Abstract
Purpose
To evaluate safety and diagnostic yield of percutaneous CT-guided biopsy of extrarenal upper urinary tract lesions.
Materials and methods
Retrospective review of our institutional database of image-guided biopsies yielded 44 CT-guided percutaneous biopsies in 44 unique patients that targeted ureteral (30, 68%) or other non-renal upper urinary tract lesions (14, 32%) between January 1, 2000 and May 1, 2017. Indications, pre-biopsy imaging, biopsy technique, peri-procedural antithrombotic use, complications including bleeding defined by Society of Interventional Radiology criteria, pathology results, and subsequent imaging were reviewed up to 3 months after the procedure to evaluate safety and diagnostic yield.
Results
Mean patient age was 66 (range 27–88) and 23/44 patients were male. The majority (34/44) of lesions were sampled with an 18-gauge biopsy device via a 17-gauge introducer needle, and the remaining 10/44 lesions were sampled with a 19/20 gauge system. The mean number of core samples obtained was 4 (range 2–10). No major complications occurred. Specifically, no patient developed a urine leak or urinary obstruction. Minor complications occurred in 3/44 (7%) biopsies, all retroperitoneal hemorrhages that did not require transfusion or other intervention. Biopsy was adequate for pathologic examination in 41 of 44 (93%) cases. Among patients undergoing surgical resection, biopsy diagnosis was concordant with surgical pathology in 9/10 (90%) cases and discordant in 1/10 (10%).
Conclusion
CT-guided percutaneous biopsy of upper urinary tract lesions can be performed safely, with high diagnostic yield, and with a high rate of concordance on subsequent surgical pathology.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Biopsy is an integral component of the evaluation of potentially malignant ureteral and other upper urinary tract masses, and when indicated, is typically performed ureteroscopically. Ureteroscopic biopsy is invasive requiring general anesthesia and ureteral stent placement, and thus may not be feasible in those patients with high-risk comorbidities. While diagnostic ureteroscopy remains the gold standard, it can be technically challenging and is associated with significant false-negative rates depending on morphological characteristics of the lesion [1]. Percutaneous biopsy may be attempted in cases where the targeted segment of ureter or renal pelvis is inaccessible via ureteroscopy, is primarily exophytic rather than endoluminal, or has been sampled with inconclusive results. With the aim of describing risk and efficacy, we retrospectively reviewed our experience of non-renal upper urinary tract biopsies over the last 16 years.
Materials and methods
This retrospective study was approved by the institutional review board, and the requirement for informed consent was waived. Research was performed in accordance with the Health Insurance Portability and Accountability Act.
Patients and data
A retrospective search of a prospectively maintained institutional database yielded 44 biopsies in 44 patients that targeted ureteral (30/44, 68%) or renal pelvis lesions (14/44, 32%) between January 1, 2000 and May 1, 2017. Twenty-three patients (52%) were male. Average patient age was 66 (range 27–88). Twelve patients (27%) continued to take 81 mg aspirin daily through the day of biopsy. Otherwise, no patient had received anti-platelet therapy within 5 days of biopsy. Four patients on warfarin or other anticoagulation medications were bridged with heparin or unfractionated enoxaparin, which were discontinued 4 or 24 h prior to the procedure, respectively. 38 of 44 of the percutaneous ureteral or renal collecting system biopsy referrals were initiated by a urologist. See Table 1 for percutaneous biopsy indications.
Biopsy technique and follow-up
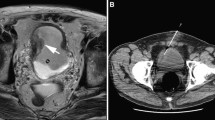
The diagnostic CT or MRI images were reviewed prior to biopsy in all patients. All biopsies were performed with a spring-loaded core sampling device (Bard Medical, Covington, GA) after patient informed consent. The medical records, including available cross-sectional imaging and subsequent surgical procedures, were reviewed up to 3 months after the biopsy to characterize procedural complications and obtain final pathologic results. In addition, patients with benign biopsy results were followed as long as records were available to ensure validity of the biopsy result. Bleeding complications were graded according to Society of Interventional Radiology guidelines. Pathology demonstrating “atypical cells” was considered non-diagnostic. The biopsy results of “atypical cells” and malignancies other than urothelial malignancy were not considered in the calculation of sensitivity and specificity. Only biopsy results of urothelial carcinoma or benign findings were included (Figs. 1, 2).
Results
No major complication occurred in 44 biopsies. Specifically, no major hemorrhage, urinary obstruction, or urine leak occurred. No patients required a new ureteral stent secondary to obstruction, and there was no evidence of ureteral stricture during the follow-up timeframe. Three of 44 (7%) biopsies resulted in minor hemorrhage that did not require treatment (SIR grade A). Two of these bleeding complications were after ureteral biopsies, and a single bleed occurred after a trans-renal collecting system biopsy. None of the patients with hemorrhage were on aspirin or any other anticoagulant.
19 (43%) patients had biopsy performed with a ureteral stent in place. 1 (2%) patient had biopsy performed with both an ipsilateral ureteral stent and nephrostomy tube in place.
Twenty-eight of 44 percutaneous biopsy specimens (64%) were positive for malignancy, including 16 (36%) urothelial carcinoma. Eleven patients (25%) had secondary malignancies involving the urinary tract (lymphoma or other metastatic disease). Of the 4 non-lymphoma metastatic lesions, 2 were prostate and 2 were colon primary adenocarcinomas. Excluding the 3 cases of “atypical cells,” 28 biopsies (64%) yielded results that were considered malignant or suspicious for malignancy. The 16 patients with benign results were followed for a median timeframe of 18 months, range 1–72 months. None of these patients were diagnosed with a malignancy in the available follow-up timeframe. Please see Table 2 for biopsy results.
Thirteen patients had follow-up surgery. Of the 13 lesions that had pathologic results from both percutaneous biopsy and subsequent surgery excluding the three biopsy results of atypical cells, 1/10 (10%) were discordant and 9/10 (90%) were concordant. The discordant case was a benign collecting system biopsy result of papillary proliferation with papillary urothelial malignancy at surgery. The 3 biopsy results of atypical cells were considered non-diagnostic and yielded a single case of inflammation at resection, and the 2 other patients were found to have malignancy at resection, including single cases each of upper tract adenocarcinoma and urothelial carcinoma. The biopsy that demonstrated squamous cell carcinoma was high-grade urothelial carcinoma with squamous features at surgery and considered concordant. All other biopsies with follow-up surgery were concordant. A single case of urothelial carcinoma at biopsy proceeded to surgery and had no malignancy found at surgical resection. This was deemed concordant after discussion with a urology specialist who deemed this to be a true positive with a small volume of cancer not identified at surgical pathology.
Our results, when considering only diagnoses of urothelial carcinoma or benign diagnoses including fibrosis, amyloid, and acute inflammation, demonstrate a sensitivity of 94% and a specificity of 100%. This is as accurate as current diagnostic methods including ureteroscopy and urine cytology. We did not see any cases of tract seeding in our follow-up, although that was not the focus of the study.
Discussion
Percutaneous biopsy of ureteral and collecting system lesions is a helpful alternative to obtain samples of suspicious lesions in difficult clinical situations. Common clinical scenarios appropriate for a percutaneous approach include patients with ileal urinary conduits, difficult anatomy (e.g., exophytic lesion), inability to gain access ureteroscopically, or negative ureteroscopic biopsy results in the setting of high clinical suspicion for malignancy.
No major complication occurred in the current patient cohort. In particular, 27% of patients continued on aspirin therapy at the time of biopsy, but no major bleeding occurred. These results are consistent with a previously published smaller series [2]. In that series, 5 of 26 (19%) patients had a total of 6 minor complications, including 4 patients who developed perinephric hematomas not requiring treatment and one patient with self-limited flank pain and hematuria. These 5 patients all had biopsies involving renal parenchyma or renal pelvis, which likely explains the slightly higher incidence of bleeding. However, this series primarily reported results for fine needle aspiration with a 22 g needle, and only 8 of their cases employed core needle biopsy with a 20-gauge device. All of the samples in the current study were obtained via core needle biopsy, and the majority with an 18-gauge device.
Undersampling of malignant urothelial lesions with either ureteroscopic or percutaneous biopsy is a major concern when targeting lesions involving the extrarenal upper urinary tract. Ureteroscopic biopsy of upper tract urothelial carcinoma has been shown to have a sensitivity of 85.4% and specificity of 100% [1]. Urine cytology and even special testing of urine specimens have only demonstrated sensitivity up to 73% and specificity of 71% [3, 4].
Two separate studies have demonstrated a 15% rate of non-diagnostic biopsies, one study looking at ureteroscopic biopsies and the other percutaneous biopsies [2, 5]. This may have been secondary to technique using fine needle aspiration and smaller biopsy gauge. We did have 3 (7%) biopsies with non-diagnostic results of atypical cells. A study with 26 patients and percutaneous biopsy had no discordant biopsies with follow-up surgical pathology [2]. The biopsy specimens in our current study that had follow-up surgical pathology demonstrated a concordance rate of 90%.
A prior study of percutaneous biopsy found an 11% recurrence rate in the nephrectomy bed, but it was not consistent with tract seeding [2]. We did not see any cases of tract seeding in our follow-up, although that was not the focus of the study.
The current study has several limitations. Many of the patients did not have follow-up surgery secondary to their poor health status so few patients had surgical confirmation of their biopsy results. Other limitations include its retrospective nature and small sample size, although larger than any previous similar study. Some of the patients had biopsies performed with nephrostomy tubes or ureteral stents in place, which may have decreased the risk or detection of urine leak. Also, many of the biopsy results were not graded, making it difficult to ascertain if specimens were upgraded or not. Finally, the patient population was highly selected, including a large number of patients that had either failed or were not amenable to ureteroscopic biopsy. Therefore, these results may not be generalizable to the overall population with suspicious upper urinary tract lesions.
Conclusion
Percutaneous biopsy of the upper urinary tract collecting system appears to be a safe and effective alternative to ureteroscopic biopsy in select patients who have failed or are inappropriate candidates for ureteroscopy.
References
Vashistha V, Shabsigh A, Zynger DL (2013) Utility and diagnostic accuracy of ureteroscopic biopsy in upper tract urothelial carcinoma. Arch Pathol Lab Med 137:400–407. https://doi.org/10.5858/arpa.2012-0136-OA
Huang SY, Ahrar K, Gupta S, et al. (2015) Safety and diagnostic accuracy of percutaneous biopsy in upper tract urothelial carcinoma. BJU Int 115:625–632. https://doi.org/10.1111/bju.12824
Jovanovic M, Soldatovic I, Janjic A, et al. (2011) Diagnostic value of the nuclear matrix protein 22 test and urine cytology in upper tract urothelial tumors. Urol Int 87:134–137. https://doi.org/10.1159/000330246
Messer J, Shariat SF, Brien JC, et al. (2011) Urinary cytology has a poor performance for predicting invasive or high-grade upper-tract urothelial carcinoma. BJU Int 108:701–705. https://doi.org/10.1111/j.1464-410X.2010.09899.x
Wang JK, Tollefson MK, Krambeck AE, Trost LW, Thompson RH (2012) High rate of pathologic upgrading at nephroureterectomy for upper tract urothelial carcinoma. Urology 79:615–619. https://doi.org/10.1016/j.urology.2011.11.049
Acknowledgments
The authors acknowledge the assistance of Sonia Watson, Ph.D., in preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflicts of interest
The authors have no conflicts of interest to declare.
Ethical approval
Institutional Review Board approval was obtained for this retrospective review.
Informed consent
For this type of study formal consent is not required.
Rights and permissions
About this article
Cite this article
Hendrickson, A.C., Schmitz, J.J., Kurup, A.N. et al. Percutaneous ureteral biopsy: safety and diagnostic yield. Abdom Radiol 44, 333–336 (2019). https://doi.org/10.1007/s00261-018-1725-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-018-1725-7