Abstract
Purpose
In recent years, several [18F]-labeled amyloid-PET tracers have been developed and have obtained clinical approval. Despite their widespread scientific use, studies in routine clinical settings are limited. We therefore investigated the impact of [18F]-florbetaben (FBB)-PET on the diagnostic management of patients with suspected dementia that was still unclarified after [18F]-fluordeoxyglucose (FDG)-PET.
Methods
All subjects were referred in-house with a suspected dementia syndrome due to neurodegenerative disease. After undergoing an FDG-PET exam, the cases were discussed by the interdisciplinary dementia board, where the most likely diagnosis as well as potential differential diagnoses were documented. Because of persistent diagnostic uncertainty, the patients received an additional FBB-PET exam. Results were interpreted visually and classified as amyloid-positive or amyloid-negative, and we then compared the individual clinical diagnoses before and after additional FBB-PET.
Results
A total of 107 patients (mean age 69.4 ± 9.7y) were included in the study. The FBB-PET was rated as amyloid-positive in 65/107. In 83% of the formerly unclear cases, a final diagnosis was reached through FBB-PET, and the most likely prior diagnosis was changed in 28% of cases. The highest impact was observed for distinguishing Alzheimer’s dementia (AD) from fronto-temporal dementia (FTLD), where FBB-PET altered the most likely diagnosis in 41% of cases.
Conclusions
FBB-PET has a high additive value in establishing a final diagnosis in suspected dementia cases when prior investigations such as FDG-PET are inconclusive. The differentiation between AD and FTLD was particularly facilitated by amyloid-PET, predicting a considerable impact on patient management, especially in the light of upcoming disease-modifying therapies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is the most prevalent form of neurodegenerative dementia, and is consequently imposing an onerous burden on health care systems in societies with aging populations [1]. Intracellular neurofibrillary tangles and extracellular amyloid plaques comprise the hallmark neuropathologies of AD [2]. Recently developed amyloid-PET radiotracers such as [18F]-florbetaben (FBB) possess proven sensitivity to detect brain amyloid pathology in vivo [3], as confirmed by subsequent autopsy studies [4]. Current considerations recommend biomarker-based classification schemes for AD, with amyloid-PET being an integral component [5].
Criteria for appropriate use of amyloid imaging have been defined to include three groups of patients in whom the biomarker evidence should be most relevant [6]: (1) early (below 65 years of age) onset of progressive dementia; (2) atypical or mixed presentation of AD; and (3) persistent or progressive unexplained mild cognitive impairment. Importantly, the results of amyloid-PET imaging bring added value in clinical management of individual patients [7]. In this regard, advanced age hampers the value of amyloid-PET, as positivity is present in more than 40% of cognitively healthy subjects older than 90 years [8].
Despite widespread use in scientific investigations, the application of amyloid-PET in clinical routine settings has remained limited [7]. However, amyloid-PET is poised to complement more established AD biomarkers, such as structural magnetic resonance imaging (MRI) [9], [18F]-fluorodeoxyglucose (FDG)-PET [10], and protein concentrations of cerebrospinal fluid (CSF) [11].
The aim of this study was to assess the additive diagnostic value of FBB-PET in a clinical setting. To this end, we extended the hitherto established algorithm of differential diagnosis of dementia at our center to include the option of amyloid-PET when the battery of prior multi-modal assessments had proven insufficient for differential diagnosis. We intended to evaluate the impact of additional amyloid-PET on the diagnosis in previously ambiguous cases.
Methods
Study design and patient enrollment
All subjects were recruited at the University of Munich, Department of Neurology, Department of Psychiatry, and Institute for Stroke and Dementia Research, respectively, and were scanned in a clinical routine setting at the Department of Nuclear Medicine between 2012 and 2015. After undergoing cognitive testing, MRI, CSF sampling and FDG-PET examinations, the cases were discussed by the interdisciplinary dementia board, which recommended an additional amyloid-PET for cases with remaining uncertainty in the final diagnosis. We selected 107 patients with mild cognitive impairment or dementia for additional amyloid-PET, and recorded their most likely diagnosis according to ICD-10 and common diagnostic criteria [12,13,14,15] as well as potential differential diagnoses prior to FBB-PET. The FBB-PET recordings were interpreted visually and classified as amyloid-positive or -negative, and diagnoses were compared before and after FBB-PET.
Clinical assessments, MRI and CSF
All patients received a clinical neurological examination and neuropsychological testing consisting of the Mini-Mental-State Examination (MMSE) and optional CERAD plus battery that includes Trail Making Test A and B as well as verbal fluency tests. Years of education were recorded, and laboratory parameters for metabolic causes of dementia (vitamin B12, thiamine and folate levels, and thyroid, and liver function) were assessed. MRI was performed with 1.5 and 3.0 Tesla magnets, using at least a T1w sequence for atrophy assessment and a T2w-FLAIR sequence for screening of leukoencephalopathy. Lumbar CSF was collected for assessment of phosphorylated tau (threshold: p-tau, <61 pg/ml), total tau (threshold: <450 pg/ml) and Aβ42 (threshold: >450 pg/ml).
PET imaging
Radiosynthesis
Radiosynthesis of FBB was performed as described previously [16], employing an automated synthesis module (Modular-Lab Standard, Eckert & Ziegler, Berlin, Germany). Averaged radiochemical purity was >99% and specific activity was 7.3 × 105 ± 3.4 × 105 GBq mmol−1. FDG was purchased commercially.
FDG PET acquisition
FDG-PET images were acquired on a GE Discovery 690 PET/CT scanner or a Siemens ECAT EXACT HR+ PET scanner. All patients had fasted for at least 6 h, and had a maximum plasma glucose level of 150 mg/dl at the time of scanning. A dose of 140 ± 7 MBq FDG was injected intravenously as the patients rested in a room with dimmed light and low noise level. Static emission frames of 5 min each were acquired from 30 to 45 min p.i. on the GE Discovery 690 PET/CT, or from 30 to 60 min p.i. on the Siemens ECAT EXACT HR+ PET scanner. A low-dose CT scan or a transmission scan with external 68Ge-source performed prior to the static acquisition was used for attenuation correction. PET data were reconstructed iteratively (GE Discovery 690 PET/CT) or with filtered-back-projection (Siemens ECAT EXACT HR+ PET).
FBB-PET acquisition
FBB-PET images were acquired in 3-D mode exclusively on a GE Discovery 690 PET/CT scanner. After intravenous injection of 300 ± 5 MBq FBB static emission recordings were generated as four frames of 5 min each extending from 90 to 110 min p.i. [17]. After inspection for movement, the frames were summed. A low-dose CT scan was performed prior to the static acquisition for attenuation correction of the PET recordings. PET data were reconstructed iteratively.
Image analysis
Visual analysis of FDG PET
For image interpretation of the FDG-PET images, three-dimensional stereotactic surface projections (3D-SSP) [18] were generated using the software Neurostat (Department of Radiology, University of Washington, Seattle, WA, USA). A senior expert visually assessed the 3-D-SSP images depicted as tracer uptake and Z-score maps against reference images from age-matched healthy controls. The reader had access to clinical information (available in all cases) and MRI imaging. FDG-PET was rated for either the presence of a neurodegenerative metabolism pattern, an intermediate likelihood group of probable synaptic dysfunction, or the absence of a neurodegenerative metabolism pattern (+ / o / -). Based on an anatomic pattern of hypometabolism, the evaluation of FDG-PET was categorized as the most likely of the following diagnoses: AD, FTLD or non-AD/non-FTLD.
Visual analysis of FBB-PET
The FBB images were visually assessed by three independent experts, who were aware of the ongoing study. Patients with significantly increased cortical FBB uptake in at least one target region were judged as amyloid-positive according to common diagnostic criteria [19]. Conflicting results between readers were resolved by consensus. Scans were definitively interpreted immediately after imaging and the final read was provided to the clinician at that time.
Statistical analysis
Normality of data distribution was assessed by the Kolmogorov-Smirnov test. The nonparametric χ2 test was used to test for significantly differing probability of categorical dichotomous (amyloid-PET read-out, final clinical diagnosis, diagnosis change, gender), trichotomous (neurodegeneration likelihood of FDG-PET) and four item (clinical categorization after FDG-PET) variates among subgroups. MMSE as an ordinal variate was compared by the Mann-Whitney test between subgroups, and age as the only metric variate was compared by a Students t-test. A significance level of p < 0.05 for rejection of the null hypothesis was applied in all analyses, whereas p < 0.1 was defined as a trend. All statistical tests were performed using SPSS (version 23.0, IBM, Chicago, IL).
Results
Demographics
A total of 107 subjects (48% male) were included in the study (Table 1). The mean age was 69.4 years (SD 9.7). MRI was available from 84 patients and revealed moderate to severe leukoencephalopathy in 40/84 (48%) cases and significant brain atrophy in 47/84 (56%) cases. CSF was obtained from 65 patients with pathological alterations of total tau (34/65, 52%), p-tau (37/65, 57%), and Aβ42 (21/65, 32%). Patients who were not evaluated by MRI or CSF had contraindications or refused the examination. All patients underwent FDG-PET.
Initially suspected diagnoses before FDG-PET in the 47 subjects with mild cognitive impairment (MCI) were AD (N = 22), depression (N = 3), vascular dementia (N = 2), and MCI not specified (N = 20). In the 60 demented subjects, the diagnoses were AD (N = 23), FTLD (N = 12), vascular dementia (N = 1), depression (N = 2), Parkinsonian syndrome (N = 1), multiple system atrophy type C (N = 1), thiamine-deficient encephalopathy (N = 1), and dementia not specified (N = 19).
FDG-PET findings
The rate of neurodegeneration-typical patterns in FDG-PET was higher in demented subjects when compared to MCI (χ 2 = 11.2, p = 0.004; Table 2), but the proportion of neurodegenerative FDG-PET patterns did not differ between the AD and non-AD subgroups of MCI patients (χ 2 = 0.5, p = 0.772). Among the subgroups of demented patients, we observed a trend towards higher frequency of neurodegenerative FDG-PET patterns in suspected FTLD patients (11/12 cases; χ 2 = 9.5, p = 0.051).
Reasons for recommending Amyloid-PET by the dementia board
Patient groups were categorized according to the rationale which led to an additional amyloid-PET, as judged by the interdisciplinary dementia board after FDG-PET. Five constellations were observed in this regard: (1) In 29/107 (27%) cases with manifest synaptic dysfunction to FDG-PET, the differential diagnosis between AD and FTLD was unclear; (2) Prodromal synaptic dysfunction, especially in the posterior cingulate cortex, was observed in 30/107 (28%) cases and FBB-PET was intended to confirm suspected AD; and (3) 24/107 (22%) cases mostly presented with low or AD-atypical synaptic dysfunction, but with clinical uncertainty regarding the underlying AD-pathology. In these subjects, FBB-PET was recommended to exclude amyloid pathology; (4) AD-like patterns of hypometabolism together with negative CSF levels for Aβ1-42 were observed in 7/107 (7%) patients, for whom FBB was recommended to elucidate a possible amyloid pathology biomarker mismatch; and (5) Possible AD-like synaptic dysfunction but atypical clinical presentation for AD was found in 17/107 (16%) patients, for who FBB-PET was intended to confirm suspected AD. As expected, the proportions of severity of hypometabolism within the neurodegenerative metabolism patterns differed significantly between recommendation subgroups (χ 2 = 59.2, p < 0.001, Fig. 1a), as did the most likely diagnostic classification after FDG-PET (χ2 = 64.4, p < 0.001, Fig. 1b).
Synaptic dysfunction and diagnostic categorization in different categories with recommendation of additional amyloid-PET. a Bar graph showing the proportions of likelihood of neurodegeneration (N+ = present; No = intermediate; N- = absent) within subgroups in which additional amyloid-PET was recommended by the interdisciplinary dementia board. b Bar graph indicating the proportions of clinical severity (MCI = mild cognitive impaired; DEM = demented) divided for favored AD and pooled non-AD diagnosis
Amyloid-PET findings and consecutive diagnoses
The mean (± SD) time period between FBB and FDG-PET was 2.7 (± 3.4) months. Of all subjects, 65/107 (61%) were visually classified as amyloid-positive (40% male; mean age 69.2 ± 9.5 y), 42/107 (39%) as amyloid-negative (59% male; mean age 69.6 ± 10.1 y, Table 3). Cognitive performance was lower in amyloid-positive patients (∆: −2.1 MMSE points, Mann-Whitney: p = 0.011), who had a higher frequency of female gender when compared to amyloid-negative patients (χ 2 = 3.9, p = 0.038). Amyloid positivity was present in all cases with recommendation due to negative CSF levels for Aβ1-42 (100%, χ 2 = 4.8, p = 0.027 versus remaining cases), and significantly lower in the sub-group for whom amyloid-PET was intended to rule out AD pathology (21%, χ 2 = 20.7, p < 0.001 versus remaining cases).
In 89/107 (83%) cases, a final diagnosis was reached after FBB-PET. A positive amyloid read led to a final diagnosis in 61/65 (94%) patients. In contrast, a negative amyloid read resulted in a final diagnosis in only 28/42 (67%) of the cases (χ 2 = 13.5, p < 0.001, Table 3. Low and intermediate likelihood of neurodegeneration in FDG-PET tended to be associated with persistently lacking a diagnosis even after FBB-PET when compared against high likelihood of neurodegeneration (χ 2 = 4.6, p = 0.101).
FBB-PET proved to be efficient in providing a final diagnosis, especially in cases in which it was desired to distinguish AD from FTLD (final diagnosis in 28/29; 97%; see Figs. 2 and 3 for illustrative cases), a rate which was significantly higher when compared to the pooled remaining subjects (χ 2 = 5.1, p = 0.018). The small group of patients with negative Aβ1-42 values in CSF received a final diagnosis in 7/7 (100%) of cases (χ 2 = 0.7, p = 0.650). Subjects with prodromal synaptic dysfunction to FDG-PET (χ 2 = 1.3, p = 0.199; see Fig. 4 for illustrative cases) obtained a final diagnosis after FBB-PET in 23/30 (77%) of cases, and those with atypical clinical presentation (χ 2 = 1.5, p = 0.264) obtained a final diagnosis in 13/17 (77%) cases. The lowest rate of established final diagnosis was observed in cases with intention to exclude AD (18/24, 75%; χ 2 = 1.5, p = 0.180; see Fig. 5 for illustrative cases).
Differential diagnosis of FTLD vs. frontal variant of AD: 3-dimensional stereotactic surface projection (3DSSP) FDG images and axial gray-scale FBB-PET images of a 63-year-old female patient (a) and a 66-year-old male patient (b). Both patients presented with FTLD-like hypometabolic patterns in FDG-PET, but with minor involvement of parietal cortex. In patient a, a final diagnosis of FTLD was established based on the negative FBB-PET. In patient b, the positive FBB-PET led to an AD diagnosis. Normalized count rates (upper rows, max: Z-score 5) and Z-maps for FDG (lower rows, max: Z-score 5). Projections: R LAT: right lateral, L LAT: left lateral, SUP: superior, INF: inferior, ANT: anterior, POST: posterior, R MED: right medial, L MED: left medial
Differential diagnosis of PPA: 3-D stereotactic surface projection (3DSSP) FDG images and axial gray-scale FBB-PET images of a 59-year-old female patient (a) and a 59-year-old male patient (b), both clinically presenting with PPA (unclassified). Both patients showed FTLD-like hypometabolic patterns in FDG-PET. Patient a received a final diagnosis of lvPPA due to AD, based on amyloid-positive FBB-PET. Patient b received a final diagnosis of svPPA due to FTLD, based on amyloid-negative FBB-PET. Normalized count (upper rows, max: Z-score 5) and Z-maps for FDG (lower rows, max: Z-score 5). Projections: R LAT: right lateral, L LAT: left lateral, SUP: superior, INF: inferior, ANT: anterior, POST: posterior, R MED: right medial, L MED: left medial
Clarification of prodromal synaptic dysfunction in MCI: 3-D stereotactic surface projection (3DSSP) FDG-PET images and axial gray-scale FBB-PET images of a 73-year-old female subject (a) and a 77-year-old female subject (b). Both patients presented with moderate hypometabolism in the posterior cingulate cortex (PCC) to FDG-PET, leading to the most likely diagnosis of AD. In subject a, the positive FBB-PET led to the final diagnosis of AD, while in subject b no final diagnosis could be reached after the negative FBB-PET. Normalized count (upper rows, max: Z-score 5) and Z-maps for FDG (lower rows, max: Z-score 5). Projections: R LAT: right lateral, L LAT: left lateral, SUP: superior, INF: inferior, ANT: anterior, POST: posterior, R MED: right medial, L MED: left medial
Differential diagnosis of vascular dementia vs. mixed dementia: Axial MRI T2 FLAIR sequence images, 3-D stereotactic surface projection (3DSSP) FDG-PET images and axial gray-scale FBB-PET images of a 78-year-old female subject (a) and a 77-year-old female subject (b), both presented with MCI, leukoencephalopathy in MRI and diffuse hypometabolic patterns in FDG-PET. For both patients, the most likely diagnosis of vascular dementia was favored after FDG-PET. Patient a received a final diagnosis of vascular dementia after the negative FBB-PET. Patient b received a final diagnosis of mixed dementia (AD + vascular dementia) after the positive FBB-PET. Normalized count (upper rows, max: Z-score 5) and Z-maps for FDG (lower rows, max: Z-score 5). Projections: R LAT: right lateral, L LAT: left lateral, SUP: superior, INF: inferior, ANT: anterior, POST: posterior, R MED: right medial, L MED: left medial
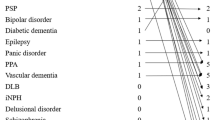
Change of prior diagnosis after FBB-PET
In 30/107 (28%) of all cases, the most likely prior diagnosis after FDG-PET was changed due to the FBB-PET results. A negative amyloid status tended to be associated with a higher rate of diagnosis change (16/42, 38%; χ 2 = 3.5, p = 0.051) when compared to amyloid-positive subjects (14/65, 22%). Considering the rationale for additional amyloid-PET recommendation subgroups described above, the impact of FBB-PET on altering the most likely prior diagnosis varied, with the highest rate of change for the AD vs. FTLD differential diagnosis subgroup (12/29, 41% change of diagnosis, Table 3), which tended towards significance in contrast with pooled other cases (χ 2 = 3.5, p = 0.054). Atypical clinical presentation and negative Aβ1-42 values in CSF had trends towards lower rate of changes in diagnosis when compared to the remaining subjects. The likelihood of neurodegeneration in FDG-PET did not predict changes in diagnosis due to additional FBB-PET (χ 2 = 1.3, p = 0.513).
Discussion
In this observational study using FBB in a clinical routine setting, we found a relevant additive value of amyloid imaging for resolving diagnoses in unclear dementia cases. These tertiary dementia care cases were selected by an interdisciplinary board informed by results of clinical examination, cognitive testing, MRI imaging, CSF analysis and FDG-PET. Amyloid-PET enabled a final diagnosis in >80% of the formerly unclear cases, and the initially favored differential diagnoses changed in nearly a third of the patients. Highest diagnostic impact was observed in the subgroup requiring differential diagnosis between AD and FTLD, in whom amyloid-PET changed >40% of the previously favored diagnoses.
Our data indicated that addition of amyloid PET changed the prior favored diagnosis in 28% of all subjects. This is in line with findings of another single-center study in 57 patients in which the authors found a percentage of 23% diagnosis reclassifications with [11C]-PiB amyloid PET [20]. Our findings of significantly higher rate of revised diagnoses among amyloid-negative, as compared to amyloid-positive subjects, are in congruence with data of a recent multi-center investigation evaluating amyloid deposition with [18F]-florbetapir in 228 patients [21]. One multi-center investigation found even higher rates of revised diagnoses (55%) when investigating 229 patients with progressive cognitive decline by [18F]-florbetapir [22]. However, others observed that additional [11C]-PiB PET brought an overall change of baseline diagnosis of only 9% when examining 140 patients with dual FDG- and amyloid-PET in an academic dementia center [23]. The considerable variability of the rates of revised diagnoses between the different studies is most likely related to the comprehensiveness of clinical evaluation prior to amyloid-PET. This is such as it is known that the added biomarker value increases diametrically with the clinical experience [7]. Also, our preselection of complex patients with inconclusive assessments including FDG-PET probably favored a higher percentage of diagnosis changes. The current study design emphasizes the added value of amyloid imaging for clinical diagnosis even after assessment of synaptic dysfunction by FDG-PET, which is itself known to have considerable influence on clinical diagnosis of AD [24]. Of interest, we have recently argued that early-phase amyloid-PET, as a surrogate marker of perfusion, has the potential to substitute for FDG-PET insofar as two channels of information (amyloid and neurodegeneration) can be obtained from one examination [25, 26]. In light of the current data, it is likely that patients with complex differential diagnosis of AD versus FTLD would potentially benefit most from this approach.
Subgroup findings in this study allowed conclusions about the particular value of amyloid-PET in different clinical conditions. This is of key importance, as limited tracer availability, high costs, and continuing absence of any curative treatment option currently make it necessary to triage patients for amyloid-PET. Here, we found the highest impact for differential diagnosis between AD and FTLD, where a final diagnosis was established in 28/29 (97%) of the cases. Most significantly, the diagnosis favored prior to addition of amyloid-PET changed in 12/29 (41%) of all patients in that subgroup. In contrast, an earlier study found high sensitivity and specificity for differentiation between AD and FTLD by sole FDG-PET when using stereotactic surface projections for visual interpretation, as in the present study [27]. In this context, selection by the interdisciplinary dementia board biased the present study towards complex or ambiguous patients, such that patients enrolled for amyloid-PET likely do not represent a population-based composition of straightforward AD and FTLD patients. However, this group composition consolidates the current findings in this subgroup, as amyloid-PET enabled a clinical diagnosis in nearly all of those challenging cases. This was especially relevant in frontal variants of AD and in FTLD with coexisting parietal hypometabolism (Fig. 2).
Our sample included nine patients with a post-amyloid PET diagnosis of primary progressive aphasia (PPA; “AD vs. FTLD” and “Rule out AD” subgroups). Of these, three were amyloid-positive and six were amyloid-negative. It has been proposed that different proportions of underlying neuropathology can support the clinical classification of PPA subtypes [15], and findings of a recent review indicated amyloid positivity of 13% for semantic variant PPA (svPPA) and 85% for logopenic variant PPA (lvPPA) [28]. In line with that distribution, all amyloid-positive PPA cases of the current study were clinically diagnosed as lvPPA whereas all amyloid-negative cases were clinically diagnosed as svPPA [29]. Two PPA cases were initially difficult to classify, but primarily suspected to be svPPA with underlying FTLD neuropathology. In both of these cases, diagnosis was revised through positive amyloid-PET (one case illustrated in Fig. 3). These case observations clearly substantiate the impact of amyloid imaging on differential dementia diagnosis such as that of PPA variants.
In a clinical routine setting, borderline findings of prodromal synaptic dysfunction in FDG-PET are inadequate as biomarker information and do not support a life-changing dementia disease diagnosis. Although there is population group-based evidence predicting conversion from MCI to AD when synaptic dysfunction is present in the posterior cingulate cortex [30], the diagnosis of AD in individual cases is often uncertain, especially when other causes (e.g., leukoencephalopathy) for cognitive decline co-exist with cerebrometabolic changes. Our data fully reflect this dilemma, as 9/30 cases with AD-typical distribution of synaptic dysfunction were amyloid-negative, even though their synaptic dysfunction pattern did not differ from that of the amyloid-positive subjects of the same subgroup (Fig. 4).
Convincing evidence that amyloid-negative PET rules out progressive AD pathology in vivo has already been presented for FBB [4]. The high negative predictive value of amyloid-PET scans primarily result from the cortical Aβ deposition builtup already early in the disease course, which makes AD very unlikely in case of amyloid-negativity. Indeed, a negative amyloid scan was present in 77% of our AD exclusion group. Four patients in this subgroup were still lacking a final diagnosis after negative amyloid-PET, as their mild cognitive impairment could not be definitively attributed, given the absent amyloid pathology. These four patients had contraindication for MRI, which might well have revealed a microvascular component (or leukencephalopathy) of their cognitive impairment, given that they all presented with cardiovascular risk factors. Two cases illustrated in Fig. 5 presented with leukoencephalopathy in MRI and moderate synaptic dysfunction to FDG-PET, but only one was identified as suffering from mixed dementia with additional underlying AD pathology.
Seven patients who had moderate-to-high likelihood for AD after FDG-PET but with negative CSF findings (normal Aβ42) were without exception rated as amyloid-positive. Similar discrepancies between molecular imaging and CSF biomarkers of amyloid pathology have been reported elsewhere [31, 32]. As an example, a recent study found a discordance of 25% between the two biomarkers [33], which fits well with our present data. It must be considered that CSF results may differ between laboratories, and a proportion of patients refuse CSF collection or have contraindication such as anticoagulation treatment.
Most of the patients in the subgroup with atypical clinical presentation of AD had a distinct hypometabolism in temporal or occipital cortices that exceeded the metabolic effect in classical AD regions like the posterior cingulate cortex or the parietal cortex. These results are in line with previous findings of congruence between FDG-PET and the phenotype [34]. A high frequency of amyloid-positive scans was observed in this subgroup, with confirmed AD pathology in most cases (85%). Although two out of eight cases with suspected PCA were amyloid-negative, this did not impact the final diagnosis. In contrast, two previous investigations found amyloid-positivity without exception in PCA samples [35, 36]. However, another study that focused on amyloid imaging with [11C]-PiB in patients with atypical clinical AD presentation likewise identified two out of five PCA cases as amyloid-negative [34]. In summary, amyloid-PET did not bring a change in diagnosis in this entire subgroup. However, we consider the use of amyloid PET as relevant for future anti-amyloid treatment options also in case of PCA.
We note a limitation of this study in that we did not attain scores for confidence in pre- and post-amyloid-PET diagnosis, but rather focused on the establishment of a final diagnosis after amyloid imaging. Thus, more detailed analyses of diagnostic certainty could not be performed. However, establishment of a final diagnosis via FBB-PET in cases which remain unclear after FDG-PET is a rather strong indicator of the added value of amyloid-PET.
Conclusion
FBB-PET has a high additive value in establishing a final diagnosis in cases with suspected dementia disorders when FDG-PET remains inconclusive. Differential diagnosis between AD and FTLD most prominently profited from additional amyloid-PET. Future work should address the question of whether this incremental value of FBB-PET translates into improved patient management, especially in light of upcoming disease-modifying therapies.
References
Ziegler-Graham K, Brookmeyer R, Johnson E, Arrighi HM. Worldwide variation in the doubling time of Alzheimer's disease incidence rates. Alzheimers Dement. 2008;4:316–23. https://doi.org/10.1016/j.jalz.2008.05.2479.
Braak H, Braak E. Neuropathological stageing of Alzheimer-related changes. Acta Neuropathol. 1991;82:239–59.
Barthel H, Sabri O. Florbetaben to trace amyloid-beta in the Alzheimer brain by means of PET. J Alzheimers Dis. 2011;26(Suppl 3):117–21. https://doi.org/10.3233/JAD-2011-0068.
Sabri O, Sabbagh MN, Seibyl J, Barthel H, Akatsu H, Ouchi Y, et al. Florbetaben PET imaging to detect amyloid beta plaques in Alzheimer's disease: phase 3 study. Alzheimers Dement. 2015;11:964–74. https://doi.org/10.1016/j.jalz.2015.02.004.
Jack CR Jr, Bennett DA, Blennow K, Carrillo MC, Feldman HH, Frisoni GB, et al. A/T/N: an unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87:539–47. https://doi.org/10.1212/WNL.0000000000002923.
Johnson KA, Minoshima S, Bohnen NI, Donohoe KJ, Foster NL, Herscovitch P, et al. Appropriate use criteria for amyloid PET: a report of the Amyloid imaging task force, the Society of Nuclear Medicine and Molecular Imaging, and the Alzheimer's Association. Alzheimers Dement. 2013;9:e-1-16. https://doi.org/10.1016/j.jalz.2013.01.002.
Vandenberghe R, Adamczuk K, Dupont P, Laere KV, Chetelat G. Amyloid PET in clinical practice: its place in the multidimensional space of Alzheimer's disease. Neuroimage Clin. 2013;2:497–511. https://doi.org/10.1016/j.nicl.2013.03.014.
Jansen WJ, Ossenkoppele R, Knol DL, Tijms BM, Scheltens P, Verhey FR, et al. Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA. 2015;313:1924–38. https://doi.org/10.1001/jama.2015.4668.
Dickerson BC, Bakkour A, Salat DH, Feczko E, Pacheco J, Greve DN, et al. The cortical signature of Alzheimer's disease: regionally specific cortical thinning relates to symptom severity in very mild to mild AD dementia and is detectable in asymptomatic amyloid-positive individuals. Cereb Cortex. 2009;19:497–510. https://doi.org/10.1093/cercor/bhn113.
Mosconi L, Tsui WH, Herholz K, Pupi A, Drzezga A, Lucignani G, et al. Multicenter standardized 18F-FDG PET diagnosis of mild cognitive impairment, Alzheimer's disease, and other dementias. J Nucl Med. 2008;49:390–8. https://doi.org/10.2967/jnumed.107.045385.
Bartlett JW, Frost C, Mattsson N, Skillback T, Blennow K, Zetterberg H, et al. Determining cut-points for Alzheimer's disease biomarkers: statistical issues, methods and challenges. Biomark Med. 2012;6:391–400. https://doi.org/10.2217/bmm.12.49.
Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P, et al. Revising the definition of Alzheimer's disease: a new lexicon. Lancet Neurol. 2010;9:1118–27. https://doi.org/10.1016/S1474-4422(10)70223-4.
Petersen RC. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183–94. https://doi.org/10.1111/j.1365-2796.2004.01388.x.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–77. https://doi.org/10.1093/brain/awr179.
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14. https://doi.org/10.1212/WNL.0b013e31821103e6.
Patt M, Schildan A, Barthel H, Schultze-Mosgau MH, Rohde B, Reininger C, et al. Metabolite analysis of [18F]Florbetaben (BAY 94-9172) in human subjects: a substudy within a proof of mechanism clinical trial. J Radioanal Nucl Chem. 2010;284:557–62.
Barthel H, Gertz HJ, Dresel S, Peters O, Bartenstein P, Buerger K, et al. Cerebral amyloid-beta PET with florbetaben (18F) in patients with Alzheimer's disease and healthy controls: a multicentre phase 2 diagnostic study. Lancet Neurol. 2011;10:424–35. https://doi.org/10.1016/S1474-4422(11)70077-1.
Minoshima S, Frey KA, Koeppe RA, Foster NL, Kuhl DE. A diagnostic approach in Alzheimer's disease using three-dimensional stereotactic surface projections of fluorine-18-FDG PET. J Nucl Med: Off Publ Soc Nucl Med. 1995;36:1238–48.
Minoshima S, Drzezga AE, Barthel H, Bohnen N, Djekidel M, Lewis DH, et al. SNMMI procedure standard/EANM practice guideline for Amyloid PET imaging of the brain 1.0. J Nucl Med. 2016;57:1316–22. https://doi.org/10.2967/jnumed.116.174615.
Frederiksen KS, Hasselbalch SG, Hejl AM, Law I, Hojgaard L, Waldemar G. Added diagnostic value of (11)C-PiB-PET in memory clinic patients with uncertain diagnosis. Dement Geriatr Cogn Dis Extra. 2012;2:610–21. https://doi.org/10.1159/000345783.
Boccardi M, Altomare D, Ferrari C, Festari C, Guerra UP, Paghera B, et al. Assessment of the incremental diagnostic value of Florbetapir F 18 imaging in patients with cognitive impairment: the incremental diagnostic value of Amyloid PET with [18F]-Florbetapir (INDIA-FBP) study. JAMA Neurol. 2016; https://doi.org/10.1001/jamaneurol.2016.3751.
Grundman M, Pontecorvo MJ, Salloway SP, Doraiswamy PM, Fleisher AS, Sadowsky CH, et al. Potential impact of amyloid imaging on diagnosis and intended management in patients with progressive cognitive decline. Alzheimer Dis Assoc Disord. 2013;27:4–15. https://doi.org/10.1097/WAD.0b013e318279d02a.
Sanchez-Juan P, Ghosh PM, Hagen J, Gesierich B, Henry M, Grinberg LT, et al. Practical utility of amyloid and FDG-PET in an academic dementia center. Neurology. 2014;82:230–8. https://doi.org/10.1212/WNL.0000000000000032.
Mosconi L, Berti V, Glodzik L, Pupi A, De Santi S, de Leon MJ. Pre-clinical detection of Alzheimer's disease using FDG-PET, with or without amyloid imaging. J Alzheimers Dis. 2010;20:843–54. https://doi.org/10.3233/JAD-2010-091504.
Daerr S, Brendel M, Zach C, Mille E, Schilling D, Zacherl MJ, et al. Evaluation of early-phase [18F]-florbetaben PET acquisition in clinical routine cases. NeuroImage Clin. 2017;14:77–86. https://doi.org/10.1016/j.nicl.2016.10.005.
Tiepolt S, Hesse S, Patt M, Luthardt J, Schroeter ML, Hoffmann KT, et al. Early [(18)F]florbetaben and [(11)C]PiB PET images are a surrogate biomarker of neuronal injury in Alzheimer's disease. Eur J Nucl Med Mol Imaging. 2016;43:1700–9. https://doi.org/10.1007/s00259-016-3353-1.
Foster NL, Heidebrink JL, Clark CM, Jagust WJ, Arnold SE, Barbas NR, et al. FDG-PET improves accuracy in distinguishing frontotemporal dementia and Alzheimer's disease. Brain : J Neurol. 2007;130:2616–35. https://doi.org/10.1093/brain/awm177.
Villarejo-Galende A, Llamas-Velasco S, Gomez-Grande A, Puertas-Martin V, Contador I, Sarandeses P, et al. Amyloid pet in primary progressive aphasia: case series and systematic review of the literature. J Neurol. 2016; https://doi.org/10.1007/s00415-016-8324-8.
Krishnan K, Machulda MM, Whitwell JL, Butts AM, Duffy JR, Strand EA, et al. Varying degrees of Temporoparietal Hypometabolism on FDG-PET reveal Amyloid-positive Logopenic primary progressive aphasia is not a homogeneous clinical entity. J Alzheimers Dis. 2016; https://doi.org/10.3233/JAD-160614.
Drzezga A, Lautenschlager N, Siebner H, Riemenschneider M, Willoch F, Minoshima S, et al. Cerebral metabolic changes accompanying conversion of mild cognitive impairment into Alzheimer's disease: a PET follow-up study. Eur J Nucl Med Mol Imaging. 2003;30:1104–13. https://doi.org/10.1007/s00259-003-1194-1.
Alexopoulos P, Kriett L, Haller B, Klupp E, Gray K, Grimmer T, et al. Limited agreement between biomarkers of neuronal injury at different stages of Alzheimer's disease. Alzheimers Dement. 2014;10:684–9. https://doi.org/10.1016/j.jalz.2014.03.006.
Schonecker S, Brendel M, Huber M, Vollmar C, Huppertz HJ, Teipel S, et al. Applied multimodal diagnostics in a case of presenile dementia. BMC Neurol. 2016;16:131. https://doi.org/10.1186/s12883-016-0647-7.
Lewczuk P, Matzen A, Blennow K, Parnetti L, Molinuevo JL, Eusebi P, et al. Cerebrospinal fluid Abeta42/40 corresponds better than Abeta42 to Amyloid PET in Alzheimer's disease. J Alzheimers Dis. 2016;55:813–22. https://doi.org/10.3233/JAD-160722.
Wolk DA, Price JC, Madeira C, Saxton JA, Snitz BE, Lopez OL, et al. Amyloid imaging in dementias with atypical presentation. Alzheimers Dement. 2012;8:389–98. https://doi.org/10.1016/j.jalz.2011.07.003.
Singh TD, Josephs KA, Machulda MM, Drubach DA, Apostolova LG, Lowe VJ, et al. Clinical, FDG and amyloid PET imaging in posterior cortical atrophy. J Neurol. 2015;262:1483–92. https://doi.org/10.1007/s00415-015-7732-5.
Whitwell J, Graff-Radford J, Singh T, Drubach D, Senjem M, Spychalla A, et al. 18F-FDG PET in posterior cortical atrophy and dementia with Lewy bodies. J Nucl Med: Off Publ Soc Nucl Med. 2016; https://doi.org/10.2967/jnumed.116.179903.
Acknowledgements
Parts of this paper originated from the doctoral thesis of Jonas Schnabel and Eva Brendel. Florbetaben precursor was kindly provided by Piramal Imaging and partial financial support rested on philanthropic donations to the Department of Neurology (Adrian Danek). We note editing of the manuscript by Inglewood Biomedical Editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MB, JS, SS, LW, EB, JMW, MU, AS, MP, CP, NA, CC, OP, JL, KB have nothing to disclose. AD received speaker honoraria from GE Healthcare. PB received speaker honoraria from Siemens and GE Healthcare. HB and OS received speaker honoraria and travel expenses from Piramal Imaging. AR received speaker honoraria from Piramal Imaging and GE Healthcare.
Ethical approval
All procedures described in the study were in accordance with the ethical standards of the Institutional Review Board and with the 1964 Helsinki Declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Brendel, M., Schnabel, J., Schönecker, S. et al. Additive value of amyloid-PET in routine cases of clinical dementia work-up after FDG-PET. Eur J Nucl Med Mol Imaging 44, 2239–2248 (2017). https://doi.org/10.1007/s00259-017-3832-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3832-z