Abstract
Purpose
This is a prospective non-randomized observation study done on 33 patients with uncomplicated spinal tuberculosis to observe the imaging characteristics on sequential F-18 FDG PET CT scans.
Methods
33 consecutive patients with pathologically proven spinal tuberculosis underwent a baseline contrast-enhanced whole body FDG PET scan before initiation of antitubercular therapy, 6 and 12 months and at 18 months or the end of antitubercular therapy.
Result
The baseline peak SUVmax of lesions in our 33 cases had values ranging from 5.9 to 30.3 (mean 14.8). 63.6 % patients had clinically occult non-contiguous multifocal skeletal involvement at the time of the baseline whole body PET CT scanning. The mean change in SUVmax at various time points was highly significant (p value < 0.001).
Conclusion
SUVmax can be taken as a reliable marker for serial quantification of metabolic activity in spinal tuberculosis. This may translate into a potential role for FDG as an imaging biomarker for noninvasive response evaluation in skeletal tuberculosis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tuberculosis of the spine is one of the most important extrapulmonary forms of tuberculosis, both in terms of relative frequency and the substantial potential for permanent disability. It has been estimated that spinal tuberculosis accounts for about 15 % of the cases of extrapulmonary tuberculosis and 2 % of all cases of tuberculosis. More than half of all osteoarticular manifestations of tuberculosis in India affect the spine [1].
The diagnosis of spinal tuberculosis is challenging. Clinical presentation is often vague and delayed due to the rather insidious onset of symptoms and slow disease progression. Early diagnosis and institution of early chemotherapy is imperative to prevent deformity and morbidity, A confident radiological diagnosis in spinal tuberculosis is however made in less than half of the cases of spinal tuberculosis. Pathological confirmation is also challenging due to the paucibacillary nature of the disease [2].
Controversies also exist regarding the management of spinal tuberculosis. While it is reasonably approved that outpatient chemotherapy with standard antitubercular drugs should be the primary management of uncomplicated spinal tuberculosis, the optimum duration of treatment remains controversial. The challenge remains in defining an accurate radiological end point to stop treatment [3].
Active tubercular lesions often exhibit a high degree of F18-fluorodeoxyglucose (F-18 FDG) uptake. Activated inflammatory cells like neutrophils, macrophages and lymphocytes show increased F-18 FDG uptake. The intensity of radiotracer uptake depends upon the grade of inflammatory activity [4]. The evolution of radiotracer uptake, thus, can be used to measure the efficacy of medical treatment, permitting either a better modulation of drug dosage or a radical modification of therapeutic strategy. FDG PET CT may thus find its place in the clinical setting and play a significant role in determining the end point in the termination of antitubercular therapy (ATT) in skeletal tuberculosis [5].
This prospective study was an attempt to determine whether F-18 fluoro-deoxyglucose positron emission tomography CT (F-18 FDG PET CT) could be used as a response evaluation tool during the treatment of uncomplicated spinal tuberculosis. The aim was to determine the metabolic and imaging characteristics of the lesions of spinal tuberculosis at presentation, to track the metabolic changes in the lesions during the course of therapy and to observe if the changes in FDG uptake correlated with the accepted clinical markers of response evaluation.
Materials and methods
Trial design
This was a non-randomized prospective observational trial conducted between April 2009 and June 2013 at the Sir Ganga Ram Hospital, New Delhi. A clearance was taken from the hospital ethics committee before conducting the trial.
Thirty-three consecutive patients who presented to the Department of Orthopedics with a radiologically suspect and pathologically proven diagnosis of skeletal tuberculosis were included in the study. All trial patients had to be more than 18 years of age. Patients already on ATT for more than 1 week or treatment failure cases, cases of proven multidrug resistant TB, uncontrolled diabetes mellitus, pregnancy, known concomitant malignancy, immuno-compromised state or concomitant chronic illness were excluded from the study.
All patients underwent basic blood investigations which included an assessment of complete blood counts and erythrocyte sedimentation rate (ESR). All patients underwent a whole body FDG PET CT scan before initiation of ATT, at 6 and 12 months during the course of treatment and at 18 months or the end of ATT. All scans were done on the dedicated PET CT scanner (discovery STE with 16 slice CT system from GE). A standard protocol was used for the PET CT scan with F-18 FDG injected at a dose of 0.15 mCi/Kg body weight and the scan performed after waiting for 60 min. Intravenous contrast material was administered for the contrast enhanced CT scan, which was done as part of the PET CT scan. A standardized uptake value (SUV) max was calculated, corrected for patient body weight by drawing a spherical ROI of 1.5 cm diameter over the most metabolically active part of the tumor. An attempt was made to include both the involved bone and soft tissue as much as possible.
The demographic data, clinical and treatment history, general and systemic examination findings, laboratory parameters and relevant radiological imaging findings of all the patients were recorded systematically in a predetermined format.
Pathology
All patients included in the trial underwent a procedure to pathologically prove the diagnosis of tuberculosis. An image guided percutaneous aspiration and biopsy from at least one radiologically evident lesion was performed in all the cases at presentation before the initiation of ATT. The identification of acid-fast bacilli on the aspirate smears or the presence of granulomas with necrosis/caseation was considered presumed proof for active tuberculosis. The aspirates were also cultured using Lowenstein Jensen (LJ) media in a few patient samples and reported 6 weeks later. Mycobacterium tuberculi was cultured in 15 of the 27 cultures.
Treatment
All patients underwent standard ATT which included of rifampicin(R)/INH (H)/pyrazinamide(Z)/ethambutol(E) for 4 months followed by RHE for 4 months and RH for next 4 months.
Statistical analysis
Data was entered and analyzed in SPSS version 12. Patients were divided into groups according to the length of follow-up. Descriptive statistics was used to summarize the clinical and demographic profiles of all the patients. Wilcoxon signed rank test, a non-parametric test was used to compare the mean change in SUVmax level at various points of follow-up from baseline to 6, 12, 18, 6 to 12, 6 to 18 and 12 to 18 months. Further, the correlation between percentage change in mean SUVmax at different time points with percentage change in clinical response indicators viz. ESR, eastern co-operative oncology group (ECOG) score and visual analog scale (VAS) pain score was measured using spearman’s rank correlation test. p values <0.05 were considered to be statistically significant.
Results
Clinical data
Of the 33 patients enrolled , 14 males (42 %) and 19 females (58 %); with mean age of 41 years; range 22–81 years comprised the patient sample for this study. The chief presenting complaint was of back pain (100 %). The mean duration of pain was 1.8 months. Weight loss and fever were the other common complaints at presentation.
, 14 males (42 %) and 19 females (58 %); with mean age of 41 years; range 22–81 years comprised the patient sample for this study. The chief presenting complaint was of back pain (100 %). The mean duration of pain was 1.8 months. Weight loss and fever were the other common complaints at presentation.
In the study group, the commonest site of pain  at initial presentation was in the dorsal region of spine (36.4 %), followed by dorso-lumbar region (15.2 %). The VAS pain score at the time of presentation for all study population was between 6 and 9, with maximum patients presenting with VAS score of 8 (36.4 %) and fewest with a score of 7 (18.2 %).
at initial presentation was in the dorsal region of spine (36.4 %), followed by dorso-lumbar region (15.2 %). The VAS pain score at the time of presentation for all study population was between 6 and 9, with maximum patients presenting with VAS score of 8 (36.4 %) and fewest with a score of 7 (18.2 %).
We calculated the significance of mean fall in VAS pain score for each of these groups. For all the six time points compared, the fall in VAS score was found to be highly significant (p value = 0.001).
After 6 months of therapy, 19 of 30 patients were ambulatory and capable of self-care. 9 of 30 (30 %) patients who had a baseline ECOG score of 4, reported very little improvement in their disability with an ECOG score of 3 and restricted physical activity due to disease.
All 25 patients (100 %) reported improvement in extent of physical disability and quality of life after 12 months of commencement of ATT with 6 of 25 patients (24 %) reporting an improvement in scores by a maximum of three points. At 12 months of therapy, all patients were reported to be at least ambulatory and capable of self-care.
At 18 months of therapy, more than half (55.6 %) patients reported their physical state to be comparable to pre disease status and rest 44.4 % (n = 8) reported that they could resume office and carry out routine activity. No patient reported any restriction in routine physical activity or worsening after 18 months of completion of ATT.
Imaging data
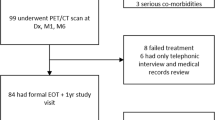
Thirty-three patients enrolled in the baseline clinical and imaging study, 30 patients (90.9 %) presented for follow-up at 6 months, 25 patients were followed up at 12 months post commencement of ATT and 18 patients were assessed at 18 months post ATT (Table 1). The ESR, ECOG scores, VAS pain scores and image findings of each patient were recorded. The attrition in sample size on follow-up at 18 months was partly due to loss of patient to follow-up with improvement of clinical condition (n = 7; 21 %) and due to cessation of ATT at 12 months of treatment (n = 8; 24 %) following clinical improvement and radiological evidence of complete resolution of disease.
The mean change in SUVmax at various time points from baseline to 6, 12, 18, 6 to 12, 6 to 18 and 12 to 18 months were calculated using the Wilcoxon signed rank test and were found to be highly significant (p value <0.001).
The baseline peak SUVmax of lesions as observed in our 33 cases had values ranging from 5.9 to 30.3 (mean 14.79; range 24.4). 21 of 33 (63.63 %) patients were also found to have clinically occult non-contiguous multifocal skeletal involvement at the time of detection on whole body PET CT scanning (Table 2).
Correlation between markers
Between baseline and 6 months, no significant correlation was seen between change in mean SUVmax and ESR (p = 0.207). However, a significant correlation was seen between fall in SUV with change in VAS score (p = 0.04).
On comparing baseline to 12 months, changes in SUVmax showed significant correlation with change in VAS score (p = 0.04). Again no correlation was seen between change in SUVmax over 12 months and change in ESR (p = 0.79).
From baseline to 18 months of therapy, similarly, spearman’s rank correlation test showed no significant correlation between change in mean SUVmax with either change in ESR (p = 0.489) or VAS score (p = 0.245) (Table 3).
Discussion
This prospective study assessed the imaging characteristics of known cases of skeletal tuberculosis on FDG PET CT scans and studied its role in response evaluation to ATT.
Though the uptake of F-18 FDG is not specific for tuberculosis, activated inflammatory cells like neutrophils, macrophages and lymphocytes demonstrate increased F-18 FDG uptake, causing significant tracer accumulation in inflammatory and infectious processes. Studies have shown that active tuberculous lesions often exhibit a high degree of FDG uptake, though this can vary, depending upon the grade of inflammatory activity [4].
This variability of FDG uptake in tuberculosis, as quantified by standard uptake values also reflects in our observations. The lowest SUVmax observed in any lesion among our 33 cases was recorded to be 5.9 while the highest recorded SUVmax was 30.3, with a wide range of 24.4 (standard deviation 6.2) thus, making it impossible for us to predict reliably any cut off value for characterizing the inflammatory lesions by the means of semiquantitative analysis of FDG uptake.
Non-contiguous multifocal tuberculous spondylitis is rare with most studies demonstrating a prevalence of less than 10 % in study populations [7, 8]. In our study however, we found that 21 of 33 (63.63 %) patients had occult non-contiguous multifocal skeletal involvement at the time of detection using whole body PET CT scanning. The significantly higher prevalence reported in our series as compared to various studies reported in literature can be explained by the fact that most of the other studies used regional imaging, and accounted only for occult non-contiguous spinal involvement, thus underestimating the true prevalence. Also the other studies used conventional radiography and MRI as the modality of screening as compared to FDG PET CT scans. The higher sensitivity of FDG PET CT for detecting lesions, often when associated with very subtle radiological features may also be a reason for the higher occult lesion detection rate in our study. However, our findings may be overestimated due to the small sample size of our study and merits validation in larger sample size studies.
Monitoring response to treatment in skeletal tuberculosis
In our study, we were able to consistently demonstrate a statistically significant change in SUVmax on FDG PET imaging during the course of ATT (Figs. 1, 2). This signifies that SUVmax can be taken as a reliable marker for serial quantification of metabolic activity in an inflammatory disease process like tuberculosis. This may translate into a potential role for FDG as an imaging biomarker for noninvasive response evaluation in skeletal tuberculosis. Further FDG PET may be able to identify the non-responders early in the course of treatment, thus reducing the lag period in the diagnosis of multidrug resistance and its associated morbidity.
Further, PET-CT imaging may also allow us to monitor the pharmacodynamics of antitubercular drugs in real time, significantly reducing drug development time for newer drugs.
Since we followed up our patients only for duration of about 2 years in this study, further long-term follow-up is recommended to observe the relapse rates in patients showing metabolic response on PET-guided therapy.
Conclusions
Metabolic activity as studied on FDG PET CT can be taken as a reliable marker for serial quantification of activity in an inflammatory disease process like tuberculosis. The changes in glycolytic activity within the inflammatory lesion as measured by FDG uptake correlates well with the clinical markers of response and possibly provide more objective evidence of response rather than the non-specific biochemical markers such as ESR. This may translate into a potential clinical role for FDG as an imaging biomarker for noninvasive response evaluation in skeletal tuberculosis and for guiding modulation of therapy. Further, FDG PET can also serve as a useful tool for early detection of multidrug resistance, thus significantly reducing lag period in diagnosis and its associated morbidity.
References
Cormican L, Hammal R, Messenger J, Milburn HJ (2006) Current difficulties in the diagnosis and management of spinal tuberculosis. Postgrad Med J 82(963):46–51
Ramachandran S, Clifton IJ, Collyns TA, Watson JP, Pearson SB (2006) The treatment of spinal tuberculosis: a retrospective study. Int J Tuberc Lung Dis 23:186–189
American Thoracic Society Centers for Disease Control and Prevention, Infectious Diseases Society of America (2003) Treatment of tuberculosis. Am J Respir Crit Care Med 167:603–662
Harkirat S, Anand SS, Indrajit IK, Dash AK, Pictorial essay (2008) PET/CT in tuberculosis. Indian J Radiol Imaging 18:141–147
Davis SL, Nuermberger EL, Um PK, Vidal C, Jedynak B, Pomper MG (2009) Noninvasive pulmonary [18F]-2-fluoro-deoxy-d-glucose positron emission tomography correlates with bactericidal activity of tuberculosis drug treatment. Antimicrob Agents Chemother 53(11):4879–4884
Dass B, Puet TA, Watanakunakor C (2002) Tuberculosis of the spine (Pott’s disease) presenting as ‘compression fractures’. Spinal Cord 40:604–608. doi:10.1038/sj.sc.3101365
Turgut M (2001) Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. a survey study on 694 patients. Neurosurg Rev 24:8–13. doi:10.1007/PL00011973
Nussbaum ES, Rockwold GL, Bergman TA, Erickson DL, Seljeskog EL (1995) Spinal tuberculosis: a diagnostic and management challenge. J Neurosurg 83:243–247
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dureja, S., Sen, I.B. & Acharya, S. Potential role of F18 FDG PET-CT as an imaging biomarker for the noninvasive evaluation in uncomplicated skeletal tuberculosis: a prospective clinical observational study. Eur Spine J 23, 2449–2454 (2014). https://doi.org/10.1007/s00586-014-3483-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-014-3483-8