Abstract
Background:
Successful surgery for perianal fistula is contingent upon accurate pre-operative classification of the primary tract and its extensions. We aimed to find, using “evidence based medicine” (EBM) methods, the optimal technique for fistula classification: MRI, anal endosonography (AES) or clinical examination.
Methods:
A clinical question was derived, “In patients suspected of having perianal fistula, how does MRI compare to AES and clinical assessment for discriminating simple from complex disease”. A search of primary literature and secondary evidence resources was performed and expert opinion sought. Inclusion criteria were blinded prospective studies (level 2b +) of patients undergoing preoperative MRI, clinical examination ± AES using a clinical outcome based reference standard. Retrieved literature was appraised using EBM methods.
Results:
The highest-ranking evidence found was level 1b. MRI is more sensitive 0.97(CI 0.92–1.01) than clinical examination, 0.75(0.65–0.86) but comparable to AES, 0.92(0.85–0.99) for discriminating complex from simple disease. The positive LR for MRI confirming complex disease is 22.7 compared to 2.1 and 6.2 for clinical examination and AES, respectively.
Conclusion:
MRI is the optimal technique for discriminating complex from simple perianal fistula, although AES is superior to clinical examination, and may be used if MRI availability is restricted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Step 1: Ask
-
Successful surgery for perianal fistula is contingent upon accurate pre-operative classification of the primary tract and its’ extensions (into either simple or complex disease) with a tendency for sepsis to recur and anal continence threatened if complex fistula is not recognised. We wondered whether MRI performs better than anal endosonography (AES) or clinical assessment in discriminating between simple and complex disease in patients suspected of having perianal fistula.
-
Before undertaking this review, our opinion, without explicit critical appraisal, was that MRI was the superior test.
-
Question: In patients with suspected perianal fistula, how does MRI compare with AES or clinical assessment in discriminating between simple and complex disease?
Step 2: Search
-
Our search was performed using standard EBP methods [1].
-
A search of secondary evidence resources including The Clinical Evidence Website from the British Medical Journal Publishing Group [2] and the Cochrane Collaboration Website [3], using the keywords “MRI” and “perianal fistula” or “fistula-in-ano”, resulted in no relevant articles. A search of the turning research into practice (TRIP) database website [4] yielded two articles which were posted on the National Guideline Clearinghouse website [5] and warranted further appraisal. They were clinical guidelines published by the American College of Radiologists [6] and the American Gastroenterological Association [7].
-
A PubMed search of the primary literature was constructed using the PICO format [1] (Fig. 1). Only studies comparing preoperative MRI and clinical examination (with or without AES) and using a clinical outcome based reference standard were included. Results were also restricted to articles written in English and published since the year 2000, in order to reflect current practice.
Step 3: Appraise
Secondary evidence
The 2005 guidelines by the American College of Radiologists [6] provide general guidance for radiological investigation of Crohn’s disease by rating different examination techniques according to their appropriateness in differing clinical environments (adult or pediatric population; new diagnosis or follow up). However, a specific rating was not given for the appropriateness of MRI for assessment of fistula-in-ano complicating Crohn’s disease. Instead, the following statement: “Along with endoscopic US, MRI is the preferred tool for evaluating perianal complications of CD”, was included in a section providing guidance on the use of MRI in patients with established Crohn’s disease and suspected complications. This guidance was based on expert consensus as follows [8]; each expert was provided with evidence from a literature search of peer-reviewed medical journals and other major applicable articles, conducted by the topic leader. The total number of source documents identified by the search was not revealed but 80% agreement between experts was considered a consensus. Additional data analysis was not performed but the guidance stated that “data from existing scientific studies was deemed insufficient for meta-analysis”.
Guidelines from the American Gastroenterological Association [7] encompass diagnosis, management and treatment of perianal Crohn’s disease. These recommendations state that “diagnosis of simple fistulas or complex perianal disease by physical examination and rectosigmoid endoscopy may be sufficient for many patients when medical therapy is the initial treatment strategy. However, if there is pain, fluctuation, or stricture on digital rectal examination or surgery is the initial treatment strategy then examination under anesthesia (EUA) and either AES or pelvic MRI is recommended”. These guidelines acknowledge that EUA is “not 100% accurate and up to 10% of patients will be misclassified on EUA alone which may lead to irreversible functional consequences” although the reference supporting this statement was not specified [7]. These guidelines were constructed from review of published literature via “hand search” and unspecified electronic databases [9]. Systematic review of the evidence was undertaken and recommendations were formulated by expert consensus. The methodology for meta-analysis and for achieving consensus, along with the references for five “level1” studies found was not revealed. Furthermore, these guidelines provide no objective data regarding the relative performance of the diagnostic techniques for discriminating simple from complex fistulas. Given the limitations of this secondary evidence to address our clinical question [10], the primary literature was reviewed.
Primary literature
The PICO search (Fig. 1) resulted in 53 English language citations of which nine were reviews. Abstract review highlighted ten relevant articles (studies) which were retrieved. Eight used operative findings or post operative consensus as the reference standard without taking into account clinical outcome. These were excluded resulting in two papers with an independent, outcome-based reference standard [11, 12] which were appraised using published evidence-based practice methods [13]. The assigned level of evidence according to the Oxford Centre for Evidence-based Medicine [14] is 1b for both studies.
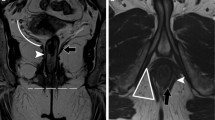
In the study by Chapple [11], 70 consecutive patients were recruited, of which 52 were eligible for analysis. Fistulas were classified using dynamic contrast-enhanced MRI and surgical exploration, into either simple or complex fistulas. These assessments were then correlated with outcome at a minimum of 1 year (satisfactory or unsatisfactory depending on need for further surgery). The results showed MRI was superior to surgical assessment for predicting clinical outcome with a significant association between MRI assessment of complexity and clinical outcome (P < 0.001), whereas there was no such association for surgical assessment and outcome (P > 0.15). While there was no significant difference between the sensitivity or specificity of MRI compared to surgical assessment (likely related to study being underpowered), discordant findings between the two methods were found in 18 of 52 (35%) patients; MRI predicted outcome accurately in 13 (72%) of these.
In the study by Buchanan et al. [12] 104 consecutive patients suspected of having perianal fistula, underwent clinical examination, AES and MRI. An independent, blinded classification of the primary tract, any extensions and site of internal opening was provided by review of each examination. Agreement between the three methods and an outcome derived reference standard [comprising consensus between the three examination methods and prolonged clinical follow up (mean 23 months ± 11)] was analyzed. This study showed significant linear trends favoring the use of MRI over AES and clinical examination, respectively, for correct classification of the primary tract, extensions and site of internal opening; with very good, good and fair agreement (Kappa statistic) between each of the examination methods and reference for MRI, AES and clinical examination, respectively.
Tests of validity of both papers are demonstrated in Table 1 [13]. The strength of the studies are demonstrated by the results described above but also by further analysis of the data (only Buchanan et al [12] contained extractable data) using evidence-based techniques [13]. These data were inputted into a downloadable spreadsheet [15] which analyzed the strength of the data (Table 2). The results indicate that if the MRI is positive, there is a high probability the disease is present, and if negative, the disease is absent.
Step 4: Apply
Best current evidence
Our review has confirmed MRI is superior for discriminating between simple and complex disease compared to clinical assessment and AES. These results are best translated into clinical practice by constructing graphs of conditional probability, based on sensitivity and specificity of each examination method (Figs. 2–4) [13]. These graphs demonstrate the usefulness of each examination method (whether test positive or negative) with differing pre-test probabilities of complex disease; for example, if the pre-test probability of complex fistula is 50%, then the post-test probability following a test-positive assessment is 96, 86 and 68% for MRI, AES and clinical assessment, respectively. While MRI is superior, AES would still be an excellent alternative if MRI availability is restricted.
Graph of conditional probability: diagnostic performance of MRI for complex fistula. (Posttest probability for a positive result is derived by drawing a vertical line up to the solid curved line and then across to the y-axis. Posttest probability for a negative result is derived by drawing a vertical line up to the dotted curved line and then across to the y-axis [13])
Graph of conditional probability: diagnostic performance of AES for complex fistula. (Posttest probability for a positive result is derived by drawing a vertical line up to the solid curved line and then across to the y-axis. Posttest probability for a negative result is derived by drawing a vertical line up to the dotted curved line and then across to the y-axis [13])
Graph of conditional probability: diagnostic performance of clinical assessment for complex fistula. (Posttest probability for a positive result is derived by drawing a vertical line up to the solid curved line and then across to the y-axis. Posttest probability for a negative result is derived by drawing a vertical line up to the dotted curved line and then across to the y-axis [13]
Clinical expertise
In addition to the compelling data extracted above, we sought an expert clinical opinion from Professor Clive Bartram, a highly experienced and widely published gastrointestinal radiologist formerly of St. Mark’s Hospital. His comments are summarized as follows:
-
Clinical assessment starts with a digital examination, continuing during examination under anesthesia with probing of tracts and possibly injection of hydrogen peroxide into an external opening to show the internal opening. Any tract or abscess that is missed will lead to recurrent sepsis, so that surgeons are particularly concerned to know about any extension of sepsis from the primary tract system. A recurrence rate of up to 25% implies that clinical examination and surgery cannot be the gold standard for accuracy. Clinical assessment is also more difficult after surgery as fibrosis makes it harder to feel tracts and collections, so that it is not surprising that MRI has been shown to be of considerable benefit in recurrent fistula. It is also difficult to distinguish active sepsis from fibrosis on endosonography, so MRI has a clear advantage for imaging recurrent disease. Multiplanar imaging is possible with 3D endosonography, but it is still much harder to distinguish a supralevator collection from one in the roof of the ischioanal fossa than on MRI, where the levator muscles are clearly defined in the coronal plane. Image quality is excellent within the sphincter complex on endosonography, but falls-off outside this. Reflections from fascial planes also complicate the image and it is generally much harder to trace sepsis outside the sphincter on endosonography than on MRI. Within the sphincter endosonography has greater resolution than MR unless an endocoil is used, and is helpful to show the extent of internal sphincter division with prior surgery.
-
Anal endosonography within an outpatient setting is very useful as a rapid, simple and cheap imaging method to support clinical examination where there is doubt as to the nature of a fistula, but in any known complex fistula, and this would include all recurrent and Crohn’s fistula, MRI will delineate all the sepsis outside the sphincter and show the relationship to the sphincter and levators, and is therefore the examination of choice.
Step 5: Evaluate
These review data were presented at our hospital’s weekly multi-disciplinary team meeting resulting in unanimous agreement for a unified diagnostic algorithm, with MRI as first line investigation for patients suspected of having perianal fistula.
Our hospital provides both secondary and tertiary referral services for management of perianal fistula and therefore we encounter a higher proportion of complex fistula disease. As a result, our pre-test probability for a patient having complex disease is high compared to secondary referral centers. It is therefore perhaps fortuitous that the study from which we were able to complete a full appraisal originated from our own institution. It is of course possible that these results may not be generalizable across different centers with different patient populations. However, by examining the graphs of conditional probability (Figs. 2–4); an investigator can assess the impact of changing pre-test probability of complex disease on test performance according to the local population. Nevertheless, further research investigating the generalizability of MRI in the diagnostic pathway for perianal fistula in non-specialist centers is warranted, particularly where MRI availability and local expertise for reporting perianal fistula may be restricted. Indeed, in both specialist and non-specialist centers, there may be considerable variability in reader performance between individuals. Therefore in our center, we are planning a prospective audit of radiologist reporting accuracy in routine clinical practice.
A limitation of this review was the small number of studies using a robust (outcome based) reference standard. Most papers used surgery or a consensus of at least two evaluation methods, without clinical follow up to define the reference standard. In addition the lack of extractable data was a major hurdle in the critical appraisal process; for example studies failed to reveal data classifying the primary tract and or the presence of extensions for each patient, according to examination method. Finally, certain studies, even as recently as 2005 [16], used a whole body coil rather than a phased array coil. The phased array coil is the current standard for routine MRI assessment of perianal fistula due to superior spatial resolution over a body coil.
Such limitations might have been largely avoided had studies followed the “STARD initiative” [17], a widely publicized set of “standards for reporting of diagnostic accuracy”. The authors of this review strongly support their use for future diagnostic performance studies.
In summary, this problem based review has supported our initial opinion that MRI is superior to both clinical examination and AES in classifying the complexity of fistula. By undertaking this review, we now have local hospital agreement to offer MRI routinely to all patients suspected of having perianal fistula.
References
Staunton M. Evidence-based radiology: steps 1 and 2––asking answerable questions and searching for evidence. Radiology 2007; 242: 23–31
http://www.clinicalevidence.com/ceweb/index.jsp Accessed 16th April 2007
http://www.cochrane.org Accessed 16th April 2007
http://www.tripdatabase.com Accessed 18th April 2007
http://www.guideline.gov Accessed 18th April 2007
Huprich JE, Bree RL, Foley WD, Gay SB, Glick SN, Heiken JP, Levine MS, Ros PR, Rosen MP, Shuman WP, Greene FL, Rockey DC, Expert panel on gastrointestinal imaging. imaging recommendations for patients with Crohn’s disease. [online publication]. Reston (VA): American College of Radiology (ACR); 2005. p 11 [46 references]
American Gastroenterological Association Clinical Practice Committee 2003 American Gastroenterological Association medical position statement: perianal Crohn’s disease. Gastroenterology 125:1503–1507
http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=8585&string=. Accessed 18th April 2007
http://www.guideline.gov/summary/summary.aspx?ss=15&doc_id=4582&string=. Accessed 18th April 2007
Halligan S, Altman DG. Evidence-based practice in radiology: steps 3 and 4––appraise and apply systematic reviews and meta-analyses. Radiology 2007; 243: 13–27
Chapple KS, Spencer JA, Windsor ACJ, Wilson D, Ward J, Ambrose NS 2000 Prognostic value of magnetic resonance imaging in the management of fistula-in-ano. Dis Colon Rectum; 43:511–516
Buchanan GN, Halligan S, Bartram CI, Williams AB, Tarroni D, Cohen CRG 2004 Clinical examination, endosonography, and mr imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology; 233:674–681
Dodd JJ 2007 Evidence-based practice in radiology: steps 3 and 4––appraise and apply diagnostic radiology literature. Radiology 242: 342–354
http://www.cebm.net/levels_of_evidence.asp. Accessed 18th April 2007
http://www.ebr.ie/spreadsheets/diagnostic.xls. Accessed 18th April 2007
Mahjoubi B, Haizadch Kharazi H, Mirzaei R, Moghimi A, Changizi A 2005 Diagnostic accuracy of body coil MRI in describing the characteristics of perianal fistulas. Colorectal Dis 8:202–207
Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, Lijmer JG, Moher D, Rennie D, de Vet HC 2003 Standards for reporting of diagnostic accuracy. towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Clin Radiol; 58:575–580
Acknowledgments
The authors would like to thank Professor Clive Bartram for his expert opinion and valuable contribution to our review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sahni, V.A., Ahmad, R. & Burling, D. Which method is best for imaging of perianal fistula?. Abdom Imaging 33, 26–30 (2008). https://doi.org/10.1007/s00261-007-9309-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-007-9309-y