+ endothelial cells in the tumor environment. No IL-10-producing cells were detectable in LL3 tumors regardless of whether the mice had been treated with T cells or MSCs. Finally, both tumor cells and other components of the tumor environment showed strong immunoreactivity against Rantes/CCL5 and TGF-ß, but the levels of these cytokines were also unaffected by the presence of exogenous MSCs in the tumor.
Unlike the relatively stable environment seen with regard to these common immunomodulatory cytokines, we observed somewhat unexpectedly that arginase-producing cells and iNOS-producing cells were abundant in tumors from mice that received T cells from Ad-FasL-treated donors and that they were greatly reduced or absent in tumors from recipient mice that received MSCs (Fig. 5). The arginase- and iNOS-producing cells mostly remained near the periphery of the tumors, and while their identity as host macrophages or myeloid cells, stromal cells, and/or tumor cells remains to be determined, it was apparent that these putative immunomodulatory cells did not abrogate anti-tumor activity of the adoptively transferred T cells or their capacity to recruit host immune effector cells.
Discussion
The potential of mesenchymal stromal cells (MSCs) to inhibit anti-tumor immunity is becoming increasingly well recognized, but the precise steps affected by these cells during the development of an anti-tumor immune response remain incompletely understood. Here, we examined how MSCs affect the steps required to mount an effective anti-tumor immune response upon generation of an anti-tumor immune response using intratumoral Ad-FasL.
Consistent with previous findings [15, 27–31], our data show that concurrent administration of MSCs enhanced growth of syngeneic Lewis lung carcinoma and that intratumoral Ad-FasL promoted rejection of the primary tumor and led to the generation of systemic, anti-tumor immunity [1]. Furthermore, our results indicate that tumor-specific T cells promoted significant infiltration of the tumor by host (recipient-derived) macrophages and other effector cells and that the presence of exogenous MSCs, which are impervious to FasL-mediated signals, created a functional or anatomic barrier that diminished the capacity of T cells to recruit and activate such effector cells.
Our data show for the first time how MSCs affect different aspects in the development of transplantable anti-tumor immunity. Specifically, (1) MSCs abrogated innate inflammation initiated by FasL in the tumor environment, thus preventing rejection of the primary tumor. (2) Yet, it was all the more surprising that despite this robust impairment of innate inflammation and tumor rejection, the mice receiving Ad-FasL were still able to generate a T cell response that showed therapeutic benefit in the adoptive transfer setting. (3) But again, co-administration of exogenous MSCs with tumor cells to adoptive recipients undermined tumor rejection by primed T cells, potentially by modulating the functional and anatomic organization of the tumor environment.
FasL can play multiple roles in the tumor environment. Almost two decades ago, a series of landmark papers proposed that expression of FasL by tumor cells could prevent immune-mediated tumor rejection by eliminating activated T cells [32–34], while, at the same time, expression of ectopic FasL in the tumor environment was shown to promote tumor rejection [5–7, 35, 36]. Subsequently, we and others have shown that this anti-tumor effect requires robust inflammation [2, 5, 8, 21], so the effect of MSCs to abrogate this response is consistent with their broad anti-inflammatory function [37–40]. Even though FasL administration failed to prevent rejection in primary hosts that received exogenous MSCs, the expansion of tumor-specific T cells in these donor mice was sufficient to provide partial control of tumor burden in adoptive recipients. MSCs have been shown to suppress migration, maturation, and antigen presentation by dendritic cells [41]; nevertheless, our data suggest that intratumoral Ad-FasL operates as a type of checkpoint blockade, allowing tumor-specific T cells to undergo activation and expansion even when inflammation is abated and supporting the notion that immunologic approaches will be most effective when combined with strategies to reduce tumor burden [2, 42].
Our adoptive transfer experiments show that MSCs caused profound suppression of adaptive, T cell-mediated events necessary for tumor rejection. Several mechanisms could account for this observation, including secretion of immunosuppressive cytokines [43], recruitment of regulatory T cells [44] or macrophages that display regulatory, immunosuppressive phenotypes [45, 46], direct inhibition of T cell proliferation [47], or even expression of FasL by MSCs, which can induce apoptosis of activated T cells [48]. However, these immunosuppressive properties may not be intrinsic to MSCs. Experimental data show that IFNγ or tumor necrosis-α (TNFα)-dependent licensing is necessary for these cells to alter the inflammatory environment, inhibit T cell activation, and promote tumor growth [49–53]. In particular, Chinnadurai et al. [49] showed that MSCs led to increased expression of inhibitory B7-related molecules B7H1 and B7DC; Han et al. [51] showed that licensing of MSCs was required for production of iNOS and immunosuppression; and Kraman et al. [52] showed that IFNγ and TNFα reversed hypoxia-induced ablation of FAP-expressing stromal cells from the tumor microenvironment and that these cells in turn inhibited antigen-specific anti-tumor immunity. The implication that T cell activation is necessary to promote licensing of MSCs should not be underappreciated. In fact, Ling et al. [54] showed that MSCs alone did not enhance tumor burden in T cell- and B cell-deficient Rag−/− mice, and our data show that the IFNγ, IL-17, MCP-1/CCL2, and Rantes/CCL5 in the tumor environment were unaffected by exogenous MSCs, and so these cytokines would thus be available to license exogenous or endogenous stromal cells.
In this light, the observation that tumor control was associated with tumor-promoting cellular infiltrates including macrophages and arginase- and iNOS-producing cells is uniquely interesting. Our interpretation is that reorganization of the tumor microenvironment, rather than the presence of unique cell populations, is essential to create an effective immunosuppressive barrier. We propose that interactions among the components of this environment are dynamic processes influenced by the cellular players and by the magnitude and type of inflammation [55]. Thus, our working model (Fig. 6) is that MSCs inhibit inflammation and they diminish, but do not abrogate, the process of T cell priming. Concomitantly, MSCs limit infiltration of activated T cells into the tumor, which results in failure to attract macrophages and other host effector cells that are necessary to mold the microenvironment to contain and eventually eliminate the tumor.
Working model for MSC-mediated inhibition of anti-tumor immunity. Schematic illustration of the effect of Ad-FasL to promote inflammation with subsequent generation of transplantable, specific anti-tumor immunity. MSCs inhibit FasL-induced rejection of the primary tumor and attenuate priming and T cell expansion in donor mice. Reorganization of the tumor environment in recipient mice by MSCs inhibits T cell-dependent killing and infiltration by host effector cells. Mouse images were obtained from royalty-free, public domain B6 mouse clip art (www.clker.com)
The exclusion of T cells from the tumor microenvironment and conceptual approaches to attack immune privilege were the subject of a recent, thorough review by Joyce and Fearon [56]. Strategies such as intratumoral Ad-FasL and systemic immune checkpoint blockade have the potential to overcome critical components of immune privilege and enable greater success for cancer patients receiving immunotherapy.
Abbreviations
- Ad:
-
Adenovirus
- APC:
-
Antigen-presenting cell
- CCL:
-
Chemokine C–C motif
- FasL:
-
Fas ligand
- GFP:
-
Green fluorescent protein
- IFN:
-
Interferon
- IHC:
-
Immunohistochemistry
- IL:
-
Interleukin
- iNOS:
-
Inducible nitrous oxide synthase
- LL3:
-
Lewis lung carcinoma cells
- LL3-G/L:
-
Lewis lung carcinoma cells expressing green fluorescent protein and luciferase
- Luc:
-
Luciferase
- MSC:
-
Mesenchymal stromal cell
- MTS:
-
(3-(4, 5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium)
- Treg:
-
Regulatory T cell
References
Modiano JF, Lamerato-Kozicki AR, Jubala CM, Coffey D, Borakove M, Schaack J, Bellgrau D (2004) Fas ligand gene transfer for cancer therapy. Cancer Ther. 2: 561–570. http://cancer-therapy.org/CT/v2/A/59.%20Modiano%20et%20al,%20561-570.pdf
Modiano JF, Bellgrau D, Cutter GR et al (2012) Inflammation, apoptosis, and necrosis induced by neoadjuvant fas ligand gene therapy improves survival of dogs with spontaneous bone cancer. Mol Ther 20:2234–2243. doi:10.1038/mt.2012.149
Ho MY, Sun GH, Leu SJ, Ka SM, Tang SJ, Sun KH (2008) Combination of fasl and gm-csf confers synergistic antitumor immunity in an in vivo model of the murine lewis lung carcinoma. Int J Cancer 123:123–133. doi:10.1002/ijc.23474
Norris JS, Bielawska A, Day T et al (2006) Combined therapeutic use of adgfpfasl and small molecule inhibitors of ceramide metabolism in prostate and head and neck cancers: a status report. Cancer Gene Ther 13:1045–1051. doi:10.1038/sj.cgt.7700965
Shimizu M, Fontana A, Takeda Y, Yagita H, Yoshimoto T, Matsuzawa A (1999) Induction of antitumor immunity with fas/apo-1 ligand (cd95l)-transfected neuroblastoma neuro-2a cells. J Immunol. 162:7350–7357
Arai H, Gordon D, Nabel EG, Nabel GJ (1997) Gene transfer of fas ligand induces tumor regression in vivo. Proc Natl Acad Sci U S A 94:13862–13867
Seino K, Kayagaki N, Okumura K, Yagita H (1997) Antitumor effect of locally produced cd95 ligand. Nat Med 3:165–170
Hohlbaum AM, Gregory MS, Ju ST, Marshak-Rothstein A (2001) Fas ligand engagement of resident peritoneal macrophages in vivo induces apoptosis and the production of neutrophil chemotactic factors. J Immunol 167:6217–6224
Jubala CM, Lamerato-Kozicki AR, Borakove M et al (2009) Mhc-dependent desensitization of intrinsic anti-self reactivity. Cancer Immunol Immunother 58:171–185. doi:10.1007/s00262-008-0535-0
Le Bon A, Tough DF (2008) Type i interferon as a stimulus for cross-priming. Cytokine Growth Factor Rev 19:33–40. doi:10.1016/j.cytogfr.2007.10.007
Spel L, Boelens JJ, Nierkens S, Boes M (2013) Antitumor immune responses mediated by dendritic cells: How signals derived from dying cancer cells drive antigen cross-presentation. Oncoimmunology 2:e26403. doi:10.4161/onci.26403
Hohlbaum AM, Saff RR, Marshak-Rothstein A (2002) Fas-ligand–iron fist or achilles’ heel? Clin Immunol 103:1–6
Lin WW, Karin M (2007) A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest 117:1175–1183. doi:10.1172/JCI31537
Bergfeld SA, DeClerck YA (2010) Bone marrow-derived mesenchymal stem cells and the tumor microenvironment. Cancer Metastasis Rev 29:249–261. doi:10.1007/s10555-010-9222-7
Djouad F, Plence P, Bony C, Tropel P, Apparailly F, Sany J, Noel D, Jorgensen C (2003) Immunosuppressive effect of mesenchymal stem cells favors tumor growth in allogeneic animals. Blood 102:3837–3844. doi:10.1182/blood-2003-04-1193
Prevosto C, Zancolli M, Canevali P, Zocchi MR, Poggi A (2007) Generation of cd4+ or cd8+ regulatory t cells upon mesenchymal stem cell-lymphocyte interaction. Haematologica 92:881–888
Lazarus HM, Koc ON, Devine SM et al (2005) Cotransplantation of hla-identical sibling culture-expanded mesenchymal stem cells and hematopoietic stem cells in hematologic malignancy patients. Biol Blood Marrow Transplant 11:389–398. doi:10.1016/j.bbmt.2005.02.001
Zhou H, Guo M, Bian C, Sun Z, Yang Z, Zeng Y, Ai H, Zhao RC (2010) Efficacy of bone marrow-derived mesenchymal stem cells in the treatment of sclerodermatous chronic graft-versus-host disease: clinical report. Biol Blood Marrow Transplant 16:403–412. doi:10.1016/j.bbmt.2009.11.006
Tolar J, Nauta AJ, Osborn MJ et al (2007) Sarcoma derived from cultured mesenchymal stem cells. Stem Cells 25:371–379. doi:10.1634/stemcells.2005-0620
Leon RP, Hedlund T, Meech SJ, Li S, Schaack J, Hunger SP, Duke RC, DeGregori J (1998) Adenoviral-mediated gene transfer in lymphocytes. Proc Natl Acad Sci U S A 95:13159–13164
Modiano JF, Sun J, Lang J et al (2004) Fas ligand-dependent suppression of autoimmunity via recruitment and subsequent termination of activated t cells. Clin Immunol 112:54–65
Kim JH, Frantz AM, Anderson KL et al (2014) Interleukin-8 promotes canine hemangiosarcoma growth by regulating the tumor microenvironment. Exp Cell Res 323:155–164. doi:10.1016/j.yexcr.2014.02.020
Ino Y, Yamazaki-Itoh R, Oguro S, Shimada K, Kosuge T, Zavada J, Kanai Y, Hiraoka N (2013) Arginase ii expressed in cancer-associated fibroblasts indicates tissue hypoxia and predicts poor outcome in patients with pancreatic cancer. PLoS ONE 8:e55146. doi:10.1371/journal.pone.0055146
Rizzardi AE, Johnson AT, Vogel RI, Pambuccian SE, Henriksen J, Skubitz AP, Metzger GJ, Schmechel SC (2012) Quantitative comparison of immunohistochemical staining measured by digital image analysis versus pathologist visual scoring. Diagn Pathol 7:42. doi:10.1186/1746-1596-7-42
Ferrarini M, Imro MA, Sciorati C, Heltai S, Protti MP, Pellicciari C, Rovere P, Manfredi AA, Rugarli C (1999) Blockade of the Fas-triggered intracellular signaling pathway in human melanomas is circumvented by cytotoxic lymphocytes. Int J Cancer 81:573–579
Tourneur L, Mistou S, Michiels FM, Devauchelle V, Renia L, Feunteun J, Chiocchia G (2003) Loss of FADD protein expression results in a biased Fas-signaling pathway and correlates with the development of tumoral status in thyroid follicular cells. Oncogene 22:2795–2804. doi:10.1038/sj.onc.1206399
Djouad F, Bony C, Apparailly F, Louis-Plence P, Jorgensen C, Noel D (2006) Earlier onset of syngeneic tumors in the presence of mesenchymal stem cells. Transplantation 82:1060–1066. doi:10.1097/01.tp.0000236098.13804.0b
Wang H, Cao F, De A, Cao Y, Contag C, Gambhir SS, Wu JC, Chen X (2009) Trafficking mesenchymal stem cell engraftment and differentiation in tumor-bearing mice by bioluminescence imaging. Stem Cells 27:1548–1558. doi:10.1002/stem.81
Li H, Feng Z, Tsang TC et al (2014) Fusion of hepg2 cells with mesenchymal stem cells increases cancerassociated and malignant properties: an in vivo metastasis model. Oncol Rep 32:539–547. doi:10.3892/or.2014.3264
Zhang P, Dong L, Long H, Yang TT, Zhou Y, Fan QY, Ma BA (2014) Homologous mesenchymal stem cells promote the emergence and growth of pulmonary metastases of the rat osteosarcoma cell line UMR-106. Oncol Lett 8:127–132. doi:10.3892/ol.2014.2127
Zhu Q, Zhang X, Zhang L et al (2014) The il-6-stat3 axis mediates a reciprocal crosstalk between cancer-derived mesenchymal stem cells and neutrophils to synergistically prompt gastric cancer progression. Cell Death Dis 5:e1295. doi:10.1038/cddis.2014.263
Hahne M, Rimoldi D, Schroter M et al (1996) Melanoma cell expression of fas(apo-1/cd95) ligand: implications for tumor immune escape. Science 274:1363–1366
O’Connell J, O’Sullivan GC, Collins JK, Shanahan F (1996) The fas counterattack: fas-mediated t cell killing by colon cancer cells expressing fas ligand. J Exp Med 184:1075–1082
Villunger A, Egle A, Marschitz I, Kos M, Bock G, Ludwig H, Geley S, Kofler R, Greil R (1997) Constitutive expression of Fas (apo-1/cd95) ligand on multiple myeloma cells: a potential mechanism of tumor-induced suppression of immune surveillance. Blood 90:12–20
Hedlund TE, Meech SJ, Srikanth S, Kraft AS, Miller GJ, Schaack JB, Duke RC (1999) Adenovirus-mediated expression of fas ligand induces apoptosis of human prostate cancer cells. Cell Death Differ 6:175–182. doi:10.1038/sj.cdd.4400477
Shimizu M, Yoshimoto T, Nagata S, Matsuzawa A (1996) A trial to kill tumor cells through fas (cd95)-mediated apoptosis in vivo. Biochem Biophys Res Commun 228:375–379
Pulavendran S, Vignesh J, Rose C (2010) Differential anti-inflammatory and anti-fibrotic activity of transplanted mesenchymal vs. hematopoietic stem cells in carbon tetrachloride-induced liver injury in mice. Int Immunopharmacol 10:513–519. doi:10.1016/j.intimp.2010.01.014
Geng Y, Zhang L, Fu B et al (2014) Mesenchymal stem cells ameliorate rhabdomyolysis-induced acute kidney injury via the activation of m2 macrophages. Stem Cell Res Therapy 5:80. doi:10.1186/scrt469
Ryu KH, Kim SY, Kim YR, Woo SY, Sung SH, Kim HS, Jung SC, Jo I, Park JW (2014) Tonsil-derived mesenchymal stem cells alleviate concanavalin a-induced acute liver injury. Exp Cell Res 326:143–154. doi:10.1016/j.yexcr.2014.06.007
Song X, Xie S, Lu K, Wang C (2015) Mesenchymal stem cells alleviate experimental asthma by inducing polarization of alveolar macrophages. Inflammation 38:485–492. doi:10.1007/s10753-014-9954-6
English K, Barry FP, Mahon BP (2008) Murine mesenchymal stem cells suppress dendritic cell migration, maturation and antigen presentation. Immunol Lett 115:50–58
Chen G, Emens LA (2013) Chemoimmunotherapy: reengineering tumor immunity. Cancer Immunol Immunother 62:203–216. doi:10.1007/s00262-012-1388-0
Yang SH, Park MJ, Yoon IH et al (2009) Soluble mediators from mesenchymal stem cells suppress t cell proliferation by inducing il-10. Exp Mol Med 41:315–324. doi:10.3858/emm.2009.41.5.035
Choi YS, Jeong JA, Lim DS (2012) Mesenchymal stem cell-mediated immature dendritic cells induce regulatory t cell-based immunosuppressive effect. Immunol Invest 41:214–229. doi:10.3109/08820139.2011.619022
Kim J, Hematti P (2009) Mesenchymal stem cell-educated macrophages: a novel type of alternatively activated macrophages. Exp Hematol 37:1445–1453. doi:10.1016/j.exphem.2009.09.004
Maggini J, Mirkin G, Bognanni I et al (2010) Mouse bone marrow-derived mesenchymal stromal cells turn activated macrophages into a regulatory-like profile. PLoS ONE 5:e9252. doi:10.1371/journal.pone.0009252
Nasef A, Zhang YZ, Mazurier C et al (2009) Selected stro-1-enriched bone marrow stromal cells display a major suppressive effect on lymphocyte proliferation. Int J Lab Hematol 31:9–19. doi:10.1111/j.1751-553X.2007.00997.x
Akiyama K, Chen C, Wang D et al (2012) Mesenchymal-stem-cell-induced immunoregulation involves fas-ligand-/fas-mediated t cell apoptosis. Cell Stem Cell 10:544–555. doi:10.1016/j.stem.2012.03.007
Chinnadurai R, Copland IB, Patel SR, Galipeau J (2014) Ido-independent suppression of t cell effector function by ifn-gamma-licensed human mesenchymal stromal cells. J Immunol. 192:1491–1501. doi:10.4049/jimmunol.1301828
Dorronsoro A, Ferrin I, Salcedo JM et al (2014) Human mesenchymal stromal cells modulate t-cell responses through TNF-alpha-mediated activation of NF-kappab. Eur J Immunol 44:480–488. doi:10.1002/eji.201343668
Han Z, Tian Z, Lv G et al (2011) Immunosuppressive effect of bone marrow-derived mesenchymal stem cells in inflammatory microenvironment favours the growth of B16 melanoma cells. J Cell Mol Med 15:2343–2352. doi:10.1111/j.1582-4934.2010.01215.x
Kraman M, Bambrough PJ, Arnold JN, Roberts EW, Magiera L, Jones JO, Gopinathan A, Tuveson DA, Fearon DT (2010) Suppression of antitumor immunity by stromal cells expressing fibroblast activation protein-alpha. Science 330:827–830. doi:10.1126/science.1195300
Ren G, Zhao X, Wang Y et al (2012) Ccr2-dependent recruitment of macrophages by tumor-educated mesenchymal stromal cells promotes tumor development and is mimicked by tnfalpha. Cell Stem Cell 11:812–824. doi:10.1016/j.stem.2012.08.013
Ling W, Zhang J, Yuan Z et al (2014) Mesenchymal stem cells use ido to regulate immunity in tumor microenvironment. Cancer Res 74:1576–1587. doi:10.1158/0008-5472.CAN-13-1656
Scapini P, Cassatella MA (2014) Social networking of human neutrophils within the immune system. Blood 124:710–719. doi:10.1182/blood-2014-03-453217
Joyce JA, Fearon DT (2015) T cell exclusion, immune privilege, and the tumor microenvironment. Science 348:74–80. doi:10.1126/science.aaa6204
Acknowledgments
The authors thank Dr. Aric Frantz, Dr. Daisuke Ito, and Lily Xia, for technical assistance and insightful suggestions. This study was supported by Grant FRD #10.03 from the University of Minnesota Academic Health Center. Histology was carried out at the Comparative Pathology Shared Resource Core of the Masonic Cancer Center and at the BioNet Histology Research Laboratory of the Academic Health Center, University of Minnesota, and was supported in part by Grant P30 CA077598 (Comprehensive Cancer Center Support Grant) from the National Institutes of Health. Edward Zamora was supported by Grant 1T32 CA009138-31s, Cancer Biology Training Grant Minority Supplement. Jaime Modiano is supported by the Alvin and June Perlman Chair in Animal Oncology. Jakub Tolar is supported by the Edmund Wallace and Anna Marie Tulloch Chair in Stem Cell Biology, Genetics, and Genomics.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have conflict of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Modiano, J.F., Lindborg, B.A., McElmurry, R.T. et al. Mesenchymal stromal cells inhibit murine syngeneic anti-tumor immune responses by attenuating inflammation and reorganizing the tumor microenvironment. Cancer Immunol Immunother 64, 1449–1460 (2015). https://doi.org/10.1007/s00262-015-1749-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00262-015-1749-6