Abstract
Objective
To assess the effects of bevacizumab and everolimus, individually and combined, on CT perfusion (CTp) parameters in liver metastases from neuroendocrine tumors (mNET) and normal liver.
Methods
This retrospective study comprised 27 evaluable patients with mNETs who had participated in a two-arm randomized clinical trial of mono-therapy with bevacizumab (Arm B) or everolimus (Arm E) for 3 weeks, followed by combination of both targeted agents. CTp was undertaken at baseline, 3 and 9 weeks, to evaluate blood flow (BF), blood volume (BV), mean transit time (MTT), permeability surface area product (PS), and hepatic arterial fraction (HAF) of mNET and normal liver, using a dual-input distributed parameter physiological model. Linear mixed models were used to estimate and compare CTp parameter values between time-points.
Results
In tumor, mono-therapy with bevacizumab significantly reduced BV (p = 0.05); everolimus had no effects on CTp parameters. Following dual-therapy, BV and BF were significantly lower than baseline in both arms (p ≤ 0.04), and PS was significantly lower in Arm E (p < 0.0001). In normal liver, mono-therapy with either agent had no significant effects on CTp parameters: dual-therapy significantly reduced BV, MTT, and PS, and increased HAF, relative to baseline in Arm E (p ≤ 0.04); in Arm B, only PS reduced (p = 0.04).
Conclusions
Bevacizumab and everolimus, individually and when combined, have significant and differential effects on CTp parameters in mNETs and normal liver, which is evident soon after starting therapy. CTp may offer an early non-invasive means to investigate the effects of drugs in tumor and normal tissue.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Computed tomography perfusion (CTp) provides a non-invasive means of assessing tissue perfusion [1,2,3]. It has been applied in a variety of clinical settings, including cerebral perfusion and stroke assessment [4]. More limited evaluations have been undertaken in oncologic applications [5].
The CTp technique relies on capturing the time-concentration curve of tissues and vascular inputs simultaneously following the intravenous administration of contrast medium. This data is then applied to physiological perfusion models, in this work the distributed parameter model, which ultimately yield a variety of CTp parameters.
Neuroendocrine tumors and their metastases are generally highly vascular tumors, which are well recognized radiologically by their hypervascular characteristics, most notably on arterial phase imaging [6]. Vascular endothelial growth factor (VEGF) and the mammalian target of rapamycin (mTOR) are implicated in the pathogenesis of this tumor [7,8,9,10,11]. Targeted antivascular therapies which inhibit these pathways are attractive potential therapeutic agents in this tumor. Such agents include bevacizumab, which is a targeted humanized monoclonal antibody to human VEGF, and everolimus, which is a targeted mammalian target of rapamycin (mTOR) inhibitor. Their mechanisms of action have components which affect the angiogenesis pathway (Fig. 1), and the combination of both agents might be expected to have some synergy. Everolimus, which is also used as an immunosuppressive agent, also interrupts signaling pathways of several cytokines and growth factors including interleukin-2 and causes a decrease in protein synthesis and arrest of the cell cycle.
Mechanisms of action of bevacizumab and everolimus. Adapted from http://jkcvhl.com/index.php/jkcvhl/article/view/7/36. Morais [26]
The liver is a particularly common site for metastases from neuroendocrine tumors. CTp provides the opportunity to non-invasively assess the effects of these targeted agents on such tumors. There have been some previous reports of the effects of bevacizumab on liver tumors on CTp parameters [12, 13], and specifically on neuroendocrine liver metastases [14]. A recent article has reported CTp effects of everolimus in liver metastases from pancreatic neuroendocrine tumors [15]. However, to the best of our knowledge, there have been no previous studies investigating the effects on perfusion of either of these agents on normal liver tissue. Furthermore, the dual-vascular input of the liver, which is required to model liver perfusion correctly, has been challenging to incorporate into modeling and has not been utilized in the above studies.
The purpose of our study was to investigate the effects of the above two targeted antivascular agents, bevacizumab and everolimus, individually and in combination, on perfusion in liver metastases from neuroendocrine tumors and normal liver, as assessed by CT perfusion utilizing dual-vascular inputs.
Materials and methods
Patients and therapy
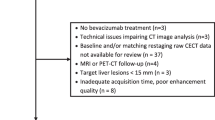
This exploratory analysis was approved by our institutional review board (IRB), with waiver of informed consent and was HIPAA (Health Insurance Portability and Accountability Act) compliant. Novartis and Genentech provided partial funding support for conduct of the study, and everolimus and bevacizumab, respectively. Patients for this analysis were drawn from those who had participated in a randomized two-arm prospective clinical trial employing targeted antivascular therapies for metastatic or recurrent well-differentiated neuroendocrine tumors; patients in that study had provided written informed consent for participation in that trial, including CT perfusion. One arm (Arm B) consisted of mono-therapy with bevacizumab for one cycle (3 weeks), followed by combined (“dual-”) therapy with bevacizumab and everolimus thereafter; the other arm (Arm E) consisted of mono-therapy with everolimus for one cycle, followed by dual-therapy with everolimus and bevacizumab thereafter (Fig. 2).
Bevacizumab was administered intravenously at a dose of 15 mg/kg every 3 weeks, and everolimus was administered orally at a dose of 10 mg daily. Exclusion criteria for the clinical protocol included prior VEGF- or mTOR-inhibitor therapies, although prior antineoplastic therapies were permitted. Other inclusion and exclusion criteria for the clinical study have been presented previously [16]. The current analysis focused solely on the subset of patients who had metastatic disease in the liver (mNET), which comprised 33 patients. In addition, unlike the previous work, the current analysis included dual-input liver CT perfusion modeling, full CT perfusion acquisition durations, image registration, and pixel-level analyses.
CT perfusion
CTp scans were undertaken prior to the initiation of therapy (baseline, T 0), at the end of the first cycle of therapy (3 weeks, T 1), and at the end of the third cycle (9 weeks, T 2) (Fig. 2). Prior to enrollment, previous imaging studies had been reviewed and a single target lesion in the liver identified by a radiologist (C.S.N. with more than 15 years’ experience in interpreting CT studies). The target lesion was required to be a contrast-enhancing solid mass and larger than 2.5 cm in longest diameter.
CT perfusion imaging was obtained with a 64-row multidetector CT scanner (VCT, GE Healthcare, Waukesha, WI) and employed a scanning protocol previously described [17]. In brief, the CTp scans were obtained in two phases: Phase 1, continuous (“cine”, 8 × 0.5-cm slice thickness) acquisition during a 30 s breath-hold; followed by Phase 2, consisting of eight intermittent short breath-hold helical scans through 590 s after commencement of Phase 1. Phase 1 images were reconstructed every half second, and both phases were reconstructed to a thickness of 0.5-cm.
The acquired images of each patient were anatomically registered using a semi-automated rigid registration algorithm, as previously described [18]. The resultant CTp datasets were analyzed using commercially available CT perfusion software on a workstation (CT Perfusion 4 version 4.3.1, Advantage Workstation 4.4; GE Healthcare, Waukesha, WI). The perfusion software utilizes the distributed parameter model. We utilized the Liver Protocol of the vendor software, which incorporates the dual-vascular input of the liver. Regions of interest (ROI) were placed in the abdominal aorta and in the portal vein on the source images to provide these vascular inputs, and perfusion parametric maps were generated of BF, BV, MTT, PS, and HAF, as previously described [17].
For each of the eight axial slice locations of each dataset, a tumor ROI was drawn freehand around the periphery of the target tumor if present on that slice, with reference to the source cine CT images and perfusion maps (C.D., more than 5 years of experience in interpreting CT studies). Visible vessels and artifacts were avoided. Wherever possible, a second tumor ROI was delineated, provided it fulfilled the same criteria as the primary target lesion and was greater than 1.5 cm in diameter.
Parallel analyses were undertaken for background (“normal”) liver parenchyma, in which metastases were not evident, on all available CT slices. Circular or elliptical ROIs were delineated in normal liver regions. These ROIs were as large as possible and placed to avoid vessels and artifacts. We delineated two normal liver ROIs on each of the 8 slices where possible; if possible, separate ROIs were placed in the right and left lobes.
The pixel-level CTp data from tumor and normal liver ROIs were extracted for summary statistics and further analyses.
Statistical methods
Pixel-level data was transformed to the cubic-root scale due to right skewness. All pixel-level data from the same tissue were combined to obtain mean CTp parameters based on the resultant volume of interest (VOI) by patient and time-point. All statistical analyses were carried out on these means on the cubic-root scale. These means were back-transformed to the raw scale for plotting and summary statistics.
Linear mixed models were used to estimate and compare CTp parameters by time, arm, and tissue type. Arm and time were modeled as fixed effect factors and patient as random effect. Since it was expected that changes in CTp parameters over time would be different between arms, an interaction between arm and time was kept for each model. Linear mixed model was also used to compare tumor and normal liver CTp parameters at baseline; arm and tissue type were modeled as fixed effect factors and patient as random effects.
Tukey–Kramer adjustment was used to control overall type I error rate at 5% for comparisons within each model. Estimated means on the cubic-root scale were back-transformed to raw scale, along with 95% confidence intervals for easier interpretation. All tests were two-sided and p values of 0.05 or less were considered statistically significant. Statistical analysis was carried out using SAS version 9 (SAS Institute, Cary, NC).
Results
Patient demographics and clinical features
A total of 39 patients were enrolled in the clinical treatment protocol, of which 33 had a target metastatic lesion in the liver. Patients with non-hepatic metastatic disease were not included in the current work (pancreas (n = 3), abdominal adenopathy (n = 2), and bone (n = 1)). Of the 33 patients with liver metastases, 5 patients were excluded because of inability to satisfactorily delineate a porto-venous vascular input (due to failure to image the portal vein adequately (n = 2) or its cavernous transformation (n = 3)), and one because the target lesion could not be adequately visualized due to streak artifacts. This resulted in a study cohort of 27 patients (median (range) age, 58.3 (21.0–76.9 years); 17 female, 10 male). There were 13 patients in Arm B (median (range) age, 56.0 (21.0–76.9 years); 7 female, 6 male); and 14 patients in Arm E (median (range) age, 56.9 (33.2–76.9 years); 10 female, 4 male). VOI sizes were: for tumor, median 25.0 cm3 (range 1.9–648.1 cm3); and for normal tissue, median 19.4 cm3 (range 1.0–92.3 cm3). Followup CT perfusion scans in 5 patients failed to be obtained: two 9-weeks time-points in each arm, and one 3-week time-point in Arm E.
Tumor vs. normal liver at baseline
CTp parameter values in tumor were significantly different from normal liver at baseline (T 0): tumor BF, BV, and HAF were significantly higher than normal liver (p ≤ 0.02); and MTT and PS were significantly lower (p ≤ 0.01) (Table 1).
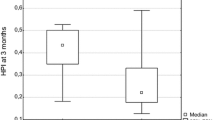
Effects on CTp parameters in tumor
Mono-therapy with bevacizumab for 3 weeks (one cycle) resulted in significant reduction in BV relative to baseline (p = 0.05), and a trend towards reduction in BF (p = 0.09). Following 2 cycles (6 weeks) of combined therapy (i.e. Arm B, with the addition of everolimus), BV and BF were significantly lower than baseline (p = 0.008 and p = 0.01, respectively) (Table 2, Fig. 3A).
In comparison, mono-therapy with everolimus for one cycle did not have significant effects on any of the 5 CTp parameters. Following 2 cycles of combined therapy (i.e. Arm E, following the addition of bevacizumab), BV, BF, and PS were significantly lower than baseline (p = 0.002, p = 0.04 and p < 0.0001, respectively); and BV was significantly lower compared to mono-therapy alone (p = 0.03). An illustrative example is presented in Fig. 4.
No significant effects on tumor MTT or HAF were evident with mono- or subsequent dual-therapy in either arm.
Effects on CTp parameters in normal liver
Mono-therapy, with bevacizumab or everolimus, was not associated with significant changes in any CTp parameters in normal liver.
The addition of everolimus to bevacizumab, in Arm B, was associated with significant reductions in BV, PS, and MTT relative to baseline (p ≤ 0.01) and significant increase in HAF (p = 0.04), with no significant effects on BF; PS and MTT were also significantly lower, and HAF significantly higher, compared to mono-therapy alone (p ≤ 0.03). In comparison, the addition of bevacizumab to everolimus, in Arm E, was associated with a significant reduction in PS relative to baseline (p = 0.04), but no significant effects on other CTp parameters were evident (Table 3, Fig. 3B).
Discussion
Our results show that bevacizumab and everolimus individually have differential effects on perfusion in metastases to the liver from neuroendocrine tumors. Our results also demonstrate that there are different effects on the various perfusion parameters when the two agents are subsequently combined. Furthermore, our results show that normal liver is affected by these agents, and that there are again differential CTp effects according to the temporal sequencing of these agents.
Our study indicates that mono-therapy with bevacizumab was associated with significant reductions in tumor BV, and a trend towards reduction in BF, 3 weeks after initiation of therapy (1 cycle). Early changes in tumor perfusion, as detected by CT perfusion, following the administration of bevacizumab have been observed in other studies and other tumor types. In a study of CTp in hepatocellular carcinoma, BV and BF significantly reduced 2 weeks after the initiation of bevacizumab [12, 13]. In a study of primary rectal cancers, reductions in BV and BF were found 2 weeks after initiation of bevacizumab; interstitial fluid pressure was also found to decrease [19]. In a previous study of mNETs, significant reductions in BV and BF were observed in as little as 2 days after the initiation of bevacizumab, and were sustained at 18 weeks [14]. Antiangiogenic agents, such as bevacizumab, inhibit the proliferation of tumor vessels and are thought to “normalize” and “prune” the tumor vasculature [20], thereby reducing tissue perfusion and the leakiness of the chaotic tumor vessels [20].
In comparison to mono-therapy with bevacizumab, our results suggest that everolimus alone did not have any significant effects on tumor perfusion after one cycle to therapy. It is not possible from our study to determine if this is related to the sample size, dose level, duration of drug exposure and/or the agent itself.
Regarding the effects of dual-therapy, tumor BF decreased significantly relative to baseline in both arms. As regards tumor BV, when bevacizumab was added to everolimus (i.e. Arm E), there was a significant reduction in tumor BV relative to mono-therapy with everolimus alone. In comparison, in Arm B, when everolimus was added to bevacizumab, BV did not significantly change relative to bevacizumab alone. Of note, the individual agents had differing effects on tumor BV. Nevertheless, the net effect was that tumor BV significantly decreased following combined therapy relative to baseline, in both arms. The observations might hint at a more potent effect on BV and BF of bevacizumab compared to everolimus.
Although the combination of both agents in both arms ultimately reduced tumor BV and BF relative to baseline, a differential response was observed with tumor PS. In Arm E, the addition of bevacizumab to everolimus significantly reduced tumor PS relative to baseline; while in Arm B, no significant changes in tumor PS were evident. Thus unlike with BV and BF above, the ultimate effects on PS appear to be affected by temporal sequencing of the agents, which may reflect complex underlying mechanisms and drug interactions. However, it is difficult to determine if this effect might simply be related to the differences of duration of exposure to one of the agents.
A consideration in assessing the efficacy of therapeutic agents in general is their side-effect and toxicity profile; it would be advantageous to have minimal, or preferably no, effects on normal organs. Our study reveals that bevacizumab and everolimus have some effects on perfusion in normal liver: the agents have different effects compared to tumor and also relative to each other. Mono-therapy with bevacizumab or everolimus did not have significant effects on any CTp parameters in normal liver, at least after one cycle of therapy and at the dose levels used in the study. Regarding the effects following dual-therapy, following the addition of everolimus to bevacizumab (Arm B) normal liver PS, MTT, and BV significantly decreased and HAF significantly increased relative to baseline; PS, MTT, and HAF were also significantly different from mono-therapy alone. In comparison, in Arm E, following the addition of bevacizumab after mono-therapy with everolimus, no significant changes in normal liver CTp parameters were evident except for PS where a significant reduction in normal liver PS was observed relative to baseline. A differential effect on PS between arms was also observed for PS in tumor.
Overall, our results suggest that the two agents had differential effects on CTp parameters in tumors, and also had different effects in tumor as compared to normal liver. Noticeably, the agents in both arms after 3 cycles of exposure resulted in lower tumor BF and BV, which could potentially be useful biomarkers of drug efficacy. In comparison in normal liver, of these two CTp parameters, only BV in Arm B was reduced. The significant BV and BF effects on tumor, but relative lack of effects in normal liver, suggests some degree of selectivity for tumors and supports their utility as therapeutic agents. The reduction in tumor PS (Arm E) may be a reflection of the pruning and normalization of tumor vasculature. However, the agents also appear to mediate significant effects on normal liver PS, the consequences of which would require further investigation.
In the context of drug development and in the assessment of therapeutic efficacy, CT perfusion offers the potential to non-invasively assess the effects of individual and combined therapeutic agents, and perhaps to allow titration of dose levels. More broadly, it may have potential to provide insights into pathophysiology and mechanisms of action in tumor and normal tissue, and to act as a prognostic and/or predictive biomarker [1].
We found that tumor BF, BV, PS, and HAF were significantly higher, and MTT significantly lower, than normal/background liver at baseline. Similar findings have been reported in other studies of liver metastases from neuroendocrine tumors [21, 22], and indeed in other tumors, such as hepatocellular carcinoma [23]. Some caution should be exercised when comparing results across studies. In particular, our study utilized a dual (arterial and portal) vascular input CT perfusion model, which more correctly models hepatic perfusion. Marked differences in absolute CTp parameter values when using single- vs. dual-vascular inputs have been demonstrated previously [24]. Also, unlike some other studies, the acquisition duration utilized in our study provided a robust evaluation of CTp parameters, particularly PS [25]. Furthermore, our statistical analyses incorporated consideration of pixel-level distribution of CTp parameter values and the longitudinal nature of the data derived from individual patients.
Comparison with a previous report of the CTp effects of everolimus on liver metastases from pancreatic neuroendocrine tumors in 9 patients is difficult because of differences in perfusion models utilized, study objectives and statistical analyses [15]. Of note, in assessing the potential utility of CTp parameters in differentiating responders from non-responders, the authors undertook a lesion-based (and not patient) analysis, in which they did not appear to acknowledge the non-independent nature of the liver metastases.
We acknowledge limitations in our study. The study was relatively small. The delineation of vascular inputs and tumor ROIs is potentially subject to some observer variability, assessment of which was beyond the scope of this study. As regards delineation of normal liver, we were limited to gross assessments of normality as determined by CT, namely, without pathological confirmation and thus without excluding the possibly of micro-metastases and associated alteration in the microvascular environment. A study which included a longer period of mono-therapy, dose-escalations, and/or more CTp time-points may have provided more insight into the effects of the agents and better temporal delineation of the time course of therapeutic effects; however, this would have increased overall radiation burden, imposed logistics constraints, and possibly compromised patient compliance.
In summary, mono-therapy with bevacizumab and everolimus have different effects on tumor perfusion. The agents have differential effects on CT perfusion in tumor and normal liver parenchyma. Within a tissue type, CTp effects may be influenced by the temporal sequencing of the agents. CT perfusion provides a potential non-invasive means of assessing the early effects of therapies on perfusion in tumors and normal tissues.
References
Dixon AK, Gilbert FJ (2012) Standardising measurement of tumour vascularity by imaging: recommendations for ultrasound, computed tomography, magnetic resonance imaging and positron emission tomography. Eur Radiol 22(7):1427–1429
Miles KA, Charnsangavej C, Lee FT, et al. (2000) Application of CT in the investigation of angiogenesis in oncology. Acad Radiol 7(10):840–850
Miles KA, Griffiths MR (2003) Perfusion CT: a worthwhile enhancement? Br J Radiol 76(904):220–231
Kambadakone AR, Sahani DV (2009) Body perfusion CT: technique, clinical applications, and advances. Radiol Clin North Am 47(1):161–178
Garcia-Figueiras R, Goh VJ, Padhani AR, et al. (2013) CT perfusion in oncologic imaging: a useful tool? Am J Roentgenol 200(1):8–19
Tamm EP, Kim EE, Ng CS (2007) Imaging of neuroendocrine tumors. Hematol Oncol Clin North Am 21(3):409–432
Cen P, Amato RJ (2012) Treatment of advanced pancreatic neuroendocrine tumors: potential role of everolimus. Onco Targets Ther 5:217–224
Hicklin DJ, Ellis LM (2005) Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol 23(5):1011–1027
Konno H, Arai T, Tanaka T, et al. (1998) Antitumor effect of a neutralizing antibody to vascular endothelial growth factor on liver metastasis of endocrine neoplasm. Jpn J Cancer Res 89(9):933–939
Terris B, Scoazec JY, Rubbia L, et al. (1998) Expression of vascular endothelial growth factor in digestive neuroendocrine tumours. Histopathology 32(2):133–138
Zhang J, Jia Z, Li Q, et al. (2007) Elevated expression of vascular endothelial growth factor correlates with increased angiogenesis and decreased progression-free survival among patients with low-grade neuroendocrine tumors. Cancer 109(8):1478–1486
Jiang T, Kambadakone A, Kulkarni NM, Zhu AX, Sahani DV (2012) Monitoring response to antiangiogenic treatment and predicting outcomes in advanced hepatocellular carcinoma using image biomarkers, CT perfusion, tumor density, and tumor size (RECIST). Invest Radiol 47(1):11–17
Zhu AX, Holalkere NS, Muzikansky A, Horgan K, Sahani DV (2008) Early antiangiogenic activity of bevacizumab evaluated by computed tomography perfusion scan in patients with advanced hepatocellular carcinoma. Oncologist 13(2):120–125
Ng CS, Charnsangavej C, Wei W, Yao JC (2011) Perfusion CT findings in patients with metastatic carcinoid tumors undergoing bevacizumab and interferon therapy. Am J Roentgenol 196(3):569–576
D’Onofrio M, Cingarlini S, Ortolani S, et al. (2017) Perfusion CT changes in liver metastases from pancreatic neuroendocrine tumors during everolimus treatment. Anticancer Res 37(3):1305–1311
Yao JC, Phan AT, Hess K, et al. (2015) Perfusion computed tomography as functional biomarker in randomized run-in study of bevacizumab and everolimus in well-differentiated neuroendocrine tumors. Pancreas 44(2):190–197
Ng CS, Hobbs BP, Chandler AG, et al. (2013) Metastases to the liver from neuroendocrine tumors: effect of duration of scan acquisition on CT perfusion values. Radiology 269(3):758–767
Chandler A, Wei W, Anderson EF, et al. (1016) Validation of motion correction techniques for liver CT perfusion studies. Br J Radiol 2012(85):e514–e522
Willett CG, Boucher Y, di Tomaso E, et al. (2004) Direct evidence that the VEGF-specific antibody bevacizumab has antivascular effects in human rectal cancer. Nat Med 10(2):145–147
Jain RK (2001) Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat Med 7(9):987–989
Guyennon A, Mihaila M, Palma J, et al. (2010) Perfusion characterization of liver metastases from endocrine tumors: computed tomography perfusion. World J Radiol 2(11):449–454
Lefort T, Pilleul F, Mule S, et al. (2012) Correlation and agreement between contrast-enhanced ultrasonography and perfusion computed tomography for assessment of liver metastases from endocrine tumors: normalization enhances correlation. Ultrasound Med Biol 38(6):953–961
Catalano OA, Choy G, Zhu A, Hahn PF, Sahani DV (2010) Differentiation of malignant thrombus from bland thrombus of the portal vein in patients with hepatocellular carcinoma: application of diffusion-weighted MR imaging. Radiology 254(1):154–162
Ng CS, Chandler AG, Wei W, et al. (2012) Effect of dual vascular input functions on CT perfusion parameter values and reproducibility in liver tumors and normal liver. J Comput Assist Tomogr 36(4):388–393
Ng CS, Chandler AG, Wei W, et al. (2013) Effect of duration of scan acquisition on CT perfusion parameter values in primary and metastatic tumors in the lung. Eur J Radiol 82(10):1811–1818
Morais C (2014) Sunitinib resistance in renal cell carcinoma. J Kidney Cancer VHL 1(1):1–11
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
NIH CCSG Grant (P30 CA016672), Novartis, Genentech and the John S. Dunn, Sr. Distinguished Chair in Diagnostic Imaging provided partial funding support for conduct of the study.
Conflicts of interest
Chaan S. Ng has received research funding from and is a Consultant for GE Healthcare. Adam G. Chandler is employed by GE Healthcare. The other authors (Wei Wei, Cihan Duran, Payel Ghosh, Ella F. Anderson, and James C. Yao) declare that they have no conflicts of interest.
Ethical approval
This retrospective analysis was approved by our institutional review board (IRB), with waiver of informed consent. Patients for this analysis were drawn from an earlier prospective clinical trial which was undertaken in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration. Informed consent was obtained from all individual participants included in the prospective study.
Rights and permissions
About this article
Cite this article
Ng, C.S., Wei, W., Duran, C. et al. CT perfusion in normal liver and liver metastases from neuroendocrine tumors treated with targeted antivascular agents. Abdom Radiol 43, 1661–1669 (2018). https://doi.org/10.1007/s00261-017-1367-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-017-1367-1