Abstract
Purpose
Diagnosis of spinal infection (SI) is challenging and usually requires multiple tests. We aimed to perform a systematic review and a bivariate meta-analysis on the diagnostic role of 18F-FDG PET/CT in patients with SI.
Methods
A comprehensive literature search of studies published through February 2019 in PubMed/MEDLINE and Cochrane library databases was carried out. Studies investigating the diagnostic performance of 18F-FDG PET/CT in patients with SI were eligible for inclusion in the qualitative analysis. For the quantitative analysis, pooled sensitivity, specificity, positive and negative likelihood ratio (LR+ and LR−) and diagnostic odds ratio (DOR) of 18F-FDG PET/CT in patients with suspected SI were calculated on a per examination-based analysis. Pooled data were presented with 95% confidence intervals (95% CI).
Results
Twenty-six articles (833 patients) using 18F-FDG PET/CT were eligible for the qualitative analysis. Twelve studies (396 patients) were selected for the meta-analysis. Overall, 18F-FDG PET/CT demonstrated a very good diagnostic performance in patients with SI and several studies underlined the value of 18F-FDG PET/CT in assessing the response to treatment. The bivariate meta-analysis on 18F-FDG PET/CT in patients with suspected SI provided the following results: sensitivity 94.8% (95% CI 88.9–97.6%) and specificity 91.4% (95% CI 78.2–96.9%). The pooled LR+, LR− and DOR were 4.7 (95% CI 2.9–7.7), 0.11 (95% CI 0.07–0.16) and 63.4 (95% CI 28.9–139), respectively. No significant heterogeneity or publication bias was found.
Conclusion
18F-FDG PET/CT demonstrated a very good diagnostic performance in patients with SI and can be used in patients in which MRI cannot be performed or is non-diagnostic or inconclusive. Several studies underlined the value of 18F-FDG PET/CT in assessing the response to treatment in patients with SI. Overall, larger multicentre and prospective studies and cost-effectiveness analyses are warranted.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Spinal infections (SI) are a heterogeneous group of disorders that can arise from haematogenous seeding of the axial skeleton from remote infected foci (primary SI) or caused by direct inoculation during spinal instrumentation or contiguous spread in patients with pressure sores (secondary SI) [1].
The incidence of SI is on a steady rise and has been reported to reach 6.5/100,000 cases each year [1]. The most frequent SI is spondylodiscitis (intervertebral disc infection with associated vertebral body osteomyelitis), but other types of SI include discitis (isolated intervertebral disc infection), spondylitis (vertebral end-plate infection), septic facet joint infection and epidural abscess. Further spread of infection into adjoining soft tissues accounts for the development of secondary epidural abscesses, paravertebral muscle abscesses and prevertebral collections [1, 2].
Predisposing factors for developing SI include immunodeficiency, drug abuse, widespread use of broad-spectrum antibiotics, corticosteroids, and immunosuppressive drugs, diabetes mellitus and spinal surgery [1,2,3]. SI can be bacterial, fungal, parasitic or viral in origin and every effort should be made to establish a microbiological diagnosis [1,2,3]; in fact, diagnostic cultures are central to directing antimicrobial therapy [2].
Despite the advances in diagnosis and therapy of SI, they remain serious diseases with potentially dangerous complications; therefore, it is relevant to perform an early diagnosis of SI before massive neurologic symptoms occur [1,2,3,4]. Diagnosis of SI is challenging and usually requires multiple tests, including clinical examination, laboratory tests, a combination of imaging techniques and biopsy samples for pathogen detection [1,2,3,4].
Symptoms of SI are often non-specific and this can delay the diagnosis [4]. Constitutional symptoms such as malaise, night sweats, back pain and weight loss are common presenting symptoms; fever is a frequent but inconsistent feature present in about half of the patients with SI [1]. Range of motion of the spine is often limited due to localized spinal pain and muscle spasm [4]. Because of the low specificity of many of these clinical findings and the potential catastrophic outcomes, a high level of suspicion and a thorough diagnostic work-up is required [1, 2].
Inflammatory markers, such as erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), are helpful in screening patients with back pain; unfortunately, they are non-specific since they can also be elevated due to other causes [1, 2].
Plain radiographs are usually normal during the early phases of an SI and become positive only in advanced stages [1, 2]. Contrast-enhanced magnetic resonance imaging (MRI) is the imaging modality of choice for diagnosis of SI if not contraindicated [1, 2, 5, 6] and is useful to evaluate the extent of the infection, providing superior imaging of paraspinal soft tissue and epidural space [2, 5, 6]. The use of gadolinium is essential in differentiating between a phlegmon and an epidural abscess and, if possible, should always be added [1, 5, 6]. However, MRI is sometimes non-specific and cannot always differentiate infections from degenerative end-plate abnormalities or postoperative changes. Moreover, MRI interpretation is hampered by metallic implant-associated artefacts [1, 5, 6].
Nuclear medicine and radiological imaging are complementary techniques in the setting of musculoskeletal infections [7, 8]. In particular, hybrid or multimodality imaging using fluorine-18-fluorodeoxyglucose (18F-FDG) positron emission tomography/computed tomography (PET/CT) could be very useful in patients with suspected SI [6,7,8,9]. 18F-FDG is a glucose analogue that usually shows a high uptake in SI. Several factors may influence 18F-FDG uptake in infection: there are both an increased number and a raised expression of glucose transporters in activated inflammatory cells, as well as an increased affinity of these transporters for glucose [6]. 18F-FDG uptake in SI is usually higher than normal bone marrow; furthermore, degenerative bone changes generally show only faintly 18F-FDG increased uptake, whereas 18F-FDG uptake in traumatized bone usually normalizes within 3–4 months [6]. Compared with CT and MRI, 18F-FDG uptake is minimally hampered by metallic implant-associated artefacts, especially when also looking at the non-attenuated images [6].
Previous published meta-analyses have already evaluated the diagnostic performance of 18F-FDG PET in patients with spondylodiscitis; however, they were based upon mixing data coming from 18F-FDG PET and 18F-FDG PET/CT studies [10,11,12]. This systematic review and meta-analysis examines the diagnostic performance of hybrid 18F-FDG PET/CT in patients with SI, including all types of SI (not only patients with spondylodiscitis) and excluding articles not performing hybrid 18F-FDG PET/CT, in order to provide timely evidence-based data in this setting.
Methods
This systematic review and meta-analysis conforms to the statement on ‘Preferred Reporting Items for Systematic Reviews and Meta-Analyses of Diagnostic Test Accuracy studies’ (PRISMA-DTA), which describes an evidence-based minimum set of items for reporting in systematic reviews and meta-analyses of diagnostic studies [13, 14].
Search strategy
Two authors (GT and MP) performed a comprehensive computer literature search of PubMed/MEDLINE and Cochrane Library databases to find relevant retrospective or prospective published articles on the diagnostic performance of 18F-FDG PET/CT in patients with SI. A search algorithm was constructed using a combination of the following terms: A) ‘PET’ OR ‘positron’ OR ‘FDG’ OR ‘fluorodeoxyglucose’ AND B) ‘spondylodiscitis’ OR ‘spondylodiskitis’ OR ‘discitis’ OR ‘diskitis’ OR ‘spondylitis’ OR ‘vertebral osteomyelitis’ OR ‘spinal osteomyelitis’ OR ‘spinal infection*’ OR ‘spine infection*’ OR ‘vertebral infection*’. The search was carried out from inception to February 28, 2019 without language restriction. To expand the search, references of the retrieved articles were also screened for additional studies.
Study selection
Studies or subsets of studies were only included in the qualitative analysis (systematic review) if investigating the diagnostic performance of 18F-FDG PET/CT in human patients with known or suspected SI. Criteria for excluding studies were as follows: (a) articles not within the field of interest of this review (including those who evaluated 18F-FDG PET only); (b) review articles, editorials or letters, comments and conference proceedings; (c) case reports. Articles with insufficient data to reassess the diagnostic performance or with possible patient overlap were also excluded from the quantitative analysis (meta-analysis). In case of possible patient overlap, the most complete article was selected. Two researchers (GT and MP) independently reviewed titles and abstracts of the retrieved articles, applying the inclusion and exclusion criteria mentioned above. Articles were rejected if they were clearly ineligible. Then, the same two researchers individually examined the full text of the remaining potentially eligible articles to assess their eligibility for inclusion. Disagreements were resolved in a consensus meeting.
Data extraction
For each included study, information was collected concerning basic study data (authors, year of publication, country of origin, study design), patient characteristics (type and number of patients undergoing PET/CT, mean or median age, sex ratio), indication of 18F-FDG PET/CT (diagnosis or assessment of treatment response), technical aspects (hybrid imaging modality, mean injected activity, time interval between radiotracer injection and image acquisition, image analysis and other imaging modalities used for comparison) and diagnostic performance data on 18F-FDG PET/CT.
Quality assessment
Critical appraisal of the overall quality of the studies included in the systematic review was based on the revised ‘Quality Assessment of Diagnostic Accuracy Studies’ tool (QUADAS-2) [15]. This tool evaluates four domains—patient selection, index test, reference standard and flow and timing—in terms of risk of bias. The first three domains are also assessed in terms of concerns regarding applicability [15].
Statistical analysis
Extraction of data regarding sensitivity and specificity, positive and negative likelihood ratio (LR+ and LR−) and diagnostic odds ratio (DOR) of 18F-FDG PET/CT in patients with suspected SI was carried out from individual studies on a per examination-based analysis. A bivariate random effects statistical model was used to calculate pooled data, which were presented with 95% confidence intervals (95% CI). Furthermore, a summary receiver operating characteristic (sROC) curve was constructed. Estimations of heterogeneity and publication bias were determined by using the I-square index (I2) [16] and Egger’s test [17], respectively. Statistical analyses were performed using OpenMetaAnalyst software that is based on R as the underlying statistical engine. OpenMetaAnalyst is funded by the Agency for Healthcare Research and Quality (AHRQ).
Results
Literature search
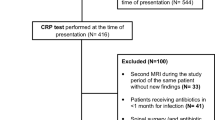
The comprehensive computer literature search from PubMed/MEDLINE and Cochrane Library database yielded a total of 319 articles. After reviewing titles and abstracts, 294 articles were excluded as follows: 209 were not in the field of interest of this review; 43 were reviews, editorials or letters and 42 were case reports. Finally, twenty-five articles were selected and retrieved in full-text version [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42]. One additional study was found screening the references of these articles [43]. Therefore, 26 articles (833 patients) on the diagnostic performance of 18F-FDG PET/CT were identified as eligible for the qualitative analysis [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. Of them, 14 articles were excluded from the quantitative analysis: 12 for insufficient data to reassess the diagnostic performance [21, 26, 30,31,32,33, 35, 38,39,40,41,42] and two for possible patient data overlap [25, 34]. Finally, 12 studies including 396 patients with suspected SI were selected as relevant for the meta-analysis on the diagnostic performance of 18F-FDG PET/CT [18,19,20, 22,23,24, 27,28,29, 36, 37, 43] (Fig. 1).
The characteristics of the studies included in the systematic review are summarized in Tables 1, 2, 3 and 4. Overall quality assessment of the studies is reported in Fig. 2.
Qualitative analysis (systematic review)
Basic study and patient characteristics
Twenty-six full-text articles published between 2007 and 2019 were selected for the systematic review. Several countries from Europe, North America and Asia were represented. About half of the studies were prospective and most of them were single-centre studies.
The patient population included individuals with known or suspected spondylodiscitis or other SI. Mean age and sex ratio were quite heterogeneous amongst the included studies (Table 1). As shown in Table 1, 18F-FDG PET/CT was always performed for diagnostic purpose and in about one-third of the studies was used also for evaluating treatment response.
Technical aspects
Closer inspection of the Table 2 showed heterogeneous technical aspects amongst the included studies. 18F-FDG PET/CT was performed using a low-dose CT acquisition in most cases. The reported mean injected activity of 18F-FDG ranged between 185 and 555 MBq (in absolute values) and between 3 and 5.7 MBq/kg. The time interval between radiotracer injection and image acquisition was highly variable ranging from 30 to 90 min after radiopharmaceutical injection.
The PET image analysis was performed by using qualitative (visual) analysis in all studies: a patient was usually considered positive for SI at 18F-FDG PET/CT when the uptake in the spinal target region was higher than bone marrow uptake in adjacent vertebras and/or the uptake in soft tissue was present. As can be seen from the Table 2, the visual score was used as imaging analysis in all studies, except one not reporting data [31] and was mainly performed considering intensity, site and pattern of radiopharmaceutical uptake. Additional semi-quantitative analysis was carried out in almost all studies and the most frequent semi-quantitative parameter was the maximal standardized uptake value (SUVmax) of the target region [18, 19, 21, 23,24,25,26,27,28,29,30, 32, 33, 35,36,37,38,39,40,41,42]. Moreover, the semi-quantitative evaluation was performed using other parameters (i.e. SUVratio: ratio between 18F-FDG uptake in the target region and uptake in a reference region) in nine studies [18, 23, 26, 27, 36,37,38, 41, 42]. Finally, in almost half of the studies [18, 20,21,22,23,24,25,26,27, 29, 33, 34, 36, 37, 42], the diagnostic performance of 18F-FDG PET/CT was compared also with other imaging tests, mostly MRI.
Main findings
Table 3 presents the diagnostic accuracy data of 18F-FDG PET/CT in patients with known or suspected SI from each study. Overall, 18F-FDG PET/CT demonstrated a good diagnostic accuracy in the diagnosis of SI (from 75 to 100%).
At visual assessment of PET images, inter-observer agreement was good with a kappa coefficient ranging from 0.75 to 0.76 [18, 23].
In patients with spinal hardware infection, 18F-FDG PET/CT showed intense, confluent and increased radiopharmaceutical uptake in the soft tissues and bone immediately adjacent to the spine hardware at multiple contiguous levels, with or without additional increased 18F-FDG uptake at the bone-hardware interface of one or more interpedicular screws [32]. Conversely, PET/CT findings of non-infectious hardware complications as hardware loosening/bone remodelling consisted of focal 18F-FDG uptake adjacent to one or two hooks, screws or anchors usually at the upper or lower portion of the spinal hardware construct [32].
The most common causes of false-positive findings for SI at 18F-FDG PET/CT were inflammatory or degenerative spondyloarthropathy, recent vertebral fractures, postoperative inflammation in previously operated patients or bone tumours. By contrast, false negatives can be due to some cases of infection with low-virulence bacteria, previous antimicrobial therapy, epidural abscesses or extensive instrumented arthrodesis in previously operated patients.
In several articles, multilevel SI and/or additional extra-spinal sources of infection or inflammation were identified by 18F-FDG PET/CT in some patients [19, 20, 22, 27, 30, 32,33,34, 36, 40].
In one article performing dual-time PET/CT acquisition protocols, no statistical difference was found between early and delayed SUVmax results in patients with SI [24].
In most of the articles comparing 18F-FDG PET/CT and MRI, the diagnostic accuracy of 18F-FDG PET/CT in patients with SI was found higher than MRI [18, 22,23,24, 27, 29, 36], whereas only two articles reported a superiority of MRI compared with 18F-FDG PET/CT without a statistically significant difference [20, 37]. Furthermore, 18F-FDG PET/CT showed higher sensitivity in diagnosing paravertebral and psoas abscesses compared with MRI, but the latter was more valuable in detecting epidural and spinal abscesses than 18F-FDG PET/CT [20, 22].
Additionally, a prospective study demonstrated a superior diagnostic accuracy of 18F-FDG PET/CT compared with planar bone scintigraphy plus Gallium-67 single-photon emission computed tomography (67Ga-SPECT)/CT in this setting [34].
Only one study described the clinical impact of 18F-FDG PET/CT in patients with SI showing that this examination provided additional information in 72% of cases and changed the clinical management in 52% of patients with SI [40].
Finally, the role of 18F-FDG PET/CT in evaluating the treatment response in patients with SI was assessed in just over a third of the articles [19, 21, 25, 26, 30, 33, 35, 37, 39, 41] and the main findings are summarized in Table 4. Overall, 18F-FDG PET/CT was useful to detect the early response to therapy in patients with SI. Change of SUVmax provided the highest sensitivity and specificity values for identifying treatment responders [19, 21, 25, 26, 30, 33, 35, 37, 39, 41]. Some prospective studies calculated the diagnostic performance of delta-SUVmax ((SUVmax before treatment—SUVmax after treatment)/SUVmax before treatment) in discriminating patients with SI who responded to the treatment [35, 41]. Nanni et al. showed that a cutoff of delta-SUVmax of 34% demonstrated a sensitivity of 82% and a specificity of 82% in differentiating treatment responders from non-responders [35]. Kim et al. found that using a cutoff of delta-SUVmax of 43% the patient-based sensitivity and specificity was 100% and 76.9%, respectively [41].
Quantitative analysis (meta-analysis)
Twelve studies including 396 patients were selected for the meta-analysis on the diagnostic performance of 18F-FDG PET/CT in patients with suspected SI by using visual analysis [18,19,20, 22,23,24, 27,28,29, 36, 37, 43]. Histological and/or microbiological findings or clinical follow-up were used as reference standard. Results of the meta-analysis are presented in Figs. 3, 4, 5 and 6.
Plots of individual studies and pooled positive likelihood ratios (LR+) of 18F-FDG PET/CT in patients with suspected spinal infection, including 95% confidence intervals (95% CI). The size of the squares is related to the weight of each study. The horizontal lines indicate the 95% CI values for each study, whereas the horizontal diameter of the rhombus indicates the 95% CI value for the pooled LR+
Plots of individual studies and pooled negative likelihood ratios (LR−) of 18F-FDG PET/CT in patients with suspected spinal infection, including 95% confidence intervals (95% CI). The size of the squares is related to the weight of each study. The horizontal lines indicate the 95% CI values for each study, whereas the horizontal diameter of the rhombus indicates the 95% CI value for the pooled LR−
Plots of individual studies and pooled diagnostic odds ratio (DOR) of 18F-FDG PET/CT in patients with suspected spinal infection, including 95% confidence intervals (95% CI). The size of the squares is related to the weight of each study. The horizontal lines indicate the 95% CI values for each study, whereas the horizontal diameter of the rhombus indicates the 95% CI value for the pooled DOR
The sensitivity of 18F-FDG PET/CT in patients with suspected SI ranged from 81.8 to 100%, with a pooled estimate of 94.8% (95% CI 88.9–97.6%). The specificity of 18F-FDG PET/CT in patients with suspected SI varied from 50 to 100%, with a pooled estimate of 91.4% (95% CI 78.2–96.9%). The sROC curve demonstrated a very good diagnostic performance of 18F-FDG PET/CT in detecting SI (Fig. 3). The pooled LR+, LR− and DOR were 4.7 (95% CI 2.9–7.7), 0.11 (95% CI 0.07–0.16) and 63.4 (95% CI 28.9–139), respectively (Figs. 4, 5 and 6).
No statistically significant heterogeneity amongst the studies was found for all the metrics evaluated (I2 < 50%). No significant publication bias was detected by Egger’s test (p = 0.1).
Discussion
Several studies have performed 18F-FDG PET/CT in patients with suspected SI reporting different values of diagnostic performance [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43]. However, most of these studies have limited power, due to the relatively small numbers of patients enrolled. Therefore, we have pooled data reported in the published studies increasing the statistical power to obtain more robust estimates on the diagnostic performance of 18F-FDG PET/CT in this setting [44].
Previous systematic reviews and meta-analyses evaluating the diagnostic performance of 18F-FDG PET and PET/CT in patients with spondylodiscitis [10,11,12] pooled together results from studies performing both 18F-FDG PET alone and PET/CT, which are expected to yield different diagnostic accuracies with higher values for hybrid PET/CT [45, 46]. As hybrid imaging methods are the current state of the art for PET imaging [46], we performed a systematic review and meta-analysis including only articles performing PET/CT and excluding those performing PET alone in order to provide timely evidence-based data. Furthermore, we have broadened the population with respect to the previous meta-analyses, including other patients with SI beyond spondylodiscitis. For all the reasons mentioned above, our results should not be compared with prior published meta-analyses.
The current study found that 18F-FDG PET/CT has a very good diagnostic performance in patients with suspected SI with high values of sensitivity (94.8%) and specificity (91.4%).
One interesting finding is that some key elements may be useful to guide the visual assessment of 18F-FDG PET/CT in cases of suspected SI, including the topography of hypermetabolic areas (pattern analysis) and the intensity of the uptake [18, 19]. Furthermore, the semi-quantitative analysis may support the visual analysis for the diagnosis of SI. Lastly, morphological abnormalities at co-registered CT images may reinforce the PET analysis [18, 19].
A recent diagnostic flowchart on imaging methods in patients with suspected SI have highlighted the predominant role of MRI in patients with suspected SI of haematogenous origin and the predominant role of 18F-FDG PET/CT in patients with post-surgical SI [9]. Based on available literature data, 18F-FDG PET/CT appears to be helpful in particular in those cases in which MRI cannot be performed or is non-diagnostic and as an adjunct in patients in whom the diagnosis is inconclusive [9].
Although 18F-FDG PET/CT has demonstrated an overall higher diagnostic performance compared with MRI for SI detection based on data retrieved by the articles included in our systematic review (Table 3), a possible selection bias cannot be excluded as in some studies only patients with inconclusive MRI underwent 18F-FDG PET/CT (Table 1). 18F-FDG PET/CT showed higher sensitivity in diagnosing paravertebral and psoas abscesses than MRI, whereas the latter was more valuable in detecting epidural and spinal abscesses [20, 22]. Clear advantages of 18F-FDG PET/CT over MRI are the absence of contraindication and severe artefacts in patients with metallic implants as well as the possibility to detect alternative or additional sources of infection or inflammation outside the spine [20, 22].
18F-FDG PET/CT can also contribute to the early assessment of the response to therapy in patients with SI [47], in particular in identifying the responders by change in the SUVmax. Consistent with this finding, some studies demonstrated that 18F-FDG PET/CT is more accurate and specific than MRI in this setting (Table 4), suggesting that 18F-FDG PET/CT should be preferred over MRI for determining when treatment can be safely discontinued, especially in those patients with a non-informative biochemical test for inflammatory markers at diagnosis.
Notably, a recent interdisciplinary and evidence-based consensus document on imaging of SI have highlighted the role of 18F-FDG PET/CT in patients with suspected SI [9]. The most relevant recommendations of this consensus document about 18F-FDG PET/CT in SI are the following: (a) in patients with suspected SI and elevated ESR and/or CRP and doubtful MRI, 18F-FDG PET/CT should be performed (level of evidence: 1); (b) in primary and post-surgical SI, if MRI is contraindicated, 18F-FDG PET/CT is the imaging modality of choice (level of evidence: 2); (c) in post-surgical SI, 18F-FDG PET/CT can detect both bone infection and soft tissue infection (level of evidence: 2); (d) in patients with SI diagnosed by 18F-FDG PET/CT, a second 18F-FDG PET/CT scan can be performed to evaluate the response to antibiotic therapy (level of evidence: 4) [9].
18F-FDG PET/MRI, that is now becoming increasingly available [48], could be another promising diagnostic tool in SI. In contrast to PET/CT, the advantages of PET/MRI are less radiation exposure and higher soft tissue contrast [48]. Unfortunately, only one study assessed the role of 18F-FDG PET/MRI in patients with suspected SI reporting a sensitivity, specificity, PPV and NPV of 100%, 88%, 86% and 100%, respectively; interestingly, the use of 18F-FDG PET/MRI significantly increased the diagnostic accuracy for the detection of SI compared with MRI alone [49]. This finding suggests the potential role of 18F-FDG PET/MRI as ‘one-stop-shop’ hybrid imaging modality in patients with SI, but further investigations should be undertaken on this topic in future research.
Given that 18F-FDG is a not specific tracer for infection, other radiopharmaceuticals have been preliminary used in the work-up of patients with SI. Experimental radiotracers such as radiolabelled antibiotics or vitamins are being developed and tested in preliminary studies with encouraging results but large-scale studies are needed [9]. 68Ga-citrate is another PET radiopharmaceutical that has been investigated in patients with inflammatory or infectious diseases, including SI [50]. In a preliminary study on the use of 68Ga-citrate PET/CT in patients with suspected bone infections, including SI, sensitivity, specificity, PPV, NPV and accuracy of 68Ga-citrate PET/CT were 100%, 76%, 85%, 100% and 90%, respectively [51]. To the best of our knowledge, there are no studies comparing the diagnostic performance of 68Ga-citrate PET/CT and 18F-FDG PET/CT in patients with suspected SI, but this may be a topic for future research.
Some limitations of our systematic review and meta-analysis should be underlined. A major limitation was the lack of laboratory data (histopathological or microbiological) as gold standard in all patients with suspected SI; therefore, some uncertainty remains in the cases with clinical follow-up.
Another potential source of bias in the meta-analyses on the diagnostic performance of 18F-FDG PET/CT in infectious and inflammatory diseases may be the heterogeneity amongst studies [52], which can be explained by baseline differences amongst patients (Table 1), various methodological aspects (Table 2) and different study quality. However, no significant statistical heterogeneity nor a significant publication bias was detected amongst the studies included in our meta-analysis.
Diagnostic performance of a test is not a measure of clinical effectiveness and improved accuracy does not necessarily result in improved patient outcomes. Unfortunately, only one article included in our systematic review assessed the clinical impact of 18F-FDG PET/CT in patients with SI reporting additional information in 72% of cases and change of clinical management in 52% of patients [40].
Overall, our systematic review and meta-analysis demonstrated that 18F-FDG PET/CT is an accurate diagnostic method in patients with suspected SI and could be used for evaluating the early response to treatment. Despite these promising results, larger prospective and multicentre studies, in particular cost-effectiveness analyses are warranted to strengthen the role of this imaging modality in this setting. Therefore, further studies will need to be undertaken, for both diagnosis and assessment of treatment response, to develop a full picture of the role of 18F-FDG PET/CT and 18F-FDG PET/MRI in patients with known or suspected SI.
Conclusions
Based on current available literature data, 18F-FDG PET/CT demonstrated a very good diagnostic performance in patients with suspected SI and can be used in patients in which MRI cannot be performed or is non-diagnostic or inconclusive. Indeed, several studies underlined the value of 18F-FDG PET/CT in evaluating the response to treatment in patients with SI. Larger multicentre and prospective studies and cost-effectiveness analyses in this field would be of great help in strengthening the role of 18F-FDG PET/CT in this setting.
References
Babic M, Simpfendorfer CS. Infections of the Spine. Infect Dis Clin N Am. 2017;31(2):279–97.
Boody BS, Tarazona DA, Vaccaro AR. Evaluation and management of pyogenic and tubercular spine infections. Curr Rev Musculoskelet Med. 2018;11(4):643–52.
Thurnher MM, Olatunji RB. Infections of the spine and spinal cord. Handb Clin Neurol. 2016;136:717–31.
Nagashima H, Tanishima S, Tanida A. Diagnosis and management of spinal infections. J Orthop Sci. 2018;23(1):8–13.
Talbott JF, Shah VN, Uzelac A, Narvid J, Dumont RA, Chin CT, et al. Imaging-based approach to Extradural Infections of the Spine. Semin Ultrasound CT MR. 2018;39(6):570–86.
Raghavan M, Lazzeri E, Palestro CJ. Imaging of Spondylodiscitis. Semin Nucl Med. 2018;48(2):131–47.
Glaudemans AW, Prandini N, DI Girolamo M, Argento G, Lauri C, Lazzeri E, et al. Hybrid imaging of musculoskeletal infections. Q J Nucl Med Mol Imaging. 2018;62(1):3–13.
Treglia G, Focacci C, Caldarella C, Mattoli MV, Salsano M, Taralli S, et al. The role of nuclear medicine in the diagnosis of spondylodiscitis. Eur Rev Med Pharmacol Sci. 2012;16(Suppl 2):20–5.
Lazzeri E, Bozzao A, Cataldo MA, Petrosillo N, Manfrè L, Trampuz A, et al. Joint EANM/ESNR and ESCMID-endorsed consensus document for the diagnosis of spine infection (spondylodiscitis) in adults. Eur J Nucl Med Mol Imaging. 2019. https://doi.org/10.1007/s00259-019-04393-6.
Prodromou ML, Ziakas PD, Poulou LS, Karsaliakos P, Thanos L, Mylonakis E. FDG PET is a robust tool for the diagnosis of spondylodiscitis: a meta-analysis of diagnostic data. Clin Nucl Med. 2014;39(4):330–5.
Yin Y, Liu X, Yang X, Guo J, Wang Q, Chen L. Diagnostic value of FDG-PET versus magnetic resonance imaging for detecting spondylitis: a systematic review and meta-analysis. Spine J. 2018;18(12):2323–32.
Kim SJ, Pak K, Kim K, Lee JS. Comparing the diagnostic accuracies of F-18 fluorodeoxyglucose positron emission tomography and magnetic resonance imaging for the detection of spondylodiscitis: a meta-analysis. Spine (Phila Pa 1976). 2019;44(7):E414–22.
McInnes MDF, Moher D, Thombs BD, McGrath TA, Bossuyt PM, the PRISMA-DTA Group, et al. Preferred reporting items for a systematic review and meta-analysis of diagnostic test accuracy studies: the PRISMA-DTA statement. JAMA. 2018;319(4):388–96.
Sadeghi R, Treglia G. Systematic reviews and meta-analyses of diagnostic studies: a practical guideline. Clin Transl Imaging. 2017;5:83–7.
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, et al. Bossuyt PM; QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Harbord RM, Egger M, Sterne JA. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25:3443–57.
Follenfant E, Balamoutoff N, Lawson-Ayayi S, Dutronc H, Dupon M, Vital JM, et al. Added value of [(18)F]fluorodeoxyglucose positron emission tomography/computed tomography for the diagnosis of post-operative instrumented spine infection. Joint Bone Spine. 2019;86(4):503–8.
Yu GJ, Koslowsky IL, Riccio SA, Chu AKM, Rabin HR, Kloiber R. Diagnostic challenges in pyogenic spinal infection: an expanded role for FDG-PET/CT. Eur J Clin Microbiol Infect Dis. 2018;37(3):501–9.
Kouijzer IJE, Scheper H, de Rooy JWJ, Bloem JL, Janssen MJR, van den Hoven L, et al. The diagnostic value of (18)F-FDG-PET/CT and MRI in suspected vertebral osteomyelitis—a prospective study. Eur J Nucl Med Mol Imaging. 2018;45(5):798–805.
Bassetti M, Merelli M, Di Gregorio F, Della Siega P, Screm M, Scarparo C, et al. Higher fluorine-18 fluorodeoxyglucose positron emission tomography (FDG-PET) uptake in tuberculous compared to bacterial spondylodiscitis. Skelet Radiol. 2017;46(6):777–83.
Smids C, Kouijzer IJ, Vos FJ, Sprong T, Hosman AJ, de Rooy JW, et al. A comparison of the diagnostic value of MRI and (18)F-FDG-PET/CT in suspected spondylodiscitis. Infection. 2017;45(1):41–9.
Dauchy FA, Dutertre A, Lawson-Ayayi S, de Clermont-Gallerande H, Fournier C, Zanotti-Fregonara P, et al. Interest of [(18)F]fluorodeoxyglucose positron emission tomography/computed tomography for the diagnosis of relapse in patients with spinal infection: a prospective study. Clin Microbiol Infect. 2016;22(5):438–43.
Gunes BY, Onsel C, Sonmezoglu K, Ozaras R, Halac M, Tabak F, et al. Diagnostic value of F-18 FDG PET/CT in patients with spondylodiscitis: is dual time point imaging time worthy? Diagn Microbiol Infect Dis. 2016;85(3):381–5.
Riccio SA, Chu AK, Rabin HR, Kloiber R. Fluorodeoxyglucose positron emission tomography/computed tomography interpretation criteria for assessment of antibiotic treatment response in pyogenic spine infection. Can Assoc Radiol J. 2015;66(2):145–52.
Niccoli Asabella A, Iuele F, Simone F, Fanelli M, Lavelli V, Ferrari C, et al. Role of (18)F-FDG PET/CT in the evaluation of response to antibiotic therapy in patients affected by infectious spondylodiscitis. Hell J Nucl Med. 2015;18(Suppl 1):17–22.
Fuster D, Tomás X, Mayoral M, Soriano A, Manchón F, Cardenal C, et al. Prospective comparison of whole-body (18)F-FDG PET/CT and MRI of the spine in the diagnosis of haematogenous spondylodiscitis. Eur J Nucl Med Mol Imaging. 2015;42(2):264–71.
Inanami H, Oshima Y, Iwahori T, Takano Y, Koga H, Iwai H. Role of 18F-fluoro-D-deoxyglucose PET/CT in diagnosing surgical site infection after spine surgery with instrumentation. Spine (Phila Pa 1976). 2015;40(2):109–13.
Nakahara M, Ito M, Hattori N, Magota K, Takahata M, Nagahama K, et al. 18F-FDG-PET/CT better localizes active spinal infection than MRI for successful minimally invasive surgery. Acta Radiol. 2015;56(7):829–36.
Dureja S, Sen IB, Acharya S. Potential role of F18 FDG PET-CT as an imaging biomarker for the noninvasive evaluation in uncomplicated skeletal tuberculosis: a prospective clinical observational study. Eur Spine J. 2014;23(11):2449–54.
Fransen BL, de Visser E, Lenting A, Rodenburg G, van Zwet AA, Gisolf EH. Recommendations for diagnosis and treatment of spondylodiscitis. Neth J Med. 2014;72(3):135–8.
Bagrosky BM, Hayes KL, Koo PJ, Fenton LZ. 18F-FDG PET/CT evaluation of children and young adults with suspected spinal fusion hardware infection. Pediatr Radiol. 2013;43(8):991–1000.
Ioannou S, Chatziioannou S, Pneumaticos SG, Zormpala A, Sipsas NV. Fluorine-18 fluoro-2-deoxy-D-glucose positron emission tomography/computed tomography scan contributes to the diagnosis and management of brucellar spondylodiskitis. BMC Infect Dis. 2013;13:73.
Fuster D, Solà O, Soriano A, Monegal A, Setoain X, Tomás X, et al. A prospective study comparing whole-body FDG PET/CT to combined planar bone scan with 67Ga SPECT/CT in the Diagnosis of Spondylodiskitis. Clin Nucl Med. 2012;37(9):827–32.
Nanni C, Boriani L, Salvadori C, Zamparini E, Rorato G, Ambrosini V, et al. FDG PET/CT is useful for the interim evaluation of response to therapy in patients affected by haematogenous spondylodiscitis. Eur J Nucl Med Mol Imaging. 2012;39(10):1538–44.
Seifen T, Rettenbacher L, Thaler C, Holzmannhofer J, Mc Coy M, Pirich C. Prolonged back pain attributed to suspected spondylodiscitis. The value of 18F-FDG PET/CT imaging in the diagnostic work-up of patients. Nuklearmedizin. 2012;51(5):194–200.
Skanjeti A, Penna D, Douroukas A, Cistaro A, Arena V, Leo G, et al. PET in the clinical work-up of patients with spondylodiscitis: a new tool for the clinician? Q J Nucl Med Mol Imaging. 2012;56(6):569–76.
Kim K, Kim SJ, Kim IJ, Kim BS, Pak K, Kim H. Diffuse increased splenic F-18 fluorodeoxyglucose uptake may be an indirect sign of acute pyogenic cause rather than tuberculous in patients with infectious spondylitis. Nucl Med Commun. 2011;32(12):1155–61.
Gasbarrini A, Boriani L, Nanni C, Zamparini E, Rorato G, Ghermandi R, et al. Spinal infection multidisciplinary management project (SIMP): from diagnosis to treatment guideline. Int J Immunopathol Pharmacol. 2011;24(1 Suppl 2):95–100.
Ito K, Kubota K, Morooka M, Hasuo K, Kuroki H, Mimori A. Clinical impact of (18)F-FDG PET/CT on the management and diagnosis of infectious spondylitis. Nucl Med Commun. 2010;31(8):691–8.
Kim SJ, Kim IJ, Suh KT, Kim YK, Lee JS. Prediction of residual disease of spine infection using F-18 FDG PET/CT. Spine (Phila Pa 1976). 2009;34(22):2424–30.
Lee IS, Lee JS, Kim SJ, Jun S, Suh KT. Fluorine-18-fluorodeoxyglucose positron emission tomography/computed tomography imaging in pyogenic and tuberculous spondylitis: preliminary study. J Comput Assist Tomogr. 2009;33(4):587–92.
Hartmann A, Eid K, Dora C, Trentz O, von Schulthess GK, Stumpe KDM. Diagnostic value of 18F-FDG PET/CT in trauma patients with suspected chronic osteomyelitis. Eur J Nucl Med Mol Imaging. 2007;34(5):704–14.
Treglia G, Sadeghi R. Meta-analyses and systematic reviews on PET and PET/CT in oncology: the state of the art. Clin Transl Imaging. 2013;1(2):73–5.
Townsend DW. Dual-modality imaging: combining anatomy and function. J Nucl Med. 2008;49(6):938–55.
Boellaard R, Delgado-Bolton R, Oyen WJ, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42(2):328–54.
Sathekge MM, Ankrah AO, Lawal I, Vorster M. Monitoring response to therapy. Semin Nucl Med. 2018 Mar;48(2):166–81.
Sollini M, Berchiolli R, Kirienko M, Rossi A, Glaudemans AWJM, Slart R, et al. PET/MRI in infection and inflammation. Semin Nucl Med. 2018;48(3):225–41.
Fahnert J, Purz S, Jarvers JS, Heyde CE, Barthel H, Stumpp P, et al. Use of simultaneous 18F-FDG PET/MRI for the detection of spondylodiskitis. J Nucl Med. 2016;57(9):1396–401.
Xu T, Chen Y. Research progress of [(68)Ga]citrate PET’s utility in infection and inflammation imaging: a review. Mol Imaging Biol. 2019. https://doi.org/10.1007/s11307-019-01366-x.
Nanni C, Errani C, Boriani L, Fantini L, Ambrosini V, Boschi S, et al. 68Ga-citrate PET/CT for evaluating patients with infections of the bone: preliminary results. J Nucl Med. 2010;51(12):1932–6.
Treglia G. Diagnostic performance of (18)F-FDG PET/CT in infectious and inflammatory diseases according to published meta-analyses. Contrast Media Mol Imaging. 2019;2019:3018349.
Acknowledgements
This work was carried out in collaboration with the Clinical Trial Unit of Ente Ospedaliero Cantonale [CTU-EOC] (Ticino, Switzerland). We are grateful to the staff of the Clinical Trial Unit of Ente Ospedaliero Cantonale for their invaluable statistical support.
Funding
This systematic review and meta-analysis was funded by the European Association of Nuclear Medicine (EANM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any study with human participants or animals performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Infection and Inflammation
Rights and permissions
About this article
Cite this article
Treglia, G., Pascale, M., Lazzeri, E. et al. Diagnostic performance of 18F-FDG PET/CT in patients with spinal infection: a systematic review and a bivariate meta-analysis. Eur J Nucl Med Mol Imaging 47, 1287–1301 (2020). https://doi.org/10.1007/s00259-019-04571-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-019-04571-6