Abstract
Purpose
To assess the performance of CT-Enteroclysis (CTE) in the preoperative evaluation of the small bowel (SB) involvement in patients with peritoneal carcinomatosis (PC), candidates for cytoreductive surgery (CRS) and hyperthermic intraperitoneal chemotherapy (HIPEC).
Material and methods
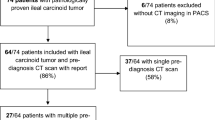
In this prospective study, 48 consecutive patients (37 women, 11 men, mean age: 57.02 years) with PC of different primaries, eligible for cytoreductive surgery and HIPEC underwent CTE before surgery. Lesions were gathered according to their location (SB wall or mesentery), distribution (jejunum/ileum, proximal/distal) and lesion size (LS, where LS0 is the absence of disease, LS1 < 1 cm, LS < 1–5 cm, and LS3 > 5 cm in maximal diameter). The preoperative CTE classification was correlated with surgical scoring of PC in the SB.
Results
CTE was found to have sensitivity 92%, specificity 96%, PPV 97%, NPV 91%, in assessing PC in the SB/mesentery. CTE exhibited “excellent” agreement with surgical classification of disease extent (overall kappa-weighted coefficient of agreement (κ w) was 0.962). Patients (n = 6) found inoperable at surgery manifested extensive plaque-like cover of the SB wall/mesentery on CTE.
Conclusions
CTE may be considered a reliable imaging technique for the preoperative evaluation of the extent and distribution of PC in the SB/mesentery in order to assist surgical planning or to prevent unnecessary surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
The peritoneal carcinomatosis (PC) is a clinical entity considered as the terminal evolution of neoplastic diseases from different primaries in the abdomen and pelvis [1–3]. Before the 1980s, PC was regarded as a lethal disease with disappointing prognosis; the majority of the patients died within 6 months after diagnosis and only palliative treatment was applied [1–3]. The innovations in peritoneal surface malignancy therapeutics and the application of more aggressive methods, namely cytoreductive surgery (CRS) in combination with hyperthermic intraperitoneal chemotherapy (HIPEC), have significantly improved the long-term survival rate in these patients [2–4]. However, the method carries a significant morbidity and mortality, and it is time- and resource-consuming. CRS combined with HIPEC is efficacious if it is performed in selected patients with peritoneal surface malignancy [5–8]. The extent and the distribution of carcinomatosis are the major criteria for limiting patients’ selection and simultaneously are of the most important prognostic factors [1, 3, 6]. Especially, extended load of the disease in the small bowel (SB) constitutes a sentinel, limiting criterion in the decision making process because enough SB needs to remain in place to allow for an adequate oral nutrition in the future [3, 9]. The presence of many diseased parts of the SB requires many segmented enterectomies which may create “short-bowel” syndrome [4, 5, 8]. Thus, evaluation of SB is a crucial component in the preoperative imaging assessment. The Peritoneal Surface Malignancy Group has accepted computed tomography (CT) as the fundamental imaging modality in the preoperative selection process [9–13]. However, even advanced CT technology usually underestimates actual SB involvement revealed at surgical exploration [9, 14]. In this study, we introduce CT in combination with enteroclysis (CT-Enteroclysis (CTE)) for the preoperative evaluation of tumor burden in the SB and it is mesentery and results were correlated with findings at surgery.
Materials and methods
Study group
This prospective study enrolled forty-eight consecutive patients (37 women and 11 men, (mean age: 57.02 years, range: 28–73)) with primary neoplasms in the abdomen (Table 1) and CT and/or MRI evidence of PC, who referred to our hospital during a 26 months period. The study protocol was approved by the Institutional Review Board of our hospital and informed consent was obtained from each subject prior to the CTE examination. All patients were eligible for CRS according to established criteria [3, 7, 8, 15]; no patient exhibited hematogenous metastasis (liver, lungs, bones, etc.) or tumorous involvement of the ligament of Treitz, or ureteral obstruction, or severe intestinal obstruction on previous CT or MR examinations and their physical condition did not preclude surgery (i.e., severe cardio-pulmonary or renal failure, age, cachexia, etc.). All patients underwent a CTE before surgery; time interval between CTE and operation was 4–7 days.
CTE: patient’s preparation, intubation, and scanning technique
Patients were fasting for 24 h prior to examination. SB distention was achieved by bypassing the stomach-using nasojejunal catheter—with rapid (130 mL/min) enteral administration of 1.8–2 L of enteral contrast medium. The nasojejunal intubation and placement were performed under fluoroscopic guidance. A 12.0 F catheter was employed (length: 135 cm, diameter: 12.0 F, Bilbao–Dotter hypotonic duodenography set, Cook, Limerick, Ireland). Local anesthetic (lidocaine hydrochloride 2%, Astrazeneca, Sweden) was applied to the patient’s nasal mucosa before starting the procedure. Intravenous sedative or analgesics were not used. After nasojejunal catheter placement, the patient was transferred to CT-Unit. An initial CT-scan of the abdomen without enteral neither i.v. contrast medium was performed. Afterwards, enteral contrast medium was administrated with the patient on the CT table. The recipient with enteral contrast was placed 150 cm in height from patient’s supine level, and thus, the enteral contrast was pushed to the bowel—via the nasojejunal catheter—due to hydrostatic pressure. Polyethylen glycol (Klean Prep, Helsinn-Birex, Ireland) was used as enteral contrast; it is isosmolar and is not absorbed from the intestinal mucosa, it is well tolerated and provides a neutral endoluminal opacification which promotes better delineation of the enhancing intestinal wall. Shortly before data acquisition, 20 mg of an antiperistaltic agent (scopolaminbutylbromid, Buscopan, Boehringer Ingelheim, Basel, Switzerland) was injected intravenously to diminish bowel motion and related artifacts. Consequently, iodinated nonionic contrast medium was injected (volume in milliliters equal to patient’s body weight plus 30 ml) at a rate of 4 ml/sec with an automatic infusion pump. All examinations were performed on a helical CT scanner (Prospeed, GE Healthcare, Milwaukee, USA) with scanning parameters: 140 kV, 200 mA, 5 mm slice thickness, 5 mm table speed, and 3 mm reconstruction intervals. The scanning delay was 60 s, after starting the intravenous administration of contrast medium.
Analysis of CTE imaging findings in the SB and it is mesentery
SB and it is mesentery were divided into four segments: the proximal jejunum (PJ-SB in the left upper quadrant), the distal jejunum (DJ-SB in the left lower quadrant), the proximal ileum (PI-SB in the right upper quadrant) and the distal ileum (DI-SB in the right lower quadrant). These segments corresponded to segments number 9 (PJ), 10 (DJ), 11 (PI), and 12 (DI) of Peritoneal Cancer Index (PCI) which is the classification system widely used by surgeons for disease load in PC and has been introduced by Jacquet and Sugarbaker [17]. Adequate luminal distention was evaluated in each segment; accepted dilatation was considered when jejunal loop diameter exceeded 20 mm or ileal diameter exceeded 15 mm and corresponded to “good” or “optimal” bowel distention on CTE, according to the scale proposed by Boudiaf et al. [18]. The disease burden of each segment was assessed on a four points grading scale according to lesion size (LS) as follows: LS0 is no disease evidence on imaging, LS1 is cancerous implants with maximal diameter less than 1 cm, LS2 is cancerous implants less than 5 cm but larger than 1 cm in maximal diameter, and LS3 is cancerous lesion larger than 5 cm in diameter. LS criteria were adopted from surgical literature on the “simplified” PCI [1, 17]. When multiple implants were recognized, the LS was based on the larger lesion and if multiple implants were coalesced forming an extended carcinomatous layer or plaque on the intestinal wall/mesentery the LS was graded as 3, in agreement with PCI definition [1, 17]. Stenotic SB segments were measured and gathered according to their length (i.e., stenosis in length 1–5 cm was graded as 2, more than 5 cm was graded as 3). The length of mesenteric surface thickening, the diameter of mesenteric nodules or masses and the diameter of mesenteric stranding were also measured and lesions were gathered into groups 1, 2, or 3 according to their maximal diameter. All CTEs were analyzed and graded in consensus by two experienced (with more than 15 years of experience) abdominal radiologists who calculated the preoperative CTE peritoneal carcinomatosis scoring (CTE-PCS); data were stored and saved in a data base (SPSS 17.0 Statistics for Windows).
Calculation of peritoneal carcinomatosis scoring at surgery (PCSS)
All patients were operated by a surgical team under the same senior surgeon. Implants’ distribution and size were recorded during the procedure accordingly to the scale [1, 17]: LS0 is no disease evidence, LS1 is cancerous implants in a maximal diameter less than 1 cm, LS2 is cancerous implants less than 5 cm but larger than 1 cm, LS3 is cancerous lesion larger in maximum diameter than 5 cm. Disease grading for PJ, DJ, PI, and DI were used for statistical analysis.
Statistical analysis
The agreement of the preoperative CTE-PCS with the PCSS at surgery was tested by the overall kappa-weighted coefficient of agreement (κ w) [20]. Sensitivities, specificities, positive predictive values (PPV), and negative predictive values (NPV) were calculated in order to assess the diagnostic performance of CTE for the presence or absence of disease, using PCSS as the “gold standard”. SPSS 17.0 Statistics for Windows was used for calculation of sensitivities, specificities, PPVs, and NPVs.
Results
CTE was well tolerated in 47 patients, while in one patient the examination was not completed due to vomiting. Adequate SB distention was achieved in all but two patients who were excluded from further analysis.
Table 2 summarizes the CTE and surgical findings according to their size and distribution. In PJ and DJ, the majority of cancerous implants were small (LS1). In PI, the number of LS2 lesions was larger in comparison to PJ and DJ. The highest scoring of lesions’ size was observed in the DI. Implants located on the SB wall were manifested as: nodules (Figs. 1, 2) or masses (Fig. 3), wall thickening exhibiting contrast enhancement, non-completely distended and distorted SB segments with wall irregularity (Fig. 4), or intestinal segment stenosis. Implants on SB mesentery were seen as mesenteric nodules or masses, increased attenuation values or stranding of the mesenteric fat, or thickening and distortion of the mesenteric folds.
The sensitivities, specificities, PPVs, and NPVs of CTE for the four SB/mesentery segments are presented in Table 3. The overall sensitivity, specificity, PPV, and NPV were 92%, 96%, 97%, and 91%, respectively. The observed sensitivity, specificity, PPV, and NPV had the highest values in DI among all SB segments.
Six out of 45 patients were considered “inoperable” in the operating theater, due to extensive infiltration of the SB/mesentery. CTE showed extensive “layered-type” SB involvement in four cases (Fig. 5), extensive involvement of the mesentery in one, and combined extensive SB and mesenteric involvement in one patient. The widely involved mesentery was rigid, thick, and shortened (Fig. 6).
A CT-Enteroclysis section at the pelvis in a patient with peritoneal carcinomatosis demonstrates extensive wall thickening of ileal loops. This is more obvious at neighboring loops, due to cancerous covering of each one of them. This type of involvement is described as “layered-type”. B At surgery, the “layered-type” of involvement corresponds to thin cancerous layer which covers almost entirely the intestinal wall, created by numerous coalescent implanted thin plaques. This patient was considered inoperable.
A CT-Enteroclysis section at the mid-abdomen of a patient with peritoneal carcinomatosis shows a shortened and distorted mesentery with mild surface nodular thickening corresponding to numerous cancerous implants. This type of mesentery could be perceived as “frozen” mesentery due lost of elasticity and shortness. Ascites and “omental-cake” are also noticed. B At surgery the SB mesentery of the same patient is rigid, thickened, and shortened (arrows). This case was considered inoperable.
κ w for the entire SB was 0.962 and corresponds to “excellent” agreement [20] between CTE and surgical findings. The highest κ w was observed in the DI and the lowest in PI. The analytical measurements of κ w for each anatomical segment of the SB are presented in Table 4.
Discussion
Extensive SB infiltration by peritoneal cancerous implants precludes effective CRS, while minimal to moderate disease may require excision of intestinal segments [3, 8]. A recent report concludes that prompt preoperative evaluation of the SB, mesentery, and periportal region for resectability may prevent unnecessary surgery [21]. Consequently, SB evaluation before surgery is of clinical relevance and findings in the preoperative imaging examination are important for the appropriate selection of patients that could benefit from CRS-HIPEC and also for the surgical planning in those patients. Although, CT is the modality of choice in the diagnosis of PC with acceptable overall diagnostic accuracy, the CT performance in detecting disease in SB is inadequate [22]. Sensitivity and specificity of CT in revealing the presence of disease is lower at SB/mesentery as compared to other parts of the peritoneum [9, 12, 13]. Even the agreement among radiologists is quite low in detecting and grading the involvement of the SB, and it is mesentery [23]. In conventional CT examinations, cancerous implants attached to a partially distended or collapsed intestinal loops are very difficult to be diagnosed [1, 9]. The adequate SB loop distension is a prerequisite for depiction of implants attached to the intestinal wall, especially for the small lesions [9]. It is worth noting that experienced surgeons dealing with CRS have mentioned that “bowel loops cut in cross section are often indistinguishable from cancer nodules” and they proposed that “only if maximal oral contrast is utilized to prepare the patient for the examination, can the greatest accuracy and the greatest prognostic implications of the examination be realized”[1]. The profound radiological answer is that enteroclysis combined with CT (CTE) can provide adequate SB loops distention [24], and consequently, small separate or coalescence implants on the intestinal wall/mesentery are more probable to be depicted on CTE. CTE has not been previously applied for preoperative SB evaluation in patients with PC, to the best of our knowledge. In this study, the overall sensitivity and specificity for the presence of disease were 92% and 96%, respectively, while PPV and NPV were 97% and 91%, respectively, for CTE, considering surgical findings as the “gold standard”. Previous studies have reported sensitivities from 8% to 87% and specificities from 67% to 100% [12, 13, 25, 26]. It might be assumed that CTE performs better than conventional CT in the disclosure of peritoneal implants located at the SB/mesentery.
Uneven distribution of PC was observed amongst different parts of the SB/mesentery in the present study. The PJ and DJ were the SB segments with lower disease load. The disease load in the distal ileum and especially at the ileocecal area was high, resulting in increased numbers of implants, usually coalescent to irregular masses. This increased burden of disease could be attributed to gravity gradients and peristaltic waves that propagate ascites with cancerous cells to the DI and it is mesentery, promoting their implantation to the distal ileum [12, 27, 28]. In addition, pooling of ascites at distal mesentery and the ileocecal plica, further facilitates implantation of cancerous cells [28]. Consequently, it is not surprising that DI exhibited the more and the larger lesions that graded with the highest score on CTE evaluation.
The PCI is an established and widely used index for assessing tumor burden in patients with PC [1, 17]. PCI and it is modifications have been applied for the selection of candidates for CRS and it is of prognostic significance as well [5, 7, 8, 13, 15]. In this study, we have adopted the concept of the surgeons in assessing the distribution and severity of PC; SB/mesentery were divided in four segments and lesions were graded by size. The preoperative assessment of tumor burden in SB/mesentery exhibited “excellent” agreement with the PCSS in this study. However, CTE-PCS gave some false-negative results in LS1 lesions. Indeed, faint lesions, a few mm in diameter can be missed by CTE as opposed to LS2 or LS3 lesions that are promptly diagnosed and are also of major clinical importance for surgeons. A LS2 or LS3 on the SB wall usually require excision of the involved intestinal segment and entero-enteric anastomosis, while for LS1 a simple removal is sufficient. Implants located on the mesentery—but not in vicinity with the mesenteric border of the SB—can be treated by excision or ablation, without removal of any SB segment. Localization of a lesion—on the SB wall or on the mesentery—is a clinically relevant information that can be provided by CTE.
Extensive infiltration of the SB/mesentery renders effective cytoreduction impossible [3, 5, 7, 15]. All cases considered inoperable by the surgeons in this study manifested as multiple coalescent cancerous implants in the form of thin contiguous plaques covered extensive segments of the SB wall or of the SB mesentery at surgery. This insidious “layered-type” cancerous coat was disclosed on CTE thanks to SB lumen distention. The “layered-type” irregular thickening of SB wall was associated with either decreased ability of the intestinal loop to distend or stenosis, in a number of cases. These findings can be better appreciated after administration of a large volume of enteral contrast. The same pattern of involvement in the SB mesentery could be associated with distortion, thickening, and fixation of mesenteric folds, which might be referred to as “frozen mesentery”. The aforementioned CTE findings, when present, preclude CRS and could be introduced as an additional exclusive criterion in the selection process for CRS-HIPEC.
The study has some limitations. First, we employed a helical CT scanner that could influence our ability for precise measurements of the smaller lesions or even decrease detectability of sub-centimeter lesions. Second, the study group consisted of patients with different primary sites of cancer. Consequently, the disease morphology and distribution within the peritoneal cavity varied. It could be more descriptive if patients with the same primary were included.
CTE seems to be a reliable imaging examination for the preoperative mapping of the extent and distribution of PC in the SB/mesentery, exhibiting excellent correlation with surgical grading. When conventional CT is inconclusive for estimation of the extent of SB/mesentery PC involvement, CTE might be indicated in the selection process of candidates for optimal CRS.
Abbreviations
- CRS:
-
Cytoreductive surgery
- HIPEC:
-
Hyperthermic intraperitoneal chemotherapy
- CTE:
-
CT-Enteroclysis
- CTE-PCS:
-
CT-Enteroclysis peritoneal carcinomatosis scoring
- PCSS:
-
Peritoneal carcinomatosis scoring at surgery
- PCI:
-
Peritoneal carcinomatosis index
- PJ:
-
Proximal jejunum, corresponding to part 9 of PCI
- DJ:
-
Distal jejunum, corresponding to part 10 of PCI
- PI:
-
Proximal ileum, corresponding to part 11 of PCI
- DI:
-
Distal ileum, corresponding to part 12 of PCI
- κw :
-
Overall Kappa-weighted coefficient of agreement
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
- CI:
-
Confidence interval
References
Harmon RL, Sugarbaker PH (2005) Prognostic indicators in peritoneal carcinomatosis from gastrointestinal cancer. Int Semin Surg Oncol 2:3. doi:10.1186/1477-7800-2-3
Sugarbaker PH (2009) From the guest editors: introduction: progress in the management of carcinomatosis. Cancer J 15:182–183
Roviello F, Caruso S, Marrelli D, et al. (2011) Treatment of peritoneal carcinomatosis with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: state of the art and future developments. Surg Oncol. doi:10.1016/j.suronc.2010.09.002
Yang XJ, Huang CQ, Suo T, et al. (2011) Cytoreductive Surgery and hyperthermic intraperitoneal chemotherapy improves survival of patients with peritoneal carcinomatosis from gastric cancer: final results of a phase III randomized clinical trial. Ann Surg Oncol. doi:10.1245/s10434-011-1631-5
Yan TD, Sim J, Morris DL (2007) Selection of patients with colorectal peritoneal carcinomatosis for cytoreductive surgery and perioperative intraperitoneal chemotherapy. Ann Surg Oncol 14:1807–1817
Yonemura Y, Bando E, Kawamura T, et al. (2007) Cytoreduction and intraperitoneal chemotherapy for carcinomatosis from gastric cancer. Cancer Treat Res 134:357–373
Cotte E, Passot G, Gilly FN, Glehen O (2010) Selection of patients and staging of peritoneal surface malignancies. World J Gastrointest Oncol 2:31–35
McKenzie S, Artinyan A, Holt AD, et al. (2011) Selection criteria for complete cytoreduction after cytoreductive surgery for peritoneal surface malignancy: lessons learned from our first series of patients. Am Surg 77:430–437
González-Moreno S, González-Bayón L, Ortega-Pérez G, González-Hernando C (2009) Imaging of peritoneal carcinomatosis. Cancer J 15:184–189
Yan TD, Morris DL, Shigeki K, Dario B, Marcello D (2008) Preoperative investigations in the management of peritoneal surface malignancy with cytoreductive surgery and perioperative intraperitoneal chemotherapy: Expert consensus statement. J Surg Oncol 98:224–227
Dowdy SC, Mullany SA, Brandt KR, Huppert BJ, Cliby WA (2004) The utility of computed tomography scans in predicting suboptimal cytoreductive surgery in women with advanced ovarian carcinoma. Cancer 101:346–352
Koh JL, Yan TD, Glenn D, Morris DL (2009) Evaluation of preoperative computed tomography in estimating peritoneal cancer index in colorectal peritoneal carcinomatosis. Ann Surg Oncol 16:327–333
Esquivel J, Chua TC, Stojadinovic A, et al. (2010) Accuracy and clinical relevance of computed tomography scan interpretation of peritoneal cancer index in colorectal cancer peritoneal carcinomatosis: a multi-institutional study. J Surg Oncol 102:565–570
Marin D, Catalano C, Baski M, et al. (2010) 64-Section multi-detector row CT in the preoperative diagnosis of peritoneal carcinomatosis: correlation with histopathological findings. Abdom Imaging 35:694–700
Piso P, Glockzin G, von Breitenbuch P, et al. (2009) Patient selection for a curative approach to carcinomatosis. Cancer J 15:236–242
Yan TD, Haveric N, Carmignani CP, Chang D, Sugarbaker PH (2005) Abdominal computed tomography scans in the selection of patients with malignant peritoneal mesothelioma for comprehensive treatment with cytoreductive surgery and perioperative intraperitoneal chemotherapy. Cancer 103:839–849
Jacquet P, Sugarbaker PH (1996) Clinical research methodologies in diagnosis and staging of patients with peritoneal carcinomatosis. In: Sugarbaker PH (ed) Peritoneal carcinomatosis: principles of management. Boston: Kluwer Academic Publishers, pp 359–374
Boudiaf M, Jaff A, Soyer P, et al. (2004) Small-bowel diseases: prospective evaluation of multi-detector row helical CT enteroclysis in 107 consecutive patients. Radiology 233:338–344
Esquivel J, Chua TC (2009) CT versus intraoperative peritoneal cancer index in colorectal cancer peritoneal carcinomatosis: importance of the difference between statistical significance and clinical relevance. Ann Surg Oncol 16:2662–2663
Kundel HL, Polansky M (2003) Measurement of observer agreement. Radiology 228:303–308
Kebapci M, Akca AK, Yalcin OT, et al. (2010) Prediction of suboptimal cytoreduction of epithelial ovarian carcinoma by preoperative computed tomography. Eur J Gynaecol Oncol 31:44–49
Ferrandina G, Sallustio G, Fagotti A, et al. (2009) Role of CT scan-based and clinical evaluation in the preoperative prediction of optimal cytoreduction in advanced ovarian cancer: a prospective trial. Br J Cancer 101:1066–1073
de Bree E, Koops W, Kröger R, et al. (2006) Preoperative computed tomography and selection of patients with colorectal peritoneal carcinomatosis for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Eur J Surg Oncol 32:65–71
Maglinte DD, Sandrasegaran K, Lappas JC, Chiorean M (2007) CT Enteroclysis Radiol 245:661–671
Pestieau SR, Jelinek JS, Sugarbaker PH (2002) Abdominal and pelvic CT for detection and volume assessment of peritoneal sarcomatosis. Tumori 88:209–214
Yan TD, Haveric N, Carmignani CP, Bromley CM, Sugarbaker PH (2005) Computed tomographic characterization of malignant peritoneal mesothelioma. Tumori 91:394–400
Schwartz B, Bresalier RS, Kim YS (1992) The role of mucin in colon-cancer metastasis. Int J Cancer 52:60–65
Meyers MA (2000) Intraperitoneal spread of malignancies in Dynamic Radiology of the Abdomen, Chapter 4, 5th Edition, New York: Springer, pp 131–235
Esquivel J, Chua TC (2009) CT versus intraoperative peritoneal cancer index in colorectal cancer peritoneal carcinomatosis: importance of the difference between statistical significance and clinical relevance. Ann Surg Oncol 16:2662–2663
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Courcoutsakis, N., Tentes, A.A., Astrinakis, E. et al. CT-Enteroclysis in the preoperative assessment of the small-bowel involvement in patients with peritoneal carcinomatosis, candidates for cytoreductive surgery and hyperthermic intraperitoneal chemotherapy. Abdom Imaging 38, 56–63 (2013). https://doi.org/10.1007/s00261-012-9869-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-012-9869-3